A Selective Anterior Obturator Nerve Block for Total Hip Arthroplasty
Adam W. Meier DO, Minhe Kim MD
Affiliation
Department of Anesthesiology, Virginia Mason Medical Center, Seattle, WA
Corresponding Author
Stanley Yuan, MD, Department of Anesthesiology, Virginia Mason Medical Center, 1100 9th Ave., B2-AN, Seattle, WA 98101, Tel: (206) 223-6980, Fax: (206) 223-6982, E-mail: stanley.yuan@virginiamason.org
Citation
Yuan, S., et al. A Selective Anterior Obturator Nerve Block for Total Hip Arthroplasty. (2017) J Anesth Surg 4(1): 45- 46.
Copy rights
© 2017 Yuan, S. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Obturator Nerve Block; Hip Arthroplasty; Postoperative analgesia
Introduction
Case Description
An 83 year-old male with history of hypertension, complete heart block with a pacemaker, ankylosing spondylitis, prostate cancer, obesity and obstructive sleep apnea was scheduled for a right total hip arthroplasty (THA) for degenerative hip disease. His daily analgesic medications included oxycodone 5 milligrams (mg) every 3 hours, gabapentin 600 mg nightly, acetaminophen 650 mg every 6 hours and meloxicam 15 mg daily. A focused airway examination revealed a Mallampati III oropharyngeal exam, thyromental distance less than 6 centimeters, limited mouth opening and limited jaw protrusion. After a lengthy discussion regarding his anesthetic options, the patient elected for general endotracheal anesthesia and agreed to an obturator nerve block in the recovery room if postoperative analgesia proved difficult. The patient had taken his nightly dose of gabapentin and morning dose of acetaminophen prior to hospital arrival. In the preoperative area, he was given celecoxib 200 mg in addition as part of a comprehensive preoperative multimodal therapy.
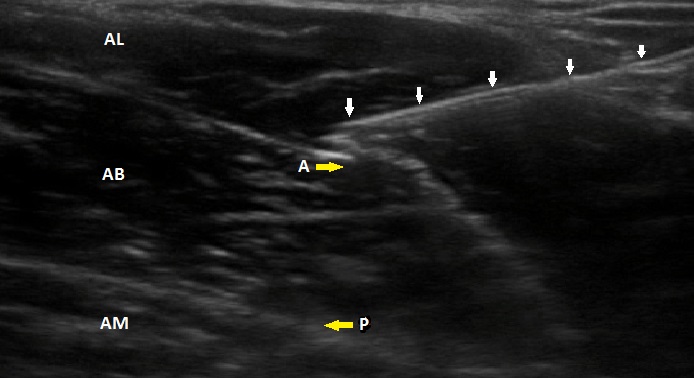
The patient was taken to the operating room where general anesthesia was induced with fentanyl 25 micrograms (mcg), propofol and succinyl choline intravenously (IV) and an endotracheal tube was placed without complication. General anesthesia was maintained with sevoflurane and a total of hydromorphone 0.8 mg IV. After successful completion of the surgery, the patient reported a pain numerical rating score (NRS) of 7/10 for generalized right hip pain upon arriving in the post anesthesia care unit (PACU). He was noted to have increased spasticity and pain with manipulation of the hip. The patient agreed to proceed with the previously consented postoperative obturator nerve block. He remained in the supine position with approximately 15 degrees of hip abduction. Skin cleansing of the medial proximal thigh and inguinal area was performed with 2% chlorhexidine and 70% isopropyl alcohol (Chloraprep). A selected obturator nerve block was performed with in-plane ultrasound-guided technique (Sonosite, M-Turbo, 6 to 15 MHz, Bothell, WA) with a 21G needle (Sonoplex). A 20-milliliter (mL) bolus of 0.5% ropivacaine was injected between the adductor longus and adductor brevis muscles to anesthetize the anterior division of the obturator nerve (Figure 1). Twenty minutes after block completion, the patient was re-evaluated. His NRS scores had decreased to 4/10 and he had significant improvement of mobility of his right hip. No opioid was given in the PACU. He was able to tolerate hip flexion and rotation without increased pain. Furthermore, hip adductions appear grossly equal bilaterally.
The patient was transferred to an inpatient orthopedics floor for continued postoperative care and rehabilitation. Scheduled acetaminophen 650 every 6 hours and gabapentin 600 mg nightly was ordered. His NRS scores remained at 4/10 and required no additional opioid medication. At 11 hours post obturator nerve block, the patient received his first oral opioid dose of oxycodone 15 mg for an NRS of 6/10. On postoperative day (POD) 1, he received two additional doses of oxycodone 15 mg, along with his scheduled acetaminophen, meloxicam 15 mg and gabapentin daily. The patient successfully participated in postoperative rehabilitation and met all performance goals on POD 1.
Discussion
This case illustrates two important points regarding the management of postoperative analgesia status post THA. A selective obturator nerve block can provide improved post-operative analgesia after THA without compromising lower extremity strength for early ambulation and rehabilitation.
The obturator nerve is derived from lumbar nerve roots and descends to the obturator foramen which subsequently divides into the anterior and posterior branches. The anterior branch, which runs between the adductor longus, adductor brevis and pectineus muscles (Figure 1), gives off an articular branch that enters the femoro acetabular joint through the acetabular notch. The anterior branch also gives off muscular branches to the adductor longus and brevis muscles. The posterior branch runs between the adductor brevis and adductor magnus and provide innervations to these muscle groups; there is also a branch to knee joint and cutaneous over the medial aspect of the thigh. Cruveilhier[1] was the first to describe that a branch of the obturator nerve provides a significant contribution to the hip joint. Since then, our understanding of the hip joint sensory innervation has been unchanged over the years[2].
Figure 1: Depicts a selective anterior branch of the obturator nerve with needle approaching in lateral to medial direction.
AL: adductor longus; AB: adductor brevis; AM: adductor magnus; A: anterior branch of obturator nerve; P: posteroir branch of obturator nerve; White arrows; block needle
We specifically targeted the anterior branch of the obturator nerve for coverage of the anteromedial hip capsule, yet without compromising the much of the lower extremity strength. By selectively targeting the anterior branch, the patient was able to ambulate and participate in rehabilitation without perceived gross muscle weakness. While a combined block of femoral, femoral cutaneous, and sciatic nerves may provide better analgesic effect. But doing so, it will also result in a significant lower extremity weakness. The risk of fall with femoral nerve blocks (FNBs) has been cited as high as seven percent[3,4] but Memtsoudis et al.[5] argued that this association may not completely be anesthesia related. Inpatient falls are categorized as “never events” by the Center for Medicare and Medicaid Services, which cost on average of $4000 per incident and are usually not reimbursed by Medicare[6,7].
Opioid medications can contribute to postoperative delirium, ileus, nausea and respiratory depression. The use of opioids is particularly concerns in the obese and elderly population because they are more prone to cognitive impairment, risk of fall, and respiratory depression[8]. Our patient did not require any postoperative opioid medication for the initial eleven hours following the obturator nerve block. He was able to participate in full rehabilitation and discharged from the hospital without any complications. Elderly and obese patients may benefit even more from the opioid-sparing effects of an obturator nerve block after total hip arthroplasty compared to their counter parts.
Conclusion
In conclusion, this case illustrates a selective anterior branch of the obturator nerve block may provide adequate postoperative analgesia for THA. Further study may compare the analgesic and motor-sparing benefits of this block undergoing hip surgery.
References
- 1. Cruveilhier, J. The anatomy of the human body. The first american from the last Paris edition, Pattison, G.S., ed. (1844) Harper and Bros New Year.
Pubmed || Crossref || Others - 2. Birnbaum, K., Prescher, A., Hessler, S., et al. The sensory innervation of the hip joint--an anatomical study. (1997) Surg Radiol Anat 19(6): 371-375.
Pubmed || Crossref || Others - 3. Ilfeld, B.M., Duke, K.B., Donohue, M.C. The association between lower extremity continuous peripheral nerve blocks and patient falls after knee and hip arthroplasty. (2010) Anesth Analg 111(6): 1552-1554.
Pubmed || Crossref || Others - 4. Atkinson, H.D., Hamid, I., Gupte, C.M., et al. Postoperative fall after the use of the 3-in-1 femoral nerve block for knee surgery: a report of four cases. (2008) J Orthop Surg 16(3): 381-384.
Pubmed || Crossref || Others - 5. Memtsoudis, S.G., Danninger, T., Rasul, R., et al. Inpatient falls after total knee arthroplasty: the role of anesthesia type and peripheral nerve blocks. (2014) Anesthesiology 120(3): 551-563.
Pubmed || Crossref || Others - 6. 6. Cui, Q., Schapiro, L.H., Kinney, M.C., et al. Reducing costly falls of total knee replacement patients. (2013) Am J Med Qual 28: 335-338.
Pubmed || Crossref || Others - 7. Inouye, S.K., Brown , C.J., Tinetti, M.E. Medicare nonpayment, hospital falls, and unintended consequences. (2009) N Engl J Med 360(23): 2390-2393.
Pubmed || Crossref || Others - 8. Solomon, D.H., Rassen, J.A., Glynn, R.J., et al. The comparative safety of opioids for nonmalignant pain in older adults. (2010) Arch Intern Med 170(22): 1979-1986.
Pubmed || Crossref || Others