Aseptic Necrosis of hysterorrafia. Case Report
Illia, R1*, Cabrera, M2, Valencia, V2, Lobenstein, G3, Uranga Imaz, M3, Manrique, G3, Fiameni, F3
Affiliation
- 1Chief of Obstetrics Service, Hospital Alemán, Buenos Aires, Argentina
- 2Obstetric Service, Hospital Alemán, Buenos Aires, Argentina
- 3Staffmembers, Obstetrics Service, Hospital Alemán, Buenos Aires, Argentina
Corresponding Author
Ricardo Illia, MD, Department of Obstetrics and Pediatrics, Buenos Aires University, Fellow ACOG Buenos Aires Argentine Section, Chief of Obstetrics Service, Hospital Alemán, Avenida Pueyrredón - 1640, Buenos Aires - 1118, Argentina, Tel: +54 11 4827-7000; Fax: +54 11 4827-7000; E-mail: rhillia@gmail.com
Citation
Illia, R., et al. Aseptic Necrosis of Hysterorrafia. Case Report. (2017) J Gynecol Neonatal Biol 3(1): 5-7.
Copy rights
© 2017 Illia, R. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Aseptic necrosis hysterorrafia; Postpartum bleeding; Uterine plastic.
Abstract
Background: The Aseptic Necrosis of Hysterorrafia (ANH) is an uncommon cause of late puerperal bleeding in cases of posts Cesarean Section (CS) often iterative. The bleeding does not decrease with the classic treatments and start at any moment and stop at any moment too. It can be serious enough to affect the patient health. In the past, the usual resolution was the total or partial hysterectomy.
Case: A 35 years old patient with uncontrollable metrorragia post cesarean section treated with surgical conservative technique.
Conclusion: Not all cases of ANH need a Hysterectomy as a definitive treatment. A conservative approach could be successful.
Introduction
Aseptic necrosis of hysterorrafia was described more than 80 years ago as a bleeding syndrome that occur after CS mainly when they are repeated. Apparently, in some of the CS, the accidental occlusion of one of uterine arteries could produce an infarct of the myometrium at the angle of the hysterography, and as a consequence, the bleeding appears at the same time as myometrial necrosis start, sometimes scarce and sometimes heavy, affecting the mother´s health. The bleeding does not decrease with conventional treatments, and stop spontaneously, as it started again at any time and an unexpected time[1-3]. It is red blood, rutilant, abundant, without any pain. The known measures to stop bleeding in puerperium do not work in this case, neither drugs nor surgical treatments. We have found several articles about the measures to stop uterine bleeding[4-6] in postpartum emergencies, but none of them refers to uterine necrosis.
Case
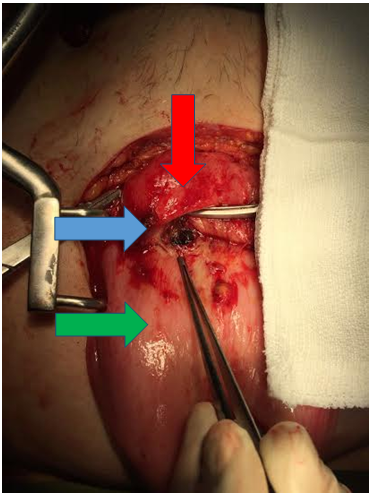
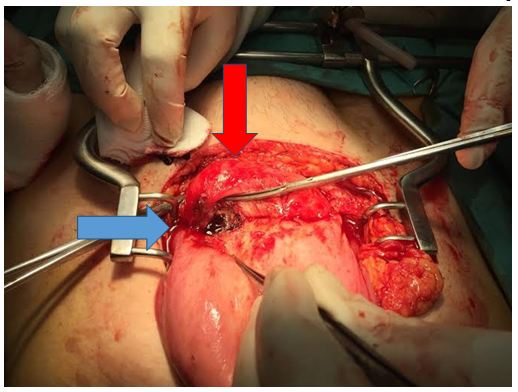
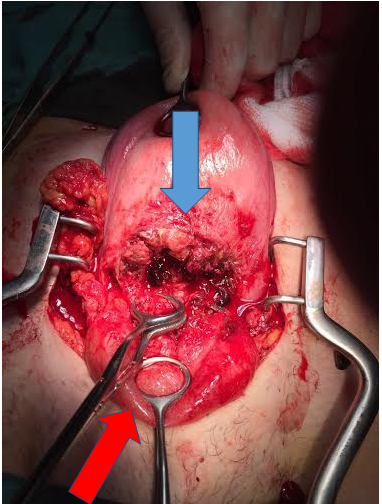
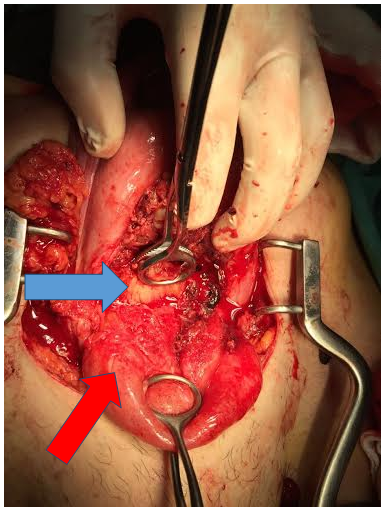
A 35 years old patient underwent to second CS because a previous CS. The surgery was uneventful and she was discharged from Hospital 72 hours after surgery in a good state. About 10 days later, she came to the Emergency Department because she presented vaginal bleeding, not had seen any damage of neither vagina nor cervix at first examination. It was a metrorrhagia. She started with nasal oxytocin every 6 hours and apparently she did well. Without bleedings he was discharged to home with the explanation to on a rush consultation if bleeding reappears. One week later, she came again for the same symptoms and was medicated in the same way. One more time, she was discharged without bleeding and negative ultrasound. But, some days later, she came again, and we started to think in the possibility of ANH. Weper formed blood tests and found a hematocrit of 28%, she was asymptomatic, and the ultrasound this time informed a cystic image over the hysterorrafia with a size of 10 cm long and 5 cm wide. With this finding, we decided to perform a relaparotomy with presuntive diagnosis of ANH, haematoma or abscess. Noteworthy, we left the bladder well down in the vesicouterine space by the time of CS because we did not performed peritonization of the hysterorrafia. When we opened the abdomen, we have seen the bladder over the hysterorrafia (Figure 1) and when we started to separate and descend the bladder from the uterus, we found the necrotic process (Figure 1- 2). The bladder was descended and then ecrotic process was bigger (Figure 2-3). We removed the necrotic tissue and rebuild the hysterorrafia with separated stitches with catgut (Figure 4-5-6). With a good uterine retraction and good homeostasis, we closed the abdomen. The patient did well and was discharged 48 hours after surgery and she remain a symptomatic for more than a six month. She does not re assumed still her menses because she continue breast feeding her baby. Weper formed a monthly ultrasound control and all the images were normal during the follow up and the patient is a symptomatic without any urinary dysfunction.
Figure 1: We can observe the uterus (green arrow), the bladder occluding the hysterorrafia (red arrow) and the necrotic area (blue arrow).
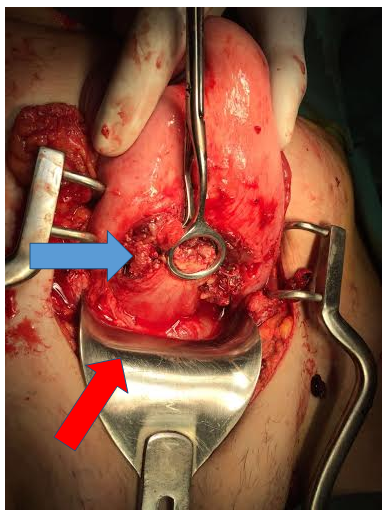
Figure 2: We descended the bladder (red arrow) and the necrosis was bigger (blue arrow).
Figure 3: The bladder libered from the hysterorrafia (red arrow) and then ecrotic area in the uterus (blue arrow).
Figure 4: Observe the bladder moved down (red arrow) and the liberation of the inferior lip of the hysterorrafia (blue arrow).
Figure 5: The bladder completely descended (red arrow) and the uterus ready to be repaired (blue arrow).
Figure 6: The repaired uterus.
Discussion
ANH is an entity described long time ago, and the usual treatment was the hysterectomy. We presented a case solved by conservative surgery, allowing the normal gynecology cal evolution and perhaps a new future pregnancy. Some authors have commented in unpublished discussions that the origin of the problem is an anomalous vascular supply of the uterus. But, none of them have performed an arteriogram before pregnancy to support this argument against the presence of neovascularization for the necrosis and inflammatory process. According Lofrumento et al. study[1], myometrial wound healing could be related with phenotype and genotype of the patient and would involve several cytokines to create the scar. In our search of articles related with the subject of our case in Pub Med and Up to Date.
We found only the article of Jae-Hyun Kwon[2] about a patient who developed uterine necrosis, but it was a twin pregnancy previously embolized. We did not find articles about specifically post cesarean section uterine scar necrosis. So, we continue sustaining the old description about the origin of ANH and propose that the treatment should be conservative instead to remove the uterus.
References
- 1. Lofrumento, D.D., Di Nardo, M.A., De Falco, M., et al. Uterine wound healing: A complex process mediated by protein and peptides. (2016) Current Protein Pept Sci.
- 2. Kwon, J.H. Uterine necrosis and hysterectomy in a postpartum hemorrhage patient who underwent repeated uterine artery embolization. (2015) Taiwan J Obstet Gynecol 54(6): 791-792.
- 3. Kaya, B., Guralp, O., Tuten, A., et al. Which uterine sparing technique should be used for uterine atony during cesarean section? The Bakri balloon or the B-Lynch suture?. (2016) Arch Gynecol Obstet 294(3): 511-517.
- 4. Kaya, B., Tuten, A., Daglar, K., et al. B-Lynch uterine compression sutures in the conservative surgical management of uterine atony. (2015) Arch Gynecol Obstet 291(5): 1005-1014.
- 5. Michael, A. Belfort. Management of postpartum hemorrhage at cesarean delivery. (2016) Literature review current through.
- 6. Younes, N. Bakri, Sabaratnam Arulkumaran. Intrauterine balloon tamponade for control of postpartum hemorrhage. (2016) Literature review current through.