Exploring Buprenorphine as a Useful Pain Management Agent
Clairmont Griffith, Bernice La France*
Affiliation
Howard University College of Medicine, Washington, DC, USA
Corresponding Author
Bernice La France, MS, MEd, SLLA, ESL, Howard University Hospital and Howard University College of Medicine, 2041 Georgia Ave. NW, Washington, D.C. 20059, Tel: (240) 565-3358; E-mail: bemore1576@gmail.com
Citation
Griffith, C et al. Exploring Buprenorphine as a Useful Pain Management Agent. (2018) J Anesth Surg 5(2): 133- 136.
Copy rights
© 2018 Griffith, C. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Abstract
The objective of this study was to assess the overall effectiveness of buprenorphine in the treatment of patients suffering from acute pain, either at their post-operative phase or due to the ongoing health issue, such as cancer and similar others. To accomplish this objective, the study followed a qualitative approach based on secondary sources accessible through digital libraries. The secondary sources used for this research included academic articles and scholarly journals, presenting empirical evidences in support or against the effectiveness of buprenorphine within the clinical setting. According to the information obtained through this study, the current data indicate insufficiency in supporting claims affirming the overall effectiveness of the medication, while it also does not refute its positive impacts in the process. In many researches, the use of buprenorphine has been examined as an alternative cure option for methadone, especially at the premise of opioid-replacement therapy that aims to reduce opioid-dependency among patients and therefore, is applied to the pain management process in an indirect manner for dual purposes. Evidences clarifying whether buprenorphine can be effective as a weak analgesic were also scarce, especially when considering the journals published on and after 2013. A lack of evidential research was also visible to assess its effective implementation among patients who are suffering from pain but are not opioid-dependent, even though the findings of most researchers suggest that the medication has been successful in opioid-dependent patients. It is thus that future studies are required to address the implications of using buprenorphine therapy in pain management.
Introduction
Buprenorphine (C29H41NO4C29H41NO4•HCl) is an opioid belonging to the class of Opiate Partial Agonists. It is commonly used to cure opioid addiction, in addition to managing acute and chronic pain[1]. Since its approval by the Food and Drug Administration (FDA) in the 1980s, it has received considerable support and acceptance from the medical field. Its rising popularity is fundamentally driven by its properties of full-agonist analgesic combined with those of partial-agonist respiratory depression[2]. Its application has however drawn many criticisms from the medical field, especially when concerning its side-effects and the fact that a few of its combinations, such as the buprenorphine/naltrexone drug formulation is yet under experimentation[3].
Methods
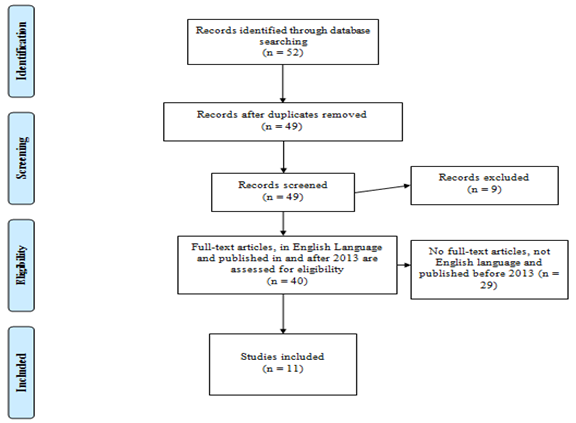
In this research, particularly, PRISMA flowchart guidelines have been followed. PRISMA flowchart involves four main steps for the selection of a source i.e. Identification, screening, eligibility, and including phases. The below figure depicts the PRISMA flowchart for this study, which shows how the sources used in the paper are selected. In this regard, 52 records are found through database searching by using the Boolean search technique. It involves combining different keywords related to the research issue using the conditions of AND, NOT and OR in order to trace and shortlist the most relevant sources of data. The different keywords used are ‘buprenorphine’, ‘pain management’, ‘effectiveness of buprenorphine’, ‘chronic pain syndrome’, ‘drawbacks of buprenorphine’, and ‘pain medication’. The corresponding step in the process involves the screening, wherein the duplicate sources are removed. In this respect, there were 3 sources that were found to be duplicate sand were removed. In this phase, all the sources are screened to select the most reliable, relevant and valid ones. Thus, considerations were provided to select those journals which were published through authenticated digital libraries. These include the Journal of the American Society of Anaesthesiologists, Pharmacy Practice Faculty Publications, Journal of Opioid Management, and National Center for Biotechnology Information of U.S. National Library of Medicine, Sage Publications, and American Journal of Pharmacy Benefits. It also involves the articles published in Journal of Pain Research, Journal of Analytical Toxicology, Annals of Emergency Medicine, Journal of Substance Abuse Treatment, JAMA Network Open, and British Journal of Anesthesia. Furthermore, the sources were examined and included in this study after ensuring that they were peer-reviewed and provided credible information regarding the effectiveness of buprenorphine in chronic pain management cases. Thus, among the total of 49 sources, 9 were excluded after screening and only the ones that have relevant information were considered for the study. The next phase is the eligibility, wherein 29 of these sources were discarded, as they did not have full-text or was published before 2013 and was in languages other than English.
Subsequently, the data analysis techniques used for this study concentrated on a thematic analysis of the obtained information from the secondary sources in alignment with the decided research objectives, which included –
Theme 1: Ways through which buprenorphine is effective in pain management
Theme 2: Effectiveness of buprenorphine in the management of chronic pain syndrome
Theme 3: Drawbacks of buprenorphine as a pain medication to be used periodically
Investigating on the basis of these three themes will assist in drawing precise conclusions as to what specific measures need to be taken in order to ensure the overall effectiveness of buprenorphine in pain management.
Results
Among all the sources collected in this paper, 11 full-texts that were reliable, relevant, and valid were eventually considered for the study. In this regard, it was found that only one of the articles has used randomized controlled trial (RCT), case report and observation method at the same time. Another article has used both RCT and observation method. Besides, two of the other sources have only used RCT method, and the remaining 8 sources have used observation method. Considerably, the information collected from these sources is analyzed in a thematic way for better understanding.
Theme 1: Ways through which buprenorphine is effective in pain management
Commonly, opioids are given to the patients either in injectable form or as an oral medication, depending on the severity of the pain they experience, which at often instances are prescribed to patients complaining about post-surgical pain. As was noted by Jirkof, (2015)[4], having the experimentation based on mice, buprenorphine application based on the typical regimen for post-surgical pain relief involves a dosage of 2 - 3 subcutaneous injections within 24-hour duration, while also being dependent on the severity and classification of the surgery. Although it remains arguable as to whether the same implications can be drawn for human patients suffering from severe post-surgical pain, researchers have provided limited or insufficient attention towards investigating the interdependency of buprenorphine effectiveness in pain management with the method of its application. Among the few texts available on this issue[5], provided crucial insights to the possibility of gaining more benefits through buprenorphine applications in pain management, but also elaborated on the drawbacks existing within past researches. According to Morgan et al. (2018)[5], the use of injectable transdermal buprenorphine has increased over time, indicating its growing preferences within the medical practitioners, as compared to sublingual or oral mucosal buprenorphine/naloxone. Similar views were also presented by Liu, et al (2015)[6] reflecting that direct injections for buprenorphine doses had greater efficacy in offering pain relief to patients.
Theme 2: Effectiveness of buprenorphine in the management of chronic pain syndrome
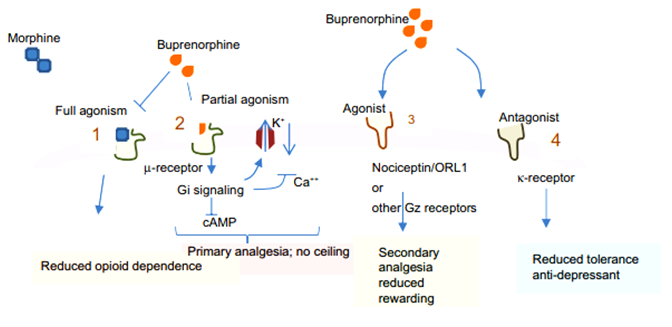
According to Khanna and Pillarisetti[7] (2015, pp. 865), the effectiveness of buprenorphine in pain management is defined by its characteristics of being “a partial agonist at µ-receptor”. The study further revealed that the formulation of buprenorphine and the generic pain model imply that the medication can be 25 to 100 times more effective than morphine; with an equipotency ratio comparison of 1:110 – 1:115 for an identical degree of analgesia. A better observation of its interactions with opioid receptors can be obtained from the diagram below:
Figure 2: Buprenorphine interactions with opioid receptors (Khanna and Pillarisetti, 2015).
Correspondingly, from the findings obtained in the study of Chen, et al. (2014)[8], it can be observed that combinations of buprenorphine with naloxone can also prove effective in treating chronic pain situations, as it allows better control on the physical qualities of the opioid to be manipulated for enhanced efficacy. As was noted by Chen et al. (2014)[8], buprenorphine-naloxone is a semi-synthetic opioid, which offers better effectiveness in pain relief in comparison with other analgesics, although it is commonly applied in the opioid replacement therapeutic process by practitioners. Similar findings were also obtained based on empirical evidences[9-11].
Theme 3: Drawbacks of buprenorphine as a pain medication to be used periodically
While addressing the limitations of buprenorphine in pain management[12] revealed that a substantial degree of clinical heterogeneity exists with regard to the use of buprenorphine. This heterogeneity is again illustrated as the function of differences pertaining to its dosage, frequency, clinical setting, and the applied administration method. Elaborating on this issue, Saloner, et al (2018)[13] asserted that recent expansion of Medicaid may have increased the frequency of prescribing buprenorphine to patients suffering from chronic pain, but its commercial availability does not show any significant correlation with the reduction in patients complaining of severe pain. It implies that the effectiveness of the medicine might be short lived. On the contrary though, Kessel, et al. (2018)[14] asserted that significant reductions have been noteworthy in the utilization frequency, costs involved and in terms of medical as well as behavioral health morbidity of buprenorphine, which offers a positive view regarding its effectiveness in pain management. Kessel et al. (2018, pp. 88)[14] further asserted that “use of induction services was associated with reduced cost and utilization of inpatient detoxification and of medical and behavioral health services”.
Discussion
Irrespective of how buprenorphine is applied, the view among clinicians can be observed as polarized. Nonetheless, medical practitioners offering treatment to patients complaining about acute pain agree with the fact almost equivocally that any treatment program is more effective when applied through a multimodal approach. This particular method is applied in the context of both regional anesthesia and non-opioid analgesics in the pain management procedure. As these traditional methods are found to assist with the substantial improvements of pain conditions within the patients, while simultaneously reducing opioid requirements among patients, it has often been accepted as an alternative to buprenorphine. Conclusively, as can be observed through the discussion above, acute pain management for patients having a relatively high degree of dependency on opioid can be a challenging and a complex issue owing to the underlying heterogeneous characteristics of the clinical setting.
Conclusion
The overall effectiveness of buprenorphine therapy in pain management process is controversial and unclear owing to the lack of adequate academic and clinical evidences to support claims made by practitioners in both favor and against its application. Nonetheless, on the basis of the evidences gathered in this research, buprenorphine can be considered as a noteworthy option to treat cases of acute pain, especially in the post-operative stages as well as in context of opioid dependence, when compared with more standard and traditional therapies, such as the use of morphine, fentanyl and oxycodone among others. The extensive degree of heterogeneity and complexity associated with the clinical setting, citing pain management requirements posits another crucial barrier to the effectiveness of buprenorphine. In particular, buprenorphine is applied in two ways, one in the sublingual manner and the other in an injectable form, having an added definable palliative effect.
References
- 1. Fiellin, D. Treatment of Acute Pain in Patients Receiving Buprenorphine/Naloxone. (2014) PCSS Guidance.
PubMed||CrossRef||Others
- 2. White, L., Hodge, A., Vlok, R., et al. Efficacy and adverse effects of buprenorphine in acute pain management: systematic review and meta-analysis of randomized controlled trials. (2018) Br J Anesth 120(4): 668-678.
- 3. D’onofrio, G., O’connor, P.G., Pantalon, M.V., et al. Emergency department–initiated buprenorphine/naloxone treatment for opioid dependence: a randomized clinical trial. (2015) JAMA 313(16): 1636-1644.
- 4. Jirkof, P., Tourvieille, A., Cinelli, P., et al. Buprenorphine for pain relief in mice: Repeated injections vs sustained-release depot formulation. (2015) Lab Anim 49(3): 177-187.
- 5. Morgan, J.R., Schackman, B.R., Leff, J.A., et al. Injectable naltrexone, oral naltrexone, and buprenorphine utilization and discontinuation among individuals treated for opioid use disorder in a United States commercially insured population. (2018) J Subst Abuse Treat 85: 90-96.
- 6. Liu, H.C., Lee, H.T., Hsu, Y.C., et al. Direct Injection LC–MS-MS Analysis of Opiates, Methamphetamine, Buprenorphine, Methadone and Their Metabolites in Oral Fluid from Substitution Therapy Patients. (2015) J Anal Toxicol 39(6): 472-480.
- 7. Khanna, I.K., Pillarisetti, S. Buprenorphine–an attractive opioid with underutilized potential in treatment of chronic pain. (2015) J Pain Res 8: 859-870.
- 8. Chen, K.Y., Lucy, C., Jianren M. Buprenorphine–naloxone therapy in pain management. (2014). Anesthesiology: J Am Society of Anesthesiol 120(5): 1262-1274.
- 9. Griffin, M.L., McDermott, K.A., McHugh, R.K., et al. Longitudinal association between pain severity and subsequent opioid use in prescription opioid dependent patients with chronic pain. (2016) Drug Alcohol Depend 163: 216-221.
- 10. Weinrib, A.Z., Burns, L.C., Mu, A., et al. A case report on the treatment of complex chronic pain and opioid dependence by a multidisciplinary transitional pain service using the ACT Matrix and buprenorphine/naloxone. (2017) J Pain Res 10: 747-755.
- 11. Donovan, K., Kogut, S., Buchanan, A.L., et al. A Claims Analysis of the Utilization of Tramadol for Acute Pain in Patients Prescribed Buprenorphine/Naloxone for Opioid Use Disorder. (2018) J Opioid Manag 1-16.
PubMed||CrossRef||Others
- 12. Love, J.S., Perrone, J., Nelson, L.S. Should Buprenorphine Be Administered to Patients with Opioid Withdrawal in the Emergency Department? (2017) Ann Emerg Med 72(1): 26-28.
- 13. Saloner, B., Levin, J., Chang, H.Y., et al. Changes in buprenorphine-naloxone and opioid pain reliever prescriptions after the Affordable Care Act Medicaid expansion. (2018) JAMA Network Open 1(4): e181588-e181588.
- 14. Kessel, J.B., Castel, L.D., Nemecek, D.A. Clinical and cost outcomes of buprenorphine treatment in a commercial benefit plan population. (2018) Am J Pharm Benefits 10(1): 84-89.
PubMed||CrossRef||Others