High prevalence of general and abdominal obesity and relationship of obesity with diabetes mellitus in patients with psychiatric disorders
Kumiko Asahi, Nobuo Imazeki, Tosei Takahashi, Mari takeuchi, Noriyo Kimura, Eriko Sasaki, Hideyuki Uchino, Kenji Murasugi, Akiko Hayakawa, Sayaka Katagiri, Noriko Ishizuka, Yoko Suzuki, Karin Sekiya, Misako Takahashi, Eiko Sato,
Affiliation
- 1Faculty of Health Care, Kiryu University, Japan
- 2Faculty of Health and Welfare, Takasaki University of Health and Welfare, Japan
- 3National Komoro-Kogen Hospital, Japan
- 4Murai Mental Hospital, Japan
- 5Niigata National Hospital, Japan
- 6Department of Periodontitis, Graduate Scool of Medical and Dental Science, Tokyo Medical and Dental University
- 7Department of Nutrition, Kyoritu Women's University, Japan
- 8Faculty of Human Nutrition, Seitoku University, Japan
Corresponding Author
Shuji Inoue, Department of Nutrition, Faculty of Health Care, Kiryu University, 606-7 Azami, Kasakake-cho, Midori-shi, Gunma 379-2392,Japan, Tel.: +81 277 48 9121; fax: +81 27748 9122; E-mails: ishuji@kiryu-u.ac.jp
Citation
Inoue, S. High Prevalence of General and Abdominal Obesity and Relationship of Obesity with Diabetes Mellitus in Patients with Psychiatric Disorders (2014) J Diabes Obes 1(2): 44- 49.
Copy rights
© 2014 Inoue, S. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Psychiatric patients; Obesity; Body mass index; Waist circumference; Diabetes mellitus
Abstract
Objective and Methods: Obesity and obesity-associated diabetes are serious health concerns in patients with psychiatric disorders. We compared the prevalence's of general obesity and abdominal obesity in 337 patients with psychiatric disorders and evaluated the risk of both types of obesity for diabetes mellitus in patients with psychiatric disorders.
Results: In patients with psychiatric disorders, the prevalence's of general obesity and abdominal obesity were very high especially in females. The prevalence of abdominal obesity was significantly higher in males than in females, and was higher than the prevalence of general obesity in all patients (total) and in males. The prevalence's of general obesity and abdominal obesity were more than 2 times high compared to those in general population. The association rate of diabetes in patients with general obesity and abdominal obesity higher than those in patients with non-general obesity and non-abdominal obesity, respectively, in total and in males and females, but these differences were not significant except in total. The values of HbA1c in patients with general obesity was significantly higher than that in patients without general obesity, in total and in males and females; but was significantly higher in patients with abdominal obesity compared to non-abdominal obese patients in total, and in females. After adjustment for several confounding factors, multiple logistic regression analysis showed significant associations of general obesity and abdominal obesity with diabetes mellitus.
Conclusions: The results of this study show that the prevalence's of general obesity and abdominal obesity in patients with psychiatric disorders is very high, especially in females which looks to be higher than those in the general population. Multiple regression analyses revealed both general and abdominal obesities were both found to be risk factors for diabetes. These results suggest that effective treatment of obesity is needed for prevention of diabetes in patients with psychiatric disorders.
Introduction
Obesity and obesity-associated diseases, including diabetes and cardiovascular disease, are important health problems in the general population. Risks for cardiovascular diseases and diabetes mellitus are increased in obese subjects[1,2], and cardiovascular disease is a major cause of death in obese patients in the general population in Western countries[3]. Patients with psychiatric disorders in Western countries also have more health problems and a much shorter life expectancy, due primarily to premature cardiovascular disease caused by obesity[4,5]. However, in Asian countries, an epidemic increase in diabetes mellitus has currently made this disease a more serious health problem than cardiovascular disease[6], particularly because Asian patients are more susceptible to diabetic microangiopathies especially nephropathy, which can lead to renal failure[7].
Patients with psychiatric disorders are more likely to suffer from obesity compared to the general population because of greater difficulties with self-management of eating habits and physical activity[8]. Several studies have examined the prevalence of general obesity (based on body mass index (BMI)) or abdominal obesity (based on waist circumference) in patients with psychiatric disorders[9-11], but a comprehensive examination of these prevalence's, together, in the same patients with psychiatric disorders has not been performed. Abdominal obesity is a stronger risk factor for lifestyle-related diseases compared to general obesity in the general Western population[12], but it is unclear whether general or abdominal obesity is more predictive of this risk in Asian countries[13]. In this study, we determined the prevalence's of general obesity and abdominal obesity, and examined whether these conditions play as risk factors for diabetes in patients with psychiatric disorders.
Materials and Methods
Subjects
The subjects were 337 outpatients with psychiatric disorders aged ≥ 20 years old who attended the Psychiatric Clinic, Komoro Kogen Hospital, Nagano, Japan. The survey period was 6 months from August 1, 2007 to August 31, 2008. Psychiatric disorders were classified using the International Classification of Disease 10th revision (ICD-10)[14] as schizophrenia (F2; N = 147, 43.6%), mood disorder (F3; N = 91, 27.0%) including bipolar affective disorder, dementia (F0; N = 44, 13.1%), neurotic disorder (F4; N = 37, 11.0%), and others (N = 18, 5.3%).
Study Protocol
Height, body weight, waist circumference (WC), and blood pressure were measured at a visit to the clinic. BMI was calculated as weight divided by the square of height (kg/m²). WC was measured at the level of the navel with a soft tape measure to determine abdominal obesity. Blood for determining HbA1c, HDL-cholesterol (HDL-C), and uric acid (UA) was collected in a fed condition at the visit because of the difficulty of requiring overnight fasting due to the psychiatric disorders of the patients.
Definitions and Criteria
General obesity was defined as BMI ≥ 25 kg/m² and abdominal obesity as WC ≥ 85 cm in males and ≥ 90 cm in females, using the criteria of the Japan Society for the Study of Obesity (JASSO)[15]. Hypertension was defined as systolic blood pressure (SBP) ≥ 140 mmHg or diastolic blood pressure (DBP) ≥ 90 mmHg or both, using the criteria in the 2009.
Japanese Society of Hypertension (JSH) Guidelines for Management of Hypertension[16]. Diabetes was defined as HbA1c (NGSP) ≥ 6.5% based on the 2013 Report of the Committee of Diabetes Classification and Diagnostic Criteria of the Japan Diabetes Society (JDS), with values of HbA1c adjusted using the National Glycohemoglobin Standardization Program[17]. HypoHDL-cholesterolemia was defined as serum HDL-C < 40 mg/dL using the 2007 Japan
Atherosclerosis Society (JAS) Guidelines for Prevention of Atherosclerotic Cardiovascular Disease[18]. Hyperuricemia was defined as serum UA > 7.0 mg/dL based on the Guidelines for Treatment of Hyperuricemia and Gout of the Japan Society of Gout and Nucleic Acid Metabolism[19]. Participants who were taking drugs for these diseases were considered to have the disease, even if laboratory values were within normal ranges.
Biochemical analysis
Concentrations of serum HDL-C and UA were determined by enzymatic methods using an autoanalyzer (TBA 2000 FR, Toshiba, Japan). HbA1c was determined by liquid chromatography (HA8170, Arkray, Japan).
Statistical analysis
Results are shown as means ± standard deviation. Patients were divided into general and non-general obesity groups or abdominal and non-abdominal obesity groups. Demographic and clinical variables were compared by unpaired Student t-test. The prevalence of obesity and the association rate of diabetes in patients with and without general obesity or with and without abdominal obesity were compared by chi-square test. Multiple logistic regression analysis was performed to determine odds ratios and 95% confidence intervals for the risk of diabetes in patients with psychiatric disorders. All analyses were performed using SPSS 15.0 and the significance level was P < 0.05.
Ethical considerations
The study complied with the Declaration of Helsinki and was approved by the institutional ethical committee of Komoro Kogen Hospital. After approval, patients who gave informed consent were included in the study.
Results
Demographic characteristics of the subjects
The demographic characteristics of the subjects are shown in Table 1. Height, body weight and UA were significantly higher in males, while age and HDL-C were significantly higher in females. WC, BMI SBP, DBR and HbA1c did not differ significantly between males and females
Table 1: Demographic characteristics of subjects
| n | Total | Male | Female |
|---|---|---|---|
| 337 | 158 | 179 | |
| Age (years) | 54.1 ± 17.8 | 51.1 ± 17.0 | 56.7 ± 18.1** |
| Height (cm) | 159.5 ± 10.7 | 167.6 ± 7.2 | **152.4 ± 7.9 |
| Body weight (kg) | 62.4 ± 14.3 | 68.2 ± 14.2 | **57.2 ± 12.3 |
| Waist circumference (cm) | 88.6 ± 12.1 | 88.5 ± 11.6 | 88.6 ± 12.6 |
| BMI (kg/m²) | 24.4 ± 4.5 | 24.2 ± 4.2 | 24.6 ± 4.7 |
| SBP (mmHg) | 131 ± 19 | 131 ± 18 | 131 ± 21 |
| DBP (mmHg) | 79 ± 12 | 79 ± 11 | 79 ± 13 |
| HDLC (mg/dl) | 59 ± 17 | 53 ± 13 | 64 ± 18** |
| HbA1C (%) | 5.7 ± 1.2 | 5.7 ± 1.3 | 5.8 ± 1.1 |
| UA (mg/dl) | 5.3 ± 1.7 | 6.0 ± 1.7 | **4.6 ± 1.4 |
**p < 0.01
Clinical characteristics and prevalences of general obesity and abdominal obesity
Table 2: Clinical characteristics in general obese (BMI ≥ 25.0) and non-obese patients with psychiatric disorders
| % (n) | Total | Male | Female | |||
|---|---|---|---|---|---|---|
| non-obese | obese | non-obese | obese | non-obese | obese | |
| 58.8% (198) | 41.2% (139 | 61.4% (97) | 38.6% (61) | 56.4% (101) | 43.6% (78) | |
| Age (years) | 56.5 ± 18.8 | 54.1 ± 17.8 | 53.9 ± 19.0** | 46.6 ± 11.9 | 58.9 ± 18.4 ** | 53.9 ± 17.4 |
| Height (cm) | 159.1 ± 10.5 | 159.5 ± 10.7 | 166.4 ± 7.6 | 169.5 ± 6.1** | 152.1 ± 8.0 | 152.8 ± 7.9 |
| Body weight (kg) | 54.4 ± 9.3 | 62.4 ± 14.3** | 59.6 ± 8.5 | 81.8 ± 10.3** | 49.4 ± 7.1 | 67.3 ± 10.1** |
| Waist circumference (cm) | 80.8 ± 7.5 | 88.6 ± 12.1 ** | 81.3 ± 6.6 | 100.0 ± 7.9 ** | 80.4 ± 8.3 | 99.3 ± 8.7 ** |
| BMI (kg/m²) | 21.4 ± 2.3 | 24.4 ± 4.5** | 21.5 ± 2.1 | 28.4 ± 2.9** | 21.3 ± 2.4 | 28.8 ± 3.5** |
| SBP (mmHg) | 128.1 ± 20.4 | 131.2 ± 19.2** | 127.8 ± 18.5 | 136.5 ± 15** | 128.3 ± 22.2 | 134.9 ± 17.7* |
| DBP (mmHg) | 76.5 ± 12.3 | 79 ± 12.3** | 76.2 ± 11.3 | 83.5 ± 10** | 76.8±13.2 | 81.8±12.4** |
| HDL--C (mg/dl) | 62.3 ± 17.7** | 58.8 ± 16.8 | 56.6 ± 13.1** | 47.9 ± 11 | 67.7 ± 19.7** | 58.7 ± 14.8 |
| HbA1C (%) | 5.7 ± 0.7 | 5.7 ± 0.8 | 5.6 ± 0.7 | 5.8 ± 1.1 | 5.7 ± 0.7 | 5.8 ± 0.7 |
| UA (mg/dl) | 4.9 ± 1.5 | 5.3 ± 1.7** | 5.6 ± 1.4 | 6.6 ± 1.9** | 4.2 ± 1.3 | 5.1 ± 1.4** |
*p < 0.05, **p < 0.01
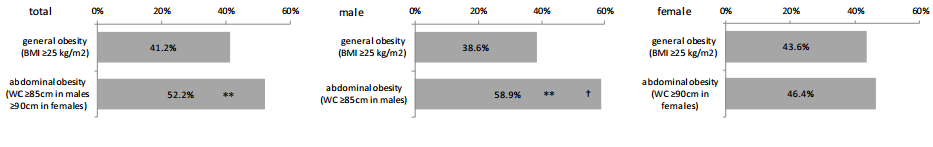
As shown in Table 2, body weight, WC, BMI, SBP, DBP and UA were significantly higher in obese patients than in non-obese patients; age and HDL-C were significantly higher in non-obese patients; and height and HbA1c did not differ significantly between the two groups. Age, body weight, WC, SBP, DBP, UA, and BMI were significantly higher in male and female patients with general obesity, whereas HDL-C was significantly higher in male and female non-obese patients. Height was significantly higher in only male patients with general obesity. There was no significant difference in HbA1c between patients with and without general obesity for both sexes. The prevalence of general obesity was 41.2% in total, 38.6% in males and 43.6% in females, with no significant gender difference, but tendency to be higher in females (Figure 1).
Figure 1: Prevalences of general obesity and abdominal obesity in patients with psychiatric disorders.
**p < 0.01 vs. general obesity, p < 0.05 vs. female abdominal obesity Rates of diabetes in patients with general obesity and abdominal obesity.
Table 3: Clinical characteristics in abdominally obese (WC ≥ 8 5cm in males and ≥ 90 cm in females) and non-obese patients with psychiatric disorders
| % (n) | Total | Male | Female | |||
|---|---|---|---|---|---|---|
| non-obese | obese | non-obese | obese | non-obese | obese | |
| 47.8% (161) | 52.2% (176) | 41.1% (65) | 58.9% (93) | 53.6% (96) | 46.4% (83) | |
| Age (years) | 55.8 ± 9.2* | 52.5 ± 16.3 | 52.6 ± 19.4 | 50.1 ± 15.2 | 58.1 ± 18.8 | 55.2 ± 17.1 |
| Height (cm) | 157.4 ± 10.8 | 161.5 ± 10.3** | 165.9 ± 7.4 | 168.8 ± 6.8 | 151.7 ± 8.7 | 153.3 ± 6.9 |
| Body weight (kg) | 52.3 ± 8.2 | 71.6 ± 12.3** | 56.4 ± 7.4 | 76.4 ± 11.8** | 49.5 ± 7.6 | 66.2 ± 10.5** |
| Waist circumference (cm) | 78.4 ± 6.1 | 97.9 ± 8.2** | 77.5 ± 4.3 | 96.2 ± 8.5** | 79.0 ± 7.0 | 99.7 ± 7.5** |
| BMI (kg/m²) | 21.1 ± 2.5 | 27.4 ± 3.7** | 20.4 ± 1.7 | 26.8 ± 3.4** | 21.5 ± 2.9 | 28.1 ± 3.9** |
| SBP (mmHg) | 127.8 ± 20.2 | 134.2 ± 17.8** | 128.0 ± 18.9 | 133.4 ± 16.3* | 127.8 ± 21.0 | 135.1 ± 19.4 |
| DBP (mmHg) | 76.1 ± 11.2 | 81.7 ± 12.7** | 75.5 ± 10.9 | 81.5 ± 11.2** | 76.6 ± 11.4 | 81.8 ± 14.2** |
| HDL---C (mg/dl) | 64.4 ± 17.5** | 53.7 ± 14.4 | 57.7 ± 12.0** | 50.1 ± 12.8 | 68.8 ± 19.2** | 57.7 ± 15.1 |
| HbA1C (%) | 5.6 ± 0.6 | 5.7 ± 1.8** | 5.6 ± 0.7 | 5.8 ± 1.0 | 5.7 ± 0.6 | 5.9 ± 0.8 ** |
| UA (mg/dl) | 4.8 ± 1.4 | 5.7 ± 1.8** | 5.5 ± 1.3 | 6.3 ± 1.9** | 4.3 ± 1.3 | 5.1 ± 1.5** |
*p < 0.05, **p < 0.01
As shown in Table 3, age and HDL-C were significantly higher in non-obese patients, while all other values were significantly higher in obese patients. Body weight, BMI, SBP, DBP, UA, and WC were significantly higher in male and female patients with abdominal obesity, whereas HDL-C was significantly higher in male and female non-abdominally obese patients. Age did not differ between males and females with abdominal obesity, but HbA1c were significantly higher in females with abdominal obesity. The prevalence of abdominal obesity was 52.2% in total, 58.9% in males and 46.4% in females, with a significantly higher prevalence in males than in females (Figure 1). The prevalence of abdominal obesity was significantly higher than that of general obesity in total and in males, but there was no difference between this prevalence's in females (Figure 1).
Relationship between diabetes and both types of obesity
Table 4: Clinical characteristics in diabetic and non-diabetic patients with psychiatric disorders
| % (n) | Total | Male | Female | |||
|---|---|---|---|---|---|---|
| non-diabetic 88.7% (299) | diabetic 11.3% (38) | non-diabetic 88.60% (140) | diabetic 11.4% (18) | non-diabetic 88.80% (159) | diabetic 11.2% (20) | |
| Age (years) | 53.6 ± 18.0 | 57.7 ± 5.5 | 50.7 ± 17.4 | 54.4 ± 13.4 | 56.2 ± 18.2 | 60.7 ± 17.0 |
| Height (cm) | 159.6 ± 10.9 | 158.8 ± 9.7 | 167.7 ± 7.3 | 166.6 ± 6.5 | 152.5 ± 8.2 | 151.7 ± 5.8 |
| Body weight (kg) | 61.8 ± 14.2 | 66.6 ± 14.4 | 67.7 ± 14.1 | 71.8 ± 15.3 | 56.6 ± 12.3 | 61.9 ± 12.0 |
| Waist circumference (cm) | 87.9 ± 11.9 | 93.8 ± 12.4** | 87.9 ± 11.2 | 93.0 ± 13.8 | 87.9 ± 12.6 | 94.5 ± 11.3* |
| BMI (kg/m²) | 24.1 ± 4.4 | 26.4 ± 4.9* | 24.0 ± 4.0 | 25.8 ± 5.1 | 24.3 ± 4.7 | 26.9 ± 4.8* |
*p < 0.05, **p < 0.01 vs. non-diabetes
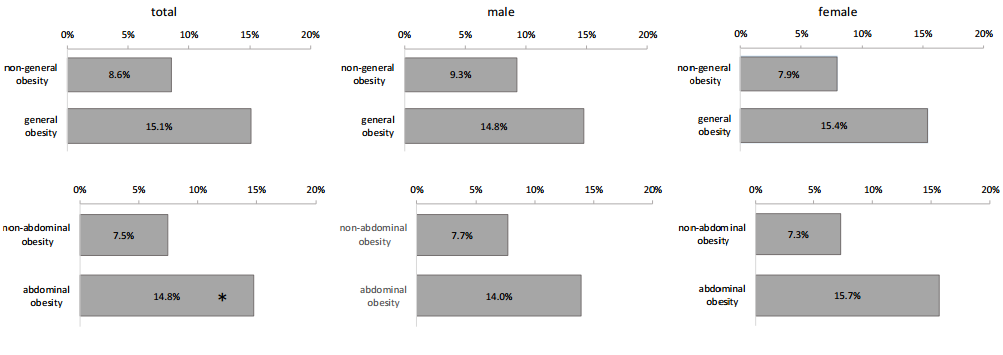
As shown in Table 4, WC and BMI were significantly higher in patients with psychiatric disorders with diabetes compared to those without diabetes in total and females, but there was no significant difference in males. There were no differences in diabetic association rate between general obese and non-general obese patients in total, males and females, and significant difference was observed only in totals between abdominal obese and non-abdominal obese patients (Figure 2). No significant differences in diabetic association rate ware observed between general obese and abdominal obese patients (Figure 2).
Figure 2: Association rates of diabetes in patients with psychiatric disorders.
*p < 0.05 vs. non-abdominal obesity
To examine the correlation between diabetes and general or abdominal obesity, multiple logistic regression analyses were performed to identify factors with a potential association with diabetes. Gender, age, general obesity and abdominal obesity were used as the explanatory variables. In these analyses, general obesity (OR 2.2, 95%CI 1.1-4.5, p = 0.03) (Table 5a) and abdominal obesity (OR 2.3, 95%CI 1.1-5.0, p < 0.03) (Table 5b) both showed a significant association with diabetes.
Table 5: Multiple logistic regression analyses of the risk of diabetes in patients with psychiatric disorders
a: explanatory variables: age, gender, general obesity (BMI ≥ 25kg/m²)
| Variable | Adjusted OR | (95% Cl) | p | |
|---|---|---|---|---|
| Age | unit odds ratio | 1.02 | (0.99-1.04) | 0.08 |
| Gender | male | 1 | - | - |
| female | 1.2 | (0.6-2.4) | 0.62 | |
| General obesity | non-obesity | 1 | - | - |
| obesity | 2.2 | (1.1-4.5) | 0.03* | |
b: explanatory variables: age, gender, abdominal obesity (WC ≥ 85cm in male, ≥ 90cm in females)
| Variable | Adjusted OR | (95% Cl) | p | |
|---|---|---|---|---|
| Age | unit odds ratio | 1.02 | (0.99-1.04) | 0.12 |
| Gender | male | 1 | - | - |
| female | 1.01 | (0.5-2.0) | 0.97 | |
| General obesity | non-obesity | 1 | - | - |
| obesity | 2.3 | (1.1-5.0) | 0.02* | |
Discussion
We found in this study, the prevalence's of general obesity (38.6% in males and 43.6% in females) and abdominal obesity (58.9% in males and 46.4% in females) were very high. There was a trend for a higher prevalence of general obesity in females, while the prevalence of abdominal obesity was significantly higher in males. The prevalence of abdominal obesity was significantly higher than that of general obesity in total and in males.
The prevalence's of general obesity in the general population in Japan are 30.4% in males and 20.2% in females, and those for abdominal obesity are 52.9% in males and 17.9% in females, based on the National Health and Nutrition Survey of the Ministry of Health, Labor and Welfare[20]. Thus, in the male patients with psychiatric disorders in this study, the prevalence's were high compared to those in males in the general population. However, the prevalence's in the female patients with psychiatric disorders in this study were more than double those in females in the general population. The prevalence's in general obesity in the general population are generally higher in males; in contrast, the prevalence of general obesity in patients in this study was slightly higher in females, and the prevalence of general obesity was more than double compared to that in females in the general population. The prevalence of abdominal obesity in male patients was slightly high compared to that in the generation. In contrast, the prevalence of abdominal obesity in female patients in this study was more than 2.5-fold high compared to that in females in the general population, although it was still lower than that in male patients. Similar higher prevalence's of general obesity in female psychiatric patients have been found in Japan[9-11] and worldwide[9]. The reason for the markedly high prevalence's of general and abdominal obesities especially in female patients with psychiatric disorders cannot be clarified from the data in this study. It is likely that patients with psychiatric disorders often engage in overeating, excessive snacking, and excessive intake of soft drinks, which causes consumption of large amounts of fat, sugar and resultant high energy intake due to difficulty with self-management[21,22]. Adverse effects of antipsychotic medication may also worsen high energy intake and reduce energy expenditure[23,24]. Social withdrawal, autism, over-sedation and daytime sleepiness may also reduce physical activity, which reduces energy expenditure due to the pathological background[25,26]. We speculate that in these situations energy balance is difficult to maintain, and this may result in weight gain and obesity in patients with psychiatric disorders, especially in female patients.
We next explored the relationship between diabetes mellitus and both types of obesity
There was no difference in diabetic association rate between patients with and without general obesity or between those with and without abdominal obesity in males and females; however, this rate was significantly higher only when evaluated for all patients with abdominal obesity compared to those without abdominal obesity. There was neither difference in diabetic association rate between patients with general obesity and those with abdominal obesity, in total and in males and females. However, multiple logistic regression analyses using gender, age, general obesity and abdominal obesity as explanatory variables indicated that general obesity and abdominal obesity both are risk factors for diabetes mellitus. The results suggested that both general obesity and abdominal obesity are equally risk factor for diabetes mellitus. This issue needs further investigation by large number of patients with psychiatric disorders in Asian countries.
Treatment of obesity is needed in patients with psychiatric disorders. Diet and exercise therapies may be difficult to use in psychiatric patients due to their disease conditions[21,22] or the adverse effects of antipsychotic drugs[23,24]. Several studies have indicated the efficacy of cognitive therapy on body weight gain using nutrition and exercise support[27,28] and the efficacy of behavior therapy using lifestyle-improving programs[28,29]. However, psychiatric patients may have difficulties with these therapies due to problems with self-control and psychiatric conditions, and successful treatment may require team healthcare delivered by nurses, pharmacists, dietitians, occupational therapists and clinical psychologists, in addition to doctors.
Anti-obesity drugs may be useful for treatment of psychiatric patients with obesity, especially in Asians since the minimum requirement to improve obesity-associated disorders has been shown to be a 3% body weight change in Japanese patients[30]. Several anti-obesity drugs with approval for long-term use worldwide have recently been discontinued due to adverse reactions[31,32], but lorcaserin, a serotonin agonist[33], and phentermine, a norepinephrine stimulator, plus topiramate, an anti-epileptic agent, have been approved for body weight reduction in the United States[34], and other anti-obesity drugs are likely to become available. Bariatric surgery has also become common and patients with extreme obesity frequently undergo gastric bypass surgery that subsequently results in weight loss ( ≥ 10%) by reducing food consumption and inhibiting the increased cytokine secretion associated with obesity, which contributes to improvement of disorders such as diabetes and other lifestyle-related diseases[35,36]. These therapies are options for treatment of obese psychiatric patients with lifestyle-related diseases. Strategies for addressing obesity in these patients are particularly important, given our findings that the prevalence's of general and abdominal obesity in patients with psychiatric disorders were high compared to those in the general population.
There are several limitations in this study. First, there is lack of power due to the relatively small number of participants, which makes it difficult to obtain definitive results. Second, the effects of antipsychotic drugs were not analyzed. Almost all the subjects took several antipsychotic drugs, since the hospital specifically treats patients with psychiatric conditions, and accurate information on all drug classes taken by individuals was not available. Third, the patients had lifestyle problems such as poor eating habits and lack of physical activity. Patients with psychiatric disorders usually have a poor diet and are inactive, and these factors may have affected the results most in this study. Further studies are needed to determine the influence of such factors in large number of patients with psychiatric disorders.
Acknowledgments
We greatly appreciate the cooperation of the outpatients at Komoro Kogen Hospital who participated in this study. We are also deeply grateful for the support of Dr. Shoda, Director of Komoro Kogen Hospital; Dr. Murasugi, Psychiatrist; and the clinic staff, including RN Takahashi, Head Nurse.
Conflicts of Interest: The authors declare that they have no conflict of interest.
References
- 1. Matsuzawa, Y. Pathophysiology and molecular mechanisms of visceral fat syndrome: the Japanese experience. (1997) Diabetes Metab Rev 13(1): 3-13.
- 2. Yoshiike, N., Nishi, N., Matsushima, S., et al. Correlation between values of body mass index and risk for diabetes, hypertension and dislipidemia: analysis of a multicenter study (in Japanese). (2000) J Jpn Soci Stud Obesity 6: 4-17.
- 3. Stevens, J., Cai, J., Pamuk, E.R., et al. The effect of age on the association between body-mass index and mortality. (1998) N Engl J Med 338(1): 1-7.
- 4. Amaddeo, F., Bisoffi, G., Bonizzato, P., et al. Mortality among patients with psychiatric illness. A ten-year case register study in an area with a community-based system of care. (1995) Br J Psychiatry 166(6): 783-788.
- 5. Hewer, W., Rossler, W., Fatkenheuer, B., et al. Mortality among patients in psychiatric hospitals in Germany. (1995) Acta Psychiatr Scand 91(3): 174-179.
- 6. Federation I.D. IDF Diabetes Atlas. International Diabetes Federation (2011) Belgium.
- 7. Ma, R.C., Chan, J.C. Type 2 diabetes in East Asians: similarities and differences with populations in Europe and the United States. (2013) Ann N Y Acad Sci 1281: 64-91.
- 8. Galletly, C.A., Foley, D.L., Waterreus, A., et al. Cardiometabolic risk factors in people with psychotic disorders: the second Australian national survey of psychosis. (2012) Aust N Z J Psychiatry 46(8): 753-761.
- 9. Foley, D.L., Mackinnon, A., Watts, G.F., et al. Cardiometabolic risk indicators that distinguish adults with psychosis from the general population, by age and gender. (2013) PLoS One 8(12): e82606.
- 10. Saiga, M., Watanabe, T., Yoshioka, S. Physical and mental factors associated with obesity in individuals with mental disorders attending psychiatric day-care facilities. (2013) Yonago Acta Med 56(1): 1-6.
- 11. Ido, Y., Makino, J., Okushima, R., et al. Factors on life-style-related disorders found in day-care schizophrenics. (2002) Aino J 1: 29-34.
- 12. Balkau, B., Deanfield, J.E., Despres, J.P., et al. International Day for the Evaluation of Abdominal Obesity (IDEA): a study of waist circumference, cardiovascular disease, and diabetes mellitus in 168,000 primary care patients in 63 countries. (2007) Circulation 116(17): 1942-1951.
- 13. Huxley, R., James, W.P., Barzi, F., et al. Ethnic comparisons of the cross-sectional relationships between measures of body size with diabetes and hypertension. (2008) Obes Rev 9(1): 53-61.
- 14. Organization W.H. The ICD-10 classification of mental and behavioural disorders.
- 15. Clinical descriptions and diagnostic guidelines. World Health Organization,Geneva (1993) New criteria for 'obesity disease' in Japan. (2002) Circ J 66: 987-92.
- 16. Ogihara, T., Kikuchi, K., Matsuoka, H., et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2009). (2009) Hypertens Res 32(1): 3-107.
- 17. Kashiwagi, A., Kasuga, M., Araki, E., et al. International clinical harmonization of glycated hemoglobin in Japan: From Japan Diabetes Society to National Glycohemoglobin Standardization Program values. (2012) J Diabetes Investig 3(1): 39-40.
- 18. Japan Atherosclerosis Society (JAS) guidelines for prevention of atherosclerotic cardiovascular diseases. (2007) J Atheroscler Thromb 5-57.
- 19. Yamanaka, H. Japanese guideline for the management of hyperuricemia and gout: second edition. (2011) Nucleosides Nucleotides Nucleic Acids 30(12): 1018-1029.
- 20. Life-style Related Diseases Control General Affairs Division M.o.H., Labour and Welfare National Health and Nutrition Survey in Japan (2007).
- 21. McCreadie, R., Macdonald, E., Blacklock, C., et al. Dietary intake of schizophrenic patients in Nithsdale, Scotland: case-control study. (1998) BMJ 317: 784-785.
- 22. Brown, S., Birtwistle, J., Roe, L., et al. The unhealthy lifestyle of people with schizophrenia. (1999) Psychol Med 29(3): 697-701.
- 23. Boehm, G., Racoosin, J.A., Laughren, T.P., et al. Consensus development conference on antipsychotic drugs and obesity and diabetes: response to consensus statement. (2004) Diabetes Care 27(8): 2088-2089.
- 24. Allison, D.B., Newcomer, J.W., Dunn, A.L., et al. Obesity among those with mental disorders: a National Institute of Mental Health meeting report. (2009) Am J Prev Med 36(4): 341-350.
- 25. De Hert, M., Dekker, J.M., Wood, D., et al. Cardiovascular disease and diabetes in people with severe mental illness position statement from the European Psychiatric Association (EPA), supported by the European Association for the Study of Diabetes (EASD) and the European Society of Cardiology (ESC). (2009) Eur Psychiatry 24(6): 412-424.
- 26. Division O.o.P.C.a.S.S.S. Health Survey for England, 1993. Health Survey for England (1993) [Health Survey for England, 1991-].
- 27. Brar, J.S., Ganguli, R., Pandina, G., et al. Effects of behavioral therapy on weight loss in overweight and obese patients with schizophrenia or schizoaffective disorder. (2005) J Clin Psychiatry 66: 205-212.
- 28. Weber, M., Wyne, K. A cognitive/behavioral group intervention for weight loss in patients treated with atypical antipsychotics. (2006) Schizophr Res 83(1): 95-101.
- 29. Kwon, J.S., Choi, J.S., Bahk, W.M., et al. Weight management program for treatment-emergent weight gain in olanzapine-treated patients with schizophrenia or schizoaffective disorder: A 12-week randomized controlled clinical trial. (2006) J Clin Psychiatry 67(4): 547-553.
- 30. Muramoto, A., Matsushita, M., Kato, A., et al. Three percent weight reduction is the minimum requirement to improve health hazards in obese and overweight people in Japan. (2014) Obes Res Clin Pract 8(5): e466-475.
- 31. Connolly, H.M., Crary, J.L., McGoon, M.D., et al. Valvular heart disease associated with fenfluramine-phentermine. (1997) N Engl J Med 337(9): 581-588.
- 32. Moreira, F.A., Crippa, J.A. The psychiatric side-effects of rimonabant. (2009) Rev Bras Psiquiatr 31(12): 145-153.
- 33. Smith, S.R., Weissman, N.J., Anderson, C.M., et al. Multicenter, placebo-controlled trial of lorcaserin for weight management. (2010) N Engl J Med 363(3): 245-256.
- 34. O'Neil, P.M., Smith, S.R., Weissman, N.J., et al. Randomized placebo-controlled clinical trial of lorcaserin for weight loss in type 2 diabetes mellitus: the BLOOM-DM study. (2012) Obesity (Silver Spring) 20(7): 1426-1436.
- 35. Moschen, A.R., Molnar, C., Geiger, S., et al. Anti-inflammatory effects of excessive weight loss: potent suppression of adipose interleukin 6 and tumour necrosis factor alpha expression. (2010) Gut 59(9): 1259-1264.
- 36. Reinehr, T., Roth, C.L., Schernthaner, G.H., et al. Peptide YY and glucagon-like peptide-1 in morbidly obese patients before and after surgically induced weight loss. (2007) Obes Surg 17(12): 1571-1577.