History of Gestational Diabetes Mellitus Leading to Type 2 Diabetes Mellitus in Hyderabad Population
Roya Rozati1,2*, A. G. Mehdi1, Akila CH1, Surayya Tahseen1, Avinash Bardia3, Aleem A Khan3
Affiliation
- 1Deccan College of Medical Sciences, Owaisi Hospital & Research Centre, Hyderabad-58, INDIA
- 2MHRT Hospital & Research Centre, Maternal Health Research Trust, Banjara Hills, Hyderabad-34, INDIA
- 3Centre for Liver Research & Diagnostics, Deccan College of Medical Sciences, Hyderabad-58, INDIA
Corresponding Author
Roya Rozati, Deccan College of Medical Sciences, Owaisi Hospital & Research Centre and MHRT Hospital & Research Centre, Maternal Health Research Trust, Banjara Hills Hyderabad-58,34 INDIA, Tel/Fax: +91(0)40 23552525; E-mail: drroyarozati@gmail.com; drrozati@rediffmail.com
Citation
Rozati, R., et al. Emergency Management of Heavy Uterine Bleeding in a Jehovas Witness. J Gynecol Neonatal Biol 2(1): 1- 4.
Copy rights
© 2015 Rozati, R. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Gestational diabetes mellitus; Per-pregnancy weight; HbA1c; Glucose oxidase peroxidase (GOD-POD) technique; Abnormal glucose tolerance
Abstract
Background: Women having gestational diabetes mellitus are at greater risk of effecting type 2 diabetes mellitus. Particularly because of the scarcity of data in India, there is requirement for understanding the distribution and possibility factors of dysglycaemia (types 2 diabetes mellitus and prediabetes) in women having affected earlier with gestational diabetes mellitus.
Methods: All women (n = 751) with past history of GDM attending two obstetric units in Hyderabad were invited to participate in the study. Among them 279(37.15%) accepted to take part in the present study. Socio-demographic, medical and anthropometric information were collected; and 75 gm OGTT performed.
Results: 213 (76.34%) women were found dysglycaemic within 5 year (median 14 months) of the pregnancy. Age was found to be 1.27 fold increase risk of having dysglycaemia (OR 1.27, 95% CI 1.03 - 1.35 p = 0.03). Presence of acanthosis nigricans (OR 2.09, 95% CI 1.89 - 6.56 p = 0.002), postpartum screening interval (OR 1.41, 95% CI 1.15 - 1.92 p = 0.02) were found to be risk factors to have dysglycaemia. The ADA suggested threshold HbA1c value of > 39 mmol/mol (5.6%) have a sensitivity and specificity of 72.3% and 67.3% respectively for detecting the occurrence of T2DM postpartum.
Conclusion: In conclusion, this study found a high possibility of development of t2dm among with a history of gdm and there is an immediate need to improve postpartum screening rates.
Introduction
Screening for diabetes in pregnancy not only enables enhanced intra-partum concern however provides a chance to recognize women having a possibility for development of types 2 diabetes mellitus (T2DM) in future. Women affected with gestational diabetes mellitus (GDM) represent a high risk group to be targeted for prevention of developing T2DM. A current meta-analysis has revealed that women having GDM are almost 8 times further expected to develop future T2DM when compared with the women having standard glucose tolerance (NGT) in pregnancy[1]. Whereas greater incidence of both T2DM and GMD are reported in India[2,3]. At present there is inadequate information available about the progression of T2DM in women with earlier GDM[4-6].
The American Diabetes Association (ADA) guidelines state that women with GDM ought to undergo screening for continual diabetes at 6-12 weeks postpartum, by means of the 2 hour OGTT[7]. Consequently, they have been supposed to have lifelong screening for the advance of diabetes at a minimum of every 3 year in case of normal glycaemic condition and once in a year in case of prediabetes.
The UK NICE guidelines states that a fasting plasma glucose test was supposed to be done at the 6-13 weeks postnatal appointment, subsequently repeated once a year[8]. Nevertheless, various factors like time commitment, increased costs, and need for phlebotomy services harmfully impact the recognition and likelihood of post-partum OGTT by patients and health care providers[9]. A survey based on a solitary, non-fasting blood sample is probable to be further satisfactory and enhance the rate of postpartum evaluation of glycaemic condition[9]. In recent times, the ADA and WHO recommended utilizing HbA1c for approving the analysis of diabetes and pre-diabetes provided the test is performed by a technique that is licensed by the national Glycohemoglobin standardization program in the USA and is standardized or traceable to the diabetes control and complication trial (DCCT)reference assay[10,11]. Whereas HbA1c is progressively used more to analyze diabetes and pre-diabetes, present are less studies all over the world (none from south Asia)[12], which have assessed its effectiveness in a population of women with earlier GDM. Therefore, we designed this study to recognize the distribution of dysglycaemia [T2DM; impaired fasting glucose (IFG); and impaired glucose tolerance (IGT)] among women with past history of GMD and evaluate the risk factors linked with it. We also evaluated the importance of HbA1c in the postpartum re-classification of women with GDM in a huge urban cohort of Indian women.
Materials and Methods
By means of medical records from Obstetrics Departments, women who have been repeatedly diagnosed through GDM based on carpenter and coustan criteria throughout pregnancy in the former 8 year (2006-2013) were recognized from one large centers in India (MHRT-Hospital and Research Trust, Hyderabad) by retrospective medical record review. In addition, women diagnosed with GDM based on newer International Association of Diabetes a Pregnancy Study Group (IADPSG) criteria were further enrolled from 2011 onward[7]. The study was agreed by ethics committees and written informed consent for participation was maintained from all patients.
Participants finished a well planned interview to make available data on age, previous history of GDM, family history of diabetes, the requirement for insulin during pregnancy, and per-pregnancy weight (which was used to calculate their per-pregnancy body mass index (BMI)). The subsequent dimension was also considered weight, height waist circumference, BMI, and blood pressure at moment of testing. Appearance or nonappearance acanthosis nigricans/skin tags were noted.
Blood sample were collected following a minimum 8 hour of fasting. The OGTT was performed as stated by the World health Organization (WHO)[7].
Total cholesterol, triglyceride and HDL cholesterol levels were calculated by end point assay method with ERBA semi auto analyzer (ERBA diagnostics, Mannheim, Germany). LDL cholesterol was calculated by friedewald equation. To calculate blood glucose, samples were collected in a fluoride vial and analyzed by glucose oxidase peroxidase (GOD-POD) technique by means of ERBA semi auto analyzer (ERBA diagnostics, Mannheim, Germany).
HbA1c was collected in EDTA-vials and analyzed by High Performance Liquid Chromatography (HPLC) based Ion Exchange Chromatography (Bio-Rad D-10tm hemoglobin A1c program, Bio-Rad laboratories, Inc., Hercules, CA94547,U.S.A) individuals were classified as being normoglycaemic (FPG < 5.6mmol/Land 2-h plasma glucose < 7.8mmol/L) with pre-diabetes (FPG = 5.6 - 6.9mmol/Land /or2-h plasma glucose = 7.8 - 11mmol/L ). The effectiveness of HbA1c was measured against OGTT criteria for analysis of diabetes and pre-diabetes. Statistical calculation was done using Graph pad software version 5.0 (college station, Texas, USA). Data were accessed as number (%) or mean ± SD as apt. The occurrence of dysglycaemia (95% confidence interval) was calculated. ANOVA test was used to test the differences among groups as appropriate. Logistic regression analysis was used and the consequences were reported as OR (95% C.I.). Test sensitivity and specificity were used to explain the diagnostic precision of HbA1c. Significance level were set at p < 0.05.
Results
A total of 751 women were ask to visit clinic for testing, but only 279 (36.08%) women were consented to take part in study. The mean age was 31.6 ± 3.5 years. The analysis was carried at 18.7 ± 14.1 months postpartum (Table 1). Normoglycaemia and dysglycaemia were recognized by OGTT. The allocation of the biochemical, clinical and anthropometric variables in women were shown in table 1 and 2. Women with normoglycaemia were younger (29.5 ± 3.7 year vs. 31.4 ± 3.8 year, p = 0.03) and assessed after a lesser postpartum interval (14.7 ± 11.6 vs. 20.1 ± 15.7 months; p = 0.02) in comparison with those of dysglycaemia. Presence of acanthosis nigricans was found higher in dysglycaemia when compare to normoglycaemia (89.04% and 10.95% respectively)
Table 1: Distribution of clinical variables in women with normal or abnormal glucose tolerance
| Parameter | Total N = 279 |
Normal OGTT n = 66 (23.65%) |
Abnormal OGTT n = 213 (76.34%) |
|---|---|---|---|
| Age (years) | 31.6 ± 3.7 | 29.5 ± 3.5 | 31.4 ± 3.8 |
| Time of postpartum screening (months since delivery) | 18.7 ± 14.1 | 14.7 ± 11.6 | 20.1 ± 15.7 |
| Presence of Acanthosis | 73(26.16%) | 8 (10.95%) | 65 (89.04%) |
| History of GDM in any pregnancy other than index pregnancy | |||
| Yes | 87 (31.18%) | 20 (22.98%) | 67 (77.01%) |
| BMI kg/m² (pre-pregnancy) | |||
| < 25kg/m² | 216 (77.41%) | 48 (72.72%) | 168 (78.87%) |
| 25-29.9 kg/m² | 52 (18.63%) | 16 (24.24%) | 36 (16.90%) |
| ≥ 30 kg/m² | 11 (3.94%) | 2 (3.03%) | 9 (4.22%) |
| Occupation | |||
| Employed | 31 (11.11%) | 9 (13.63%) | 22 (10.32%) |
| Housewife | 248 (88.88%) | 57 (86.36%) | 191 (89.67%) |
| Highest level of Education | |||
| Graduate/postgraduate | 156 (55.91%) | 38 (57.57%) | 118 (55.39%) |
| Less than graduate | 123 (44.08%) | 28 (42.42%) | 95 (44.60%) |
| Diagnosis of GDM (Trimester) | |||
| First | 37 (13.26%) | 5 (7.57%) | 32 (15.02%) |
| Second | 215 (77.06%) | 52 (78.78%) | 163 (76.52%) |
| Third | 27 (09.67%) | 9 (13.63%) | 18 (8.45%) |
| Insulin treatment % | |||
| Required | 185 (64.30%) | 33 (50.00%) | 152 (71.36%) |
| Not required | 94 (33.69%) | 33 (50.00%) | 61(28.63%) |
BMI: Body mass index; GDM: gestational diabetes mellitus
Risk factor analysis
Age was found to be 1.27 fold increase risk with higher likelihood of having dysglycaemia (OR 1.27, 95% CI 1.03 - 1.35 p = 0.03). At the time postpartum, Greater postpartum BMI (OR 1.23, 95% CI 1.12 - 1.73 p = 0.04) were also found to be associated with probability to have dysglycaemia. Presence of acanthosis nigricans (OR 2.09, 95% CI 1.89 - 6.56 p = 0.002), postpartum screening interval (OR 1.41, 95% CI 1.15 - 1.92 p = 0.02) were linked by means of a elevated probability to have dysglycaemia (Table 2)
Table 2: Risk factors for abnormal glucose tolerance (213 Subjects)
| Variable | OR( 95% CI) | p value |
|---|---|---|
| Age (year) | 1.27 (1.03-1.35) | 0.03 |
| Postpartum screening interval (month) | 1.41 (1.15 - 1.92) | 0.02 |
| BMI kg/m² (at time of postpartum testing) (per kg/m²) | 1.23 (1.12 - 1.73) | 0.04 |
| Acanthosis nigricans/skin tags | ||
| No | 1.00 | |
| Yes | 2. 09 (1.89- 6.56) | 0.002 |
BMI: Body mass index; GDM: gestational diabetes mellitus
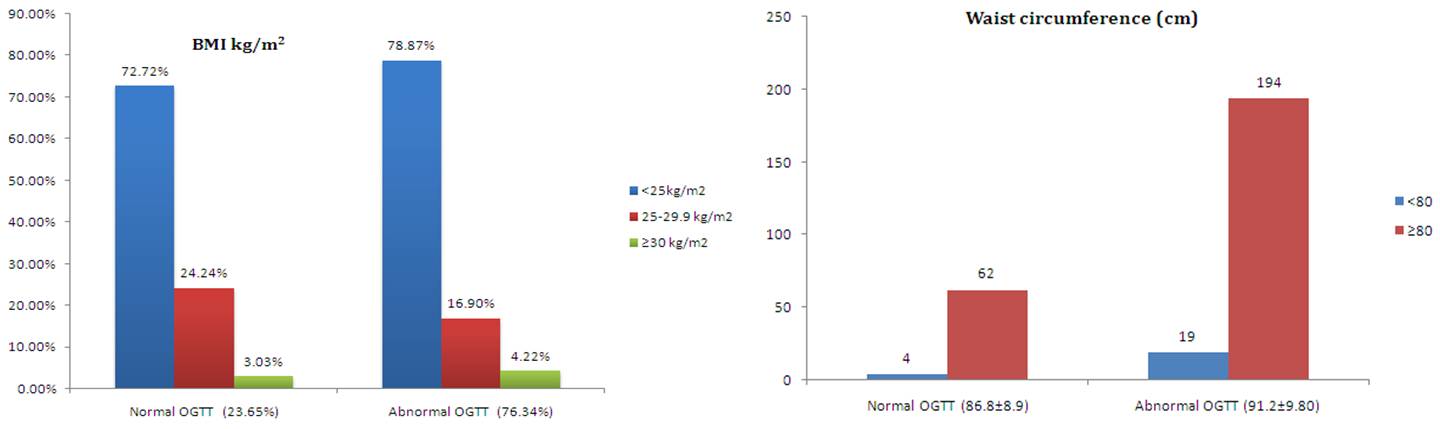
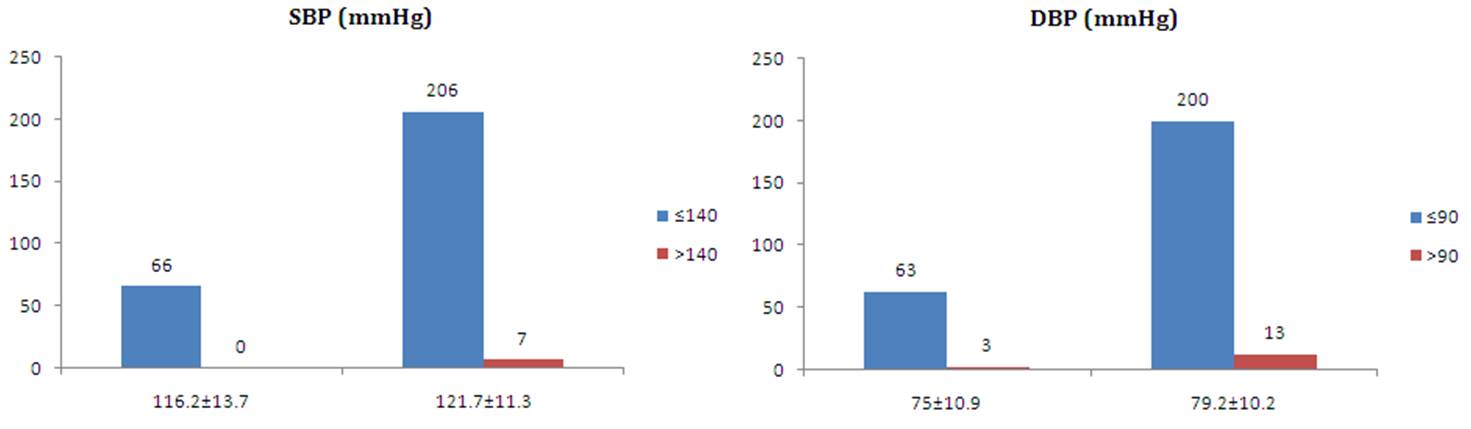
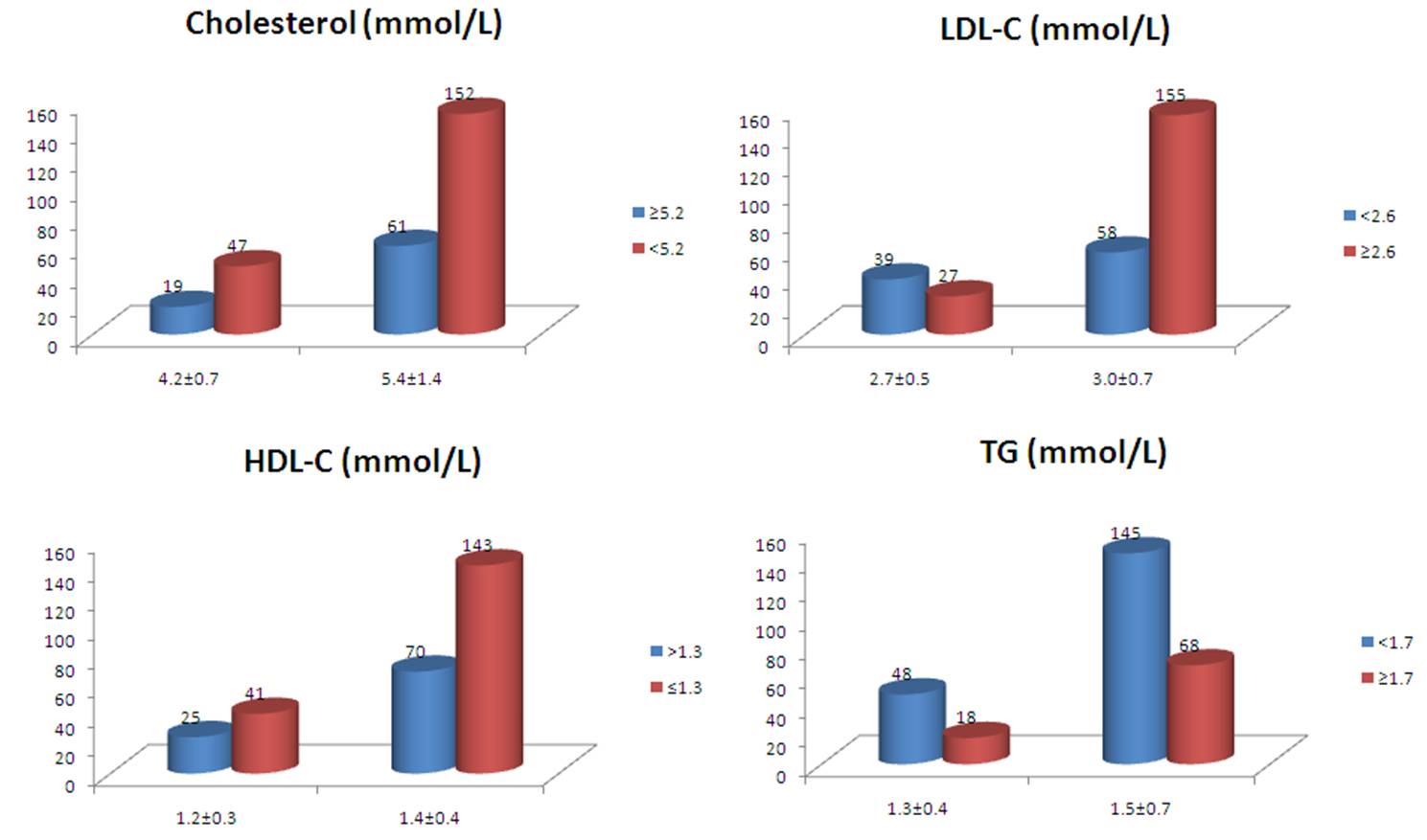
The predictors of cardiovascular risk: BMI, waist height ratio were considerably elevated amongst the women with dysglycaemia (Figure 1). Blood pressure was also found to be high risk factor amongst the women with dysglycaemia (Figure 2). Lipid was considerably prominent between the women with dysglycaemia (Figure 3).
Figure 1:
Figure 2:
Figure 3:
Performance of HbA1c and FPG compared to OGTT
The sensitivity and specificity of suggested threshold of ≥ 39 mmol/mol (5.7%) to find out any degree of abnormal glucose tolerance(diabetes + prediabetes) was 72.3% and 67.3% correspondingly with a positive predictive value (PPV) and a negative predictive value (NPV)of 86.5% and 49.7% respectively (Table 3). The sensitivity and specificity of ADA cutoff of ≥ 5.6 mmol/L for detecting any degree of abnormal glucose tolerance (diabetes+ prediabetes) was 84.5% and 100% with PPV and NPV of 100% and 72.5% respectively (Table 3).
Table 3: Performance of fasting glucose (FPG) ≥ 5.6 mmol/L (100 mg/dl) and HbA1c ≥ 39 mmol/mol (5.7%) for diagnosis of abnormal glucose tolerance (diabetes or prediabetes)
| Parameter | Sensitivity | Specificity | Positive predictive value | Negative predictive value |
|---|---|---|---|---|
| HbA1c | 72.3% | 67.3% | 86.5% | 49.7% |
| FPG | 84.5% | 100% | 72.5% | 76.1% |
Discussion
The cumulative incidence of diagnosed diabetes among the women with a history of GDM has been noted to be comparatively greater among south Asian[13]. We observed an overall prevalence of 32.25% for diabetes, at median period of 14 months of postpartum screening. The incidence of was nearly 50% when the mean follow up period exceeded 2years, which is much former than those reported by other Indian studies (35% - 50%, at mean follow up of 5 years)[4-6]. The occurrence of diabetes in our study group is as well greatly elevated than has been published in general population studies. In the INDIAB study, the occurrence was 1.4% in 20 - 29 year age group and 4.9% in a 30 - 39 year age group, compared to 25% and 42% respectively in our study.
We furthermore evaluated the effectiveness of HbA1c and FPG compared to 75g OGTT in recognition of dysglycaemia in postpartum women .We established that in the postpartum period, the ADA cut-off value of 39 mmol/L (5.6%) of HbA1c, for diabetes, has a sensitivity of 72.3% and specificity of 67.3% by means of the FPG criterion only for diabetes, the sensitivity was 84.5% with specificity of 100%. A recent meta- analysis of six studies evaluated the usefulness of HbA1c for diagnosis of abnormal glucose tolerance in postpartum screening[12]. This meta-analysis established low sensitivity and specificity of HbA1c at cut off level ≥ 39 mmol/mol (5.7%) to identify any degree of glucose intolerance. Our results were similar to those published by kim et al. (65% and 68% respectively) incorporated in the meta-analysis[14], through compared screening intervals (19.6 ± 15.3 months in present study; 18 ± 12 months in the study by Kim et al.).
By means of either FPG or HbA1c, we might have been missed nearly 18% of cases of diabetes that would or else have been identified with OGTT. Bearing in mind the elevated conversion rates for diabetes, this discovery has significant implications. Initially, these women may go on to have successive pregnancies with undiagnosed type 2 diabetes and potentially poor glycaemic control, raising the possibility of congenital anomalies and additional fetal or maternal complications. Second, failure to recognize glucose intolerance (either per-diabetes or diabetes) prevents these women from implementing behavioral and medication interventions that might decrease their possibility of developing diabetes or its micro vascular and macro vascular complications, deteriorating their long-term health. The consequences of our study imply that the OGTT is still mainly suitable test to identify diabetes in the postpartum period.
We conducted a thorough assessment of risk factors related with increased incidence of T2DM amongst the women having a history of GDM. Predictors of cardiovascular risk: BMI, waist circumference, blood pressure, and abnormal lipid parameters were considerably elevated among women with dysglycaemia. We hypothesize so as to this might be one of the reasons for greater frequency of dysglycaemia among this population. The parameters related with insulin resistance including waist circumference, waist-height ratio, and acanthosis nigricans were greater in women with dysglycaemia. These consequences imply obesity, mostly visceral obesity, is linked with greater possibility of diabetes.
Only 37.15% of women with GDM decided to undergo testing in perspective of this research study. In common, postpartum screening is apparently low in other parts of world, unreliable from 14% in usual case to 60% in a randomized controlled study[15]. Hunt and colleagues noticed postpartum screening rates from 23% to 58% on screening with a FPG or a 2-hour 75-g OGTT[16]. The necessity for improving postpartum rates must be one of the top priorities for clinicians and public health policy markers.
The modest contribution rates might be seen as a most important restriction of this study. It is probable that women at higher or lower risk of developing dysglycaemia may have been further expected to respond to invitation. Further major limitation is that preconception diabetes status was not identified and only 25 out of 279 patients were tested between 6- 12 weeks after delivery, which might has lead to conclusion whether or not the index pregnancy was difficult with pre-conception diabetes. Yet, known the age and sex related common population estimates of the incidence of type 2 diabetes, it is probable that the enormous majority of women, who were diagnosed with type 2 diabetes in the post-partum period, were de novo cases.
The strength of this research consist of a comparatively large population cohort evaluated prospectively, performing an assessment of the effectiveness of HbA1c for the first time among an Indian population with GDM, and a comprehensive assessment of risk factors.
In conclusion, this study found a high possibility of development of T2DM among with a history of GDM at median follow up of 14 months. There is an immediate need to improve postpartum screening rates, and execute early intervention strategies to decrease the chance of diabetes among women with gestational diabetes.
Acknowledgment
The authors thank Maternal Health and Research Trust (MHRT) and Owaisi Hospital and Research Centre, Hyderabad, India.
Conflict of interest: None
References
- 1. Bellamy, L., Casas, J.P., Hingorani, A.D., et al. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. (2009) Lancet 373(9677): 1771-1779.
- 2. Guariguata, L., Linnenkamp, U., Beagley, J., et al. Global estimates of the prevalence of hyperglycaemia in pregnancy. (2014) Diabetes Res Clin Pract 103(2): 176-185.
- 3. Ramachandran, A., Snehalatha, C., Ma, R.C. Diabetes in South-East Asia: an update, (2014) Diabetes Res Clin Pract 103(2): 231-237.
- 4. Krishnaveni, G.V., Hill, J.C., Veena, S.R., et al. Gestational diabetes and the incidence of diabetes in the 5 years following the index pregnancy in South Indian women. (2007) Diabetes Res Clin Pract 78(3): 398-404.
- 5. Kale, S.D., Yajnik, C.S., Kulkarni, S.R., et al. High risk of diabetes and metabolic syndrome in Indian women with gestational diabetes mellitus. (2004) Diabet Med 21(11): 1257-1258.
- 6. Mahalakshmi, M.M., Bhavadharini, B., Kumar, M., et al. Clinical profile, outcomes, and progression to type 2 diabetes among Indian women with gestational diabetes mellitus seen at a diabetes center in South India. (2014) Indian J Endocrinol Metab 18(3): 400-406.
- 7. American Diabetes Association. Standards of medical care in diabetes. (2014) Diabetes Care 37: S14-s80.
- 8. NICE clinical guideline. Diabetes in pregnancy: (2015) management of diabetes and its complications from preconception to the postnatal period.
- 9. Carson, M.P., Morgan, B., Gussman, D., et al. SUGAR: Spotting undiagnosed glucose abnormal results-A new protocol to increase postpartum testing among women with gestational diabetes mellitus. (2015) Am J Perinatol 32(3): 299-306.
- 10. International Expert Committee. International Expert Committee report on the role of A1C assay in the diagnosis of diabetes. (2009) Diab Care 32(7): 1327-1334.
- 11. International Diabetes Federation Guideline Development Group. Global guideline for type 2 diabetes. (2014) Diab Res Clin Pract 104(1): 1-52.
- 12. Su, X., Zhang, Z., Qu, X., et al. Hemoglobin A1c for diagnosis of postpartum abnormal glucose tolerance among women with gestational diabetes mellitus: diagnostic meta-analysis. (2014) PLoS One 9(7): e102144.
- 13. Mukerji, G., Chiu, M., Shah, B.R. Impact of gestational diabetes on the risk of diabetes following pregnancy among Chinese and South Asian women. (2012) Diabetologia 55(8): 2148-2153.
- 14. Kim, C., Herman, W.H., Cheung, N.W., et al. Comparison of hemoglobin A1c with fasting plasma glucose and 2-h post challenge glucose for risk stratification among women with recent gestational diabetes mellitus. (2011) Diab Care 34(9): 1949-1951.
- 15. Cark, H.D., Graham, I.D., Karovitch, A., et al. Do postal reminders increase postpartum screening of diabetes mellitus in women with gestational diabetes mellitus? A randomized controlled trail. (2009) Am J Obstet Gynecol 200(6): 634e1-7.
- 16. Hunt, K.J., Logan, S.L., Conway, D.L., et al. Postpartum screening following GDM: how well are we doing? (2010) Curr Diab Rep 10(3): 235-241.