Knowledge and Attitude of Infection Prevention Measures among Radiology Staff in Al Baha Hospitals.
Hossam M. El-Hawary, Nasser S Al-Ghamdi, Yazeed M Al-Zahrani, Hamzah S Al-Zahrani, Ahmed Y Al-Zahrani
Affiliation
- 1Department of Medical Microbiology, Faculty of Medicine, Al Baha University, KSA
- 2Department of Community Medicine, Faculty of Medicine, Al Baha University, KSA
- 3Department of Community Medicine, Environment and Industrial Medicine, El-Minia University, Egypt
- 4Medical Interns, Faculty of Medicine, Al Baha University, KSA
Corresponding Author
Muhammad A. Halwani, Department of Medical Microbiology, Faculty of Medicine, Al Baha University, KSA, E-mail: mhalwani@bu.edu.sa
Citation
Muhammad A. Halwani, et al. Knowledge and Attitude of Infection Prevention Measures among Radiology Staff in Al Baha Hospitals. (2017) Clin Trials Pathol Case Stud 2(1): 41- 47.
Copy rights
© 2017 Muhammad A. Halwani. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Knowledge; Attitude; Infection; Control; Radiology
Abstract
Introduction: Radiology staff is most often exposed to different infectious patients but their knowledge and attitude towards infection prevention measures has rarely been investigated.
Objectives: To evaluate the knowledge and attitudes of radiology staff at Al Baha hospitals to infection prevention measures that should be followed routinely.
Subjects and Methods: A survey was conducted using a questionnaire distributed during the 2016 academic year, among radiology staff in five different hospitals in the Al Baha area.
Results: Eighty-two of 112 staff members (73%) filled out the questionnaire. They consisted of radiologists, technicians, nurses, and others. There was no significant difference be- tween these healthcare workers in their knowledge of infection prevention measures. Moreover, the results also depicted these same healthcare workers were knowledgeable when managing patients with airborne infection: 64/82 (78%) (P = 0.02). Interestingly, the knowledge of proper cleaning and decontamination of equipment and surfaces was significantly associated with staff who had more than 10 years’ experience in this line of work. Finally, the results show that having infection control training helps radiology staff deal better with infectious patients who need specific type of precautions (air- borne, droplet, contact).
Conclusions: Radiology staff in the Al Baha Hospitals’ knowledge and attitude in infection prevention measures is fairly acceptable when dealing with infectious patients. More training is still required in order to apply standard precautions to all patients.
Introduction
Infection control is concerned with preventing the spread of infection inhealthcare institutions. It is the practical subdivision of hospital epidemiology which is practiced within any healthcare system rather than directed to the community[1]. Radiology staff in hospitals manage different patients daily. Some of them might have different infections which could be serious and might even lead to death[2]. Those patients who have infections can put the radiology staff at risk when they visit the department. Furthermore, they can also be a source of contamination to the radiology area such as surfaces, instruments, and machines[3]. Therefore, radiology staff should be knowledgeable and up-to-date to deal with such patients[4]. Moreover, they should be skilled in basic infection prevention measures in order to protect themselves and other patients from the risk of infection[5].
According to the Saudi National Council of Statistics, Al Baha area which is located in the south west part of the Kingdom of Saudi Arabia (KSA) has a population of 411,888 people. The health system in Al Baha area is managed by the Ministry of Health and has 10 hospitals with different bed capacities ranging from 30 to 350 beds. However, only five of these hospitals have radiology services. Thus, the purpose of this study is to evaluate the knowledge and attitudes of radiology staff in Al Baha hospitals towardsroutine infection prevention measures when dealing with patients.
Methods
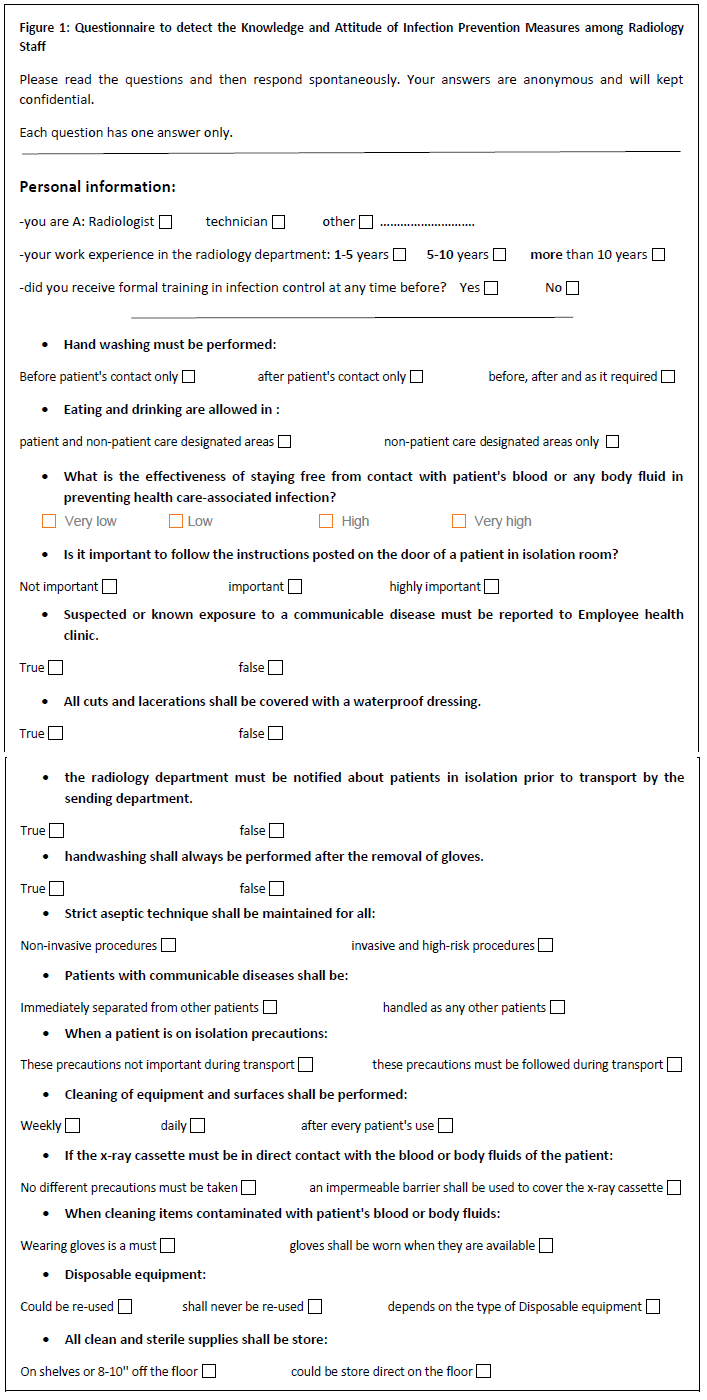
A descriptive qualitative survey was carried out among all workers in the radiology departments in the five hospitals which provide radiology services in Al Baha. A structured questionnaire (Figure 1) was distributed between the radiology staff and filled out by 73% study participants (82/112). This research was approved by the Ethical Research Committee of the Faculty of Medicine at Al Baha University. All the questionnaires were then entered and analyzed using the Statistical Package for Social Sciences (SPSS) version 16.0. Chi-square (χ²) test and Fishers exact tests were used to test for the differences between categorical data. The results were collected and analyzed using the 0.05 significance level.
Figure 1: Questionnaire to detect the knowledge and Attitude of Infection Prevention Measures among Radiology Staff
Results
This study was conducted on 82 employees in the radiology departments in Al Baha hospitals with 73% response rate. The study group was categorized according to occupation, experience, and infection control background. The results show that 58.5% of the study group had no previous training in infection prevention precautions (Table 1). Application and practice of standard precautions of infection control at the radiological departments by the study group were generally accepted (Table 2 and 3).
Table 1: General characteristics of the study group.
| General characteristics | Study group (n = 82) | |
|---|---|---|
| No | % | |
| Occupation | ||
| Radiologist | 6 | 7.3 |
| Technician | 59 | 72 |
| Nurse | 11 | 13.4 |
| Others | 6 | 7.3 |
| Occupational experience | ||
| 1 - 5 years | 27 | 32.9 |
| 6 - 10 years | 36 | 43.9 |
| > 10 years | 19 | 23.2 |
| Previous infection control training | ||
| Yes | 34 | 41.5 |
| No | 48 | 58.5 |
Table 2: Application of infection prevention precautionsof in the radiology departments.
| Application of infection prevention precautions in the radiology departments | Study group (n = 82) | |
|---|---|---|
| No | % | |
| For every patient regardless the infectious state | ||
| True | 79 | 96.3 |
| False | 3 | 3.7 |
| Department notification about isolated patient prior to transportation | ||
| True | 81 | 98.8 |
| False | 1 | 1.2 |
| For isolated patient need X-ray during transportation to the department | ||
| True | 65 | 79.3 |
| False | 17 | 20.7 |
| Patient with communicable disease shall be examined by the department | ||
| Immediately | 53 | 64.6 |
| At the end of the schedule | 29 | 35.4 |
| Cleaning and decontamination of equipment and surfaces at the department preformed | ||
| Weekly | 28 | 34.1 |
| Daily | 25 | 30.5 |
| Immediately after patient | 29 | 35.4 |
Table 3: Practice of infection prevention precautions in the radiology departments.
| Practice of infection prevention precautions in the radiology departments. | Study group (n = 82) | |
|---|---|---|
| No | % | |
| For patient with airborne infection, you should wear | ||
| N-95 mask | 64 | 78 |
| Surgical mask | 18 | 22 |
| For patient with droplet infection, you should wear | ||
| N-95 mask | 51 | 62.2 |
| Surgical mask | 31 | 37.8 |
| For patient with contact infection, you should wear | ||
| Gloves | 63 | 79.8 |
| Surgical mask | 19 | 23.2 |
| Hand washing after seeing the patient and after removal of the gloves | ||
| True | 65 | 79.3 |
| False | 17 | 20.7 |
| Gloves should be changed between patients | ||
| Sure | 53 | 64.6 |
| May be | 18 | 22 |
| I don’t know | 11 | 13.4 |
| After exposure to patient during examination you should | ||
| Go home | 16 | 19.5 |
| Go to staff clinic | 37 | 45.1 |
| Do nothing | 29 | 35.4 |
There was an insignificant relationship between staff occupation and the application of infection prevention precautions in the radiological departments (p-value > 0.05) (Table 4). Practices of precautions of infection control in the radiological departmentsfor all staff members regardless of their occupation were applied onlywhen they knew patientshadan airborne infection (p-value < 0.05) (Table 5).
Table 4: The relation between occupation and the application of infection prevention precautions in the radiology departments.
| Application of infection prevention precautions in the radiology department. | Study group (n = 82) | p value | |||
|---|---|---|---|---|---|
| Radiologist (n = 6) |
Technician (n = 59) |
Nurse (n = 11) |
Others (n = 6) |
||
| No (%) | No (%) | No (%) | No (%) | ||
| For every patient regardless the infectious state | |||||
| True | 5 (83.3%) | 58 (98.3%) | 10 (91%) | 6 (100%) | 0.2 |
| False | 1 (16.7%) | 1 (1.7%) | 1 (9%) | 0 (0%) | |
| Department notification about isolated patient prior to transportation | |||||
| True | 6 (100%) | 58 (98.3%) | 11 (100%) | 6 (100%) | 0.94 |
| False | 0 (0%) | 1 (1.7%) | 0 (0%) | 0 (0%) | |
| For isolated patient need X-ray during transportation to the department | |||||
| True | 6 (100%) | 46 (78%) | 9 (82%) | 4 (67%) | 0.52 |
| False | 0 (0%) | 13 (22%) | 2 (18%) | 2 (33%) | |
| Patient with communicable disease shall be examined by the department | |||||
| Immediately | 2 (33%) | 39 (66%) | 8 (73%) | 4 (67%) | 0.4 |
| At the end of the schedule | 4 (67%) | 20 (34%) | 3 (27%) | 2 (33%) | |
| Cleaning and decontamination of equipment and surfaces at the department preformed | |||||
| Weekly | 0 (0%) | 23 (39%) | 3 (27%) | 2 (33%) | 0.42 |
| Daily | 2 (33%) | 16 (27%) | 4(36.5%) | 3 (50%) | |
| Immediately after patient | 4 (67%) | 20 (34%) | 4 (36.5%) | 1 (17%) | |
Table 5: The relation between occupation and the practice of infection prevention precautions of the radiology staff.
| Practice of infection prevention precautions in the radiology department. | Study group (n = 82) | p value | |||
|---|---|---|---|---|---|
| Radiologist (n = 6) |
Technician (n = 59) |
Nurse (n = 11) |
Others (n = 6) |
||
| No (%) | No (%) | No (%) | No (%) | ||
| For patient with airborne infection, you should wear | |||||
| N-95 mask | 6 (100%) | 46 (78%) | 10 (91%) | 2(33%) | 0.02* |
| Surgical mask | 0 (0%) | 13 (22%) | 1 (9%) | 4 (67%) | |
| For patient with droplet infection, you should wear | |||||
| N-95 mask | 5 (83.3%) | 35 (59%) | 8 (73%) | 3 (50%) | 0.52 |
| Surgical mask | 1 (16.7%) | 24 (41%) | 3 (27%) | 3 (50%) | |
| For patient with contact infection, you should wear | |||||
| Gloves | 6 (100%) | 41 (69.5%) | 41 (69.5%) | 5 (83.3%) | 0.07 |
| Surgical mask | 0 (0%) | 18 (30.5%) | 0 (0%) | 1 (16.7%) | |
| Hand washing after seeing the patient and after removal of the gloves | |||||
| True | 6 (100%) | 47 (80%) | 8 (73%) | 4 (67%) | 0.49 |
| False | 0 (0%) | 12 (20%) | 3 (27%) | 2 (33%) | |
| Gloves should be changed between patients | |||||
| Sure | 6 (100%) | 38 (64%) | 5 (46%) | 4 (66%) | 0.43 |
| May be | 0 (0%) | 14 (24%) | 3 (27%) | 1 (17%) | |
| I don’t know | 0 (0%) | 7 (12%) | 3 (27%) | 1 (17%) | |
| After exposure to patient during examination you should | |||||
| Go home | 0 (0%) | 10 (17%) | 4 (36.5%) | 2 (33%) | 0.018* |
| Go to staff clinic | 6 (100%) | 22 (37%) | 6 (54.5%) | 3 (50%) | |
| Do nothing | 0 (0%) | 27 (46%) | 1 (9%) | 1 (17%) | |
Application and practice of infection prevention precautions in the radiological departments in relation to the experience in years was insignificant (p-value > 0.05), except when it comes to the cleaning and decontamination of equipment and surfaces in the department (p-value < 0.05) (Table 6 and 7). The relation between previous infection control training and the application of cleaning and decontamination of equipment and surfaces in the radiological departments by the study group was highly significant (p-value < 0.01) (Table 8). Table 9 shows that there is a correlation between practices of infection prevention precautionsin the Radiology departments (airborne, droplet, or contact precautions) and previous infection control training (p-value < 0.05).
Table 6: The relation between occupational experience and the application of infection prevention precautions of the radiology staff.
Cleaning and decontamination of equipment and surfaces at the department preformed
| Staff Response | Study group (n = 82) | p value | ||
|---|---|---|---|---|
| 1 - 5 years (n = 27) |
6 - 10 years (n = 36) |
> 10 years (n = 19) |
||
| No (%) | No (%) | No (%) | ||
| For every patient regardless the infectious state | ||||
| True | 26 (96%) | 35 (97%) | 18(94.8%) | 0.9 |
| False | 1 (4%) | 1 (3%) | 1 (5.2%) | |
| Department notification about isolated patient prior to transportation | ||||
| True | 26 (96%) | 36 (100%) | 19 (100%) | 0.36 |
| False | 1 (4%) | 0 (0%) | 0 (0%) | |
| For isolated patient need X-ray during transportation to the department | ||||
| True | 21 (78%) | 27 (75%) | 17 (89.5%) | 0.44 |
| False | 6 (22%) | 9 (25%) | 2 (10.5%) | |
| Patient with communicable disease shall be examined by the department | ||||
| Immediately | 17 (63%) | 22 (61%) | 14 (73.7%) | 0.64 |
| At the end of the schedule | 10 (37%) | 14 (39%) | 5 (26.3%) | |
| Weekly | 12 (44.5%) | 10 (28%) | 6 (31.2%) | 0.02* |
| Daily | 12 (44.5%) | 10 (28%) | 3 (15.8%) | |
| Immediately after patient | 3 (11%) | 16 (44%) | 10 (53%) | |
Table 7: The relation between occupational experience and the practice of infection prevention precautions of the radiology staff.
Gloves should be changed between patientsAfter exposure to patient during examination you should
| Staff Response | Study group (n = 82) | p value | ||
|---|---|---|---|---|
| 1 - 5 years (n = 27) |
6 - 10 years (n = 36) |
> 10 years (n = 19) |
||
| No (%) | No (%) | No (%) | ||
| For patient with airborne infection, you should wear | ||||
| N-95 mask | 24 (89%) | 24 (67%) | 16 (84.2%) | 0.08 |
| Surgical mask | 3 (11%) | 12 (33%) | 3 (15.8%) | |
| For patient with droplet infection, you should wear | ||||
| N-95 mask | 17 (63%) | 21 (58.3%) | 13 (68.8%) | 0.76 |
| Surgical mask | 10 (37%) | 15 (41.7%) | 6 (31.2%) | |
| For patient with contact infection, you should wear | ||||
| Gloves | 20 (74%) | 26 (72%) | 17 (89.5%) | 0.32 |
| Surgical mask | 7 (26%) | 10 (28%) | 2 (10.5%) | |
| Hand washing after seeing the patient and after removal of the gloves | ||||
| True | 23 (85%) | 27 (75%) | 15 (79%) | 0.61 |
| False | 4 (15%) | 9 (25%) | 4 (21%) | |
| Sure | 17 (63%) | 21 (58.3%) | 15 (79%) | 0.1 |
| May be | 9 (33%) | 8 (22%) | 1 (5.2%) | |
| I don’t know | 1 (4%) | 7 (19.7%) | 3 (15.8%) | |
| Go home | 2 (7.4%) | 10 (28%) | 4 (21%) | 0.11 |
| Go to staff clinic | 11 (40.7%) | 18 (50%) | 8 (42%) | |
| Do nothing | 14 (51.9%) | 8 (22%) | 7 (37%) | |
Table 8: The relation between previous infection control training and the application of infection prevention precautions of the radiology staff.
| Staff Response | Study group (n = 82) | p-value | |
|---|---|---|---|
| Yes (n = 34) | No (n = 48) | ||
| No (%) | No (%) | ||
| For every patient regardless the infectious state | |||
| True | 33 (97%) | 46 (96%) | 0.77 |
| False | 1 (3%) | 2 (4%) | |
| Department notification about isolated patient prior to transportation | |||
| True | 34 (100%) | 47 (98%) | 0.4 |
| False | 0 (0%) | 1 (2%) | |
| For isolated patient need X-ray during transportation to the department | |||
| True | 31 (91%) | 34 (91.7%) | 0.25 |
| False | 3 (9%) | 4 (8.3%) | |
| Patient with communicable disease shall be examined by the department | |||
| Immediately | 24 (71%) | 29 (60%) | 0.34 |
| At the end of the schedule | 10 (29%) | 19 (40%) | |
| Cleaning and decontamination of equipment and surfaces at the department preformed | |||
| Weekly | 11 (32%) | 17 (35.4%) | 0.001* |
| Daily | 4 (12%) | 21 (43.8%) | |
| Immediately after patient | 19 (56%) | 10 (20.8%) | |
Table 9: The relation between previous infection control training and the practice of infection prevention precautions in the radiology department.
| Staff Response | Study group (n = 82) | p value | |
|---|---|---|---|
| Yes (n = 34) | No (n = 48) | ||
| No (%) | No (%) | ||
| For patient with airborne infection, you should wear | |||
| N-95 mask | 31 (91%) | 33 (68.75%) | 0.014* |
| Surgical mask | 3 (9%) | 15 (31.25%) | |
| For patient with droplet infection, you should wear | |||
| N-95 mask | 26 (76.5%) | 25 (52%) | 0.025* |
| Surgical mask | 8 (23.5%) | 23 (48%) | |
| For patient with contact infection, you should wear | |||
| Gloves | 30 (88%) | 33 (68.75%) | 0.039* |
| Surgical mask | 4 (12%) | 15 (31.25%) | |
| Hand washing after seeing the patient and after removal of the gloves | |||
| True | 30 (88%) | 35 (73%) | 0.09 |
| False | 4 (12%) | 13 (27%) | |
| Gloves should be changed between patients | |||
| Sure | 25 (73%) | 28 (58.3%) | 0.35 |
| May be | 6 (18%) | 12 (25%) | |
| I don’t know | 3 (9%) | 8 (16.7%) | |
| After exposure to patient during examination you should | |||
| Go home | 6 (18%) | 10 (20.8%) | 0.76 |
| Go to staff clinic | 17 (50%) | 20 (41.7%) | |
| Do nothing | 11 (32%) | 18 (37.5%) | |
Discussion
Employees in radiology departments are exposed to many risks during their work especially respiratory infection[3,6]. In some hospitals, this risk may rise with the increase in patient numbers. It was also noticed that the time spent between radiology staff and the patients increase according to the type of procedure they go through. It must be remembered however that some patients might have other infectious diseases other than airborne infections, which can also be another risk to radiology staff. Such patients should be considered as well and radiology staff should be trained or at least aware of them[7,8,9].
The study had a 73% response rate with the participants categorized as: technicians 72%, nurses 13.4%, radiologists 7.3%, and others 7.3%. It is a widely held view that infection control involves knowledge, measures, and practice of guidelines adopted to protect healthcare providers and patients[9]. Thus, standard precautions of infection control are the main plan for the prevention of healthcare related infections, and are applied to all patients at any times regardless of their diagnosis. Elements of these precautions include hand hygiene and the use of appropriate personal protective equipment during contact with a patient and his products. Another problem that radiology staff may face is when a procedure is interventional nature. This might increase the risk of exposure[10]. Despite the fact that in this study around 76.8% of radiology workers had work experience < 10 years, and just 34 workers (41.5%) had previous training in infection control, their application of infection prevention precautions was fairly accepted. Although, the type and duration of training in Al Baha can be regarding as basic and less frequent in comparison to their counterparts elsewhere in the world, their compliance can be considered acceptable. Lack of infection prevention training among radiology staff in many centers worldwide was reported before in different studies and this deficiency increases the risk of exposure to infection[3,8,9,10,11].
Although this study foundthat many radiology staff had positive attitudes when dealing with patients who need respiratory precautions, some staff do not show this kind of behavior. This however should be changed and standard precautions should be applied at all times with all patients; those with or without infection[12]. Furthermore, radiology staff should inform patients about any precautions and why they must be applied[10]. This is done for their own safety, the safety of the patient, and for the safety of future patients.
Each radiology staff, according to their occupational category, have their own way of dealing with patients complaining of airborne symptoms. These results are similar to other studies[8,9]. All employees in radiology departments should be aware of hygiene requirements during daily routine procedures. Reluctance in infection prevention precautions may lead to bacterial contamination of different surfaces in the department, exposing both staff and patients to the possibility of infection[3]. Radiology workers are in direct contact with suspected or probable cases of respiratory diseases or other infectious diseases while conducting chest X-ray examinations[2,13].
The infection control experience of the department staff could play an important role in prevention of infection. Many surfaces and equipment present in radiology departments can present great challenges for effective disinfection[14]. The disinfection practices are effective in reducing or eliminating pathogens. Radiology workers should be aware of the value of disinfecting contact surfaces between patients to prevent infection transmission[4]. This study clearly found that the work experience in years was significantly related with the cleaning and decontamination of equipment and surfaces in the department. In a similar study, the more experience a radiology staff had, the better they are regarding knowledge about infection prevention[1].
With regards to the correlation between infection control training and the application of cleaning and decontamination of equipment and surfaces in the radiological department, the study found it was highly significant. Moreover, practices of infection control precautions according to the previous infection control training were significant when performed for patients with airborne, droplet, or contact precautions. Similarly, it is a finding that has also been identified in the literature. Infection control training such as hand hygiene induced significant improvement in awareness and practices among radiographers and healthcare assistants[5]. Therefore, continuing training is compulsory. On a similar note, it was reported that 94% of surveyed radiology workers needed training in the use of infection control guidelines[1]. In the Kingdom of Saudi Arabia, infection control is a rapidly growing issue so the infrastructure of this discipline is still under establishment and trying to improve[15,16].
Conclusion
This study found that the knowledge and attitude of staff working in Al Baha Radiology departments towards the application of standard precautions of infection prevention was acceptable. However, the results clearly illustrate the need for more continuous training in order to increase awareness of standard precautions and thus minimize infection exposure.
References
- 1. Antwi, W.K., AdesiKyei, K., Gawugah, J., et al. Infection Control by Radiographers during Radiological Examinations in Ghana. (2015) World J Med Res 4: 2.
- 2. Lin, Y.C., Dong, S.L., Yeh, Y.H., et al. Emergency management and infection control in a radiology department during an outbreak of severe acute respiratory syndrome. (2005) Br J Radiol 78(931): 606-611.
- 3. Buerke, B., Mellmann, A., Kipp, F., et al. Hygienic aspects in radiology: what the radiologist should know. (2012) Rofo 184(12): 1099-1109.
- 4. Hubble, W.L., Turner, J.A., Heuertz, R. Effectiveness of Current Practices for Disinfecting Medical Equipment in a Radiology Department. (2016) Radiol Technol 87(3): 250-260.
- 5. O'Donoghue, M., Ng, S.H., Suen, L.K., et al. A quasi-experimental study to determine the effects of a multifaceted educational intervention on hand hygiene compliance in a radiography unit. (2016) Antimicrob Resist Infect Control 5: 36.
- 6. Baffoy-Fayard, N., Maugat, S., Sapoval, M., et al. Potential exposure to hepatitis C virus through accidental blood contact in interventional radiology. (2003) J Vasc Interv Radiol 14(2): 173-179.
- 7. Ustünsöz, B. Hospital infections in radiology clinics. (2005) Diagn Interv Radiol 11(1): 5-9.
- 8. Reddy, P., Liebovitz, D., Chrisman, H., et al. Infection control practices among interventional radiologists: results of an online survey. (2009) J Vasc Interv Radiol 20(8): 1070-1074.
- 9. Siewert, B., Brook, O.R., Mullins, M.M., et al. Practice policy and quality initiatives: strategies for optimizing staff safety in a radiology department. (2013) Radiographics 33(1): 245-261.
- 10. Mirza, S.K., Tragon, T.R., Fukui, M.B., et al. Microbiology for Radiologists: How to Minimize Infection Transmission in the Radiology Department. (2015) Radiographics 35(4): 1231-1244.
- 11. Nyhsen, C.M., Humphreys, H., Nicolau, C., et al. Infection prevention and ultrasound probe decontamination practices in Europe: a survey of the European Society of Radiology. (2016) Insights Imaging 7(6): 841-847.
- 12. Quan, M., Wang, X., Wu, H., et al. Influencing factors on use of standard precautions against occupational exposures to blood and body fluids among nurses in China. (2015) Int J Clin Exp Med 8(12): 22450-22459.
- 13. Kim, J.S., Kim, H.S., Park, J.Y., et al. Contamination of X-ray cassettes with methicillin-resistant Staphylococcus aureus and methicillin-resistant Staphylococcus haemolyticus in a radiology department. Ann Lab Med 32(3): 206-209.
- 14. Zhang, E., Burbridge, B. Methicillin-resistant Staphylococcus aureus: implications for the radiology department. (2011) AJR Am J Roentgenol 197(5): 1155-1159.
- 15. Memish, Z.A., Zumla, A., Alhakeem, R.F., et al. Hajj: infectious disease surveillance and control. (2014) Lancet 383(9934): 2073-2082.
- 16. El Beltagy, K., El-Saed, A., Sallah, M., et al. Impact of infection control educational activities on rates and frequencies of percutaneous injuries (PIs) at a tertiary care hospital in Saudi Arabia. (2012) J Infect Public Health 5(4): 297-303.