Long Term Follow-Up In Feminine Stress Urinary Incontinence Ambulatory Surgery By Using A Single Incision Transobturator Mesh
Víctor Navalon-Monllor, Alba Monzó-Cataluña, Celia Ramada-Calaforra, Yoni PallásCosta, Pedro Navalón-Verdejo
Affiliation
Urology Department, University Hospital “Casa de la Salud”, Catholic University San Vicente Mártir, Valencia, Spain
Corresponding Author
Pedro Navalón Verdejo, Urology Department, University Hospital “Casa de la Salud”, Catholic University San Vicente Mártir, Valencia, Spain, Paseo Alameda 38- 2 46023, Valencia; E-mail: pedronavalon@yahoo.com
Citation
Pedro Navalón-Monllor, V. Long Term Follow-Up in Feminine Stress Urinary Incontinence Ambulatory Surgery by Using a Single Incision Transobturator Mesh. (2018) J Anesth Surg 5(1): 17- 21.
Copy rights
© 2018 Pedro Navalón-Monllor, V. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Stress urinary surgery; Local anesthesia; Ambulatory Surgery; Single Incision TOT
Abstract
Objective: To evaluate short and long-term results obtained from ambulatory surgical treatment of feminine stress urinary incontinence (SUI), by using a transobturator mesh (TOT) and a single Contasure-Needleless incision (Neomedic-International).
Patients and Method: Between January 2007 and December 2015, 215 patients suffering from SUI received surgery under local anaesthesia and strict ambulatory regime, by placing a Needleless suburethral sling without tension. We evaluated all the inclusion criteria and both long and short-term results. Every patient underwent a bladder stress test, a urodynamic study and a quality of life questionnaire (ICIQSF) before and after the procedure. Later, they were followed up by means of annual reviews until December 2016.
Results: Tolerance to the surgical procedure was satisfactory and duration was in all cases less than 10 minutes, hospital stay until discharge was always inferior to 2 hours. The results we obtained in short, medium and long term are comparable to the ones achieved with epidural anaesthesia. Hospitalisation and level of postoperative satisfaction was very high as well.
Conclusion: Almost all patients affected by this problem are good candidates to be included in an ambulatory surgery program, improving ostensibly cost-effectiveness without any repercussion on the quality of care or satisfaction degree and giving excellent and long-lasting results, both medium and long term.
Introduction
In light of the new theories that emerged in recent years on the pathophysiology of SUI[1-3], various surgical correction systems have been designed based on the use of tension-free slings, such as TVT (Gynecare), IVS (Tyco), Sparc / Monarc (AMS), Urotape / Optape (Porges), Uretex (Bard), etc., which use mesh of suburethral implantation[4,5]. Differences between these systems lie basically in the type of mesh selected and the access for its insertion, but all of them aim for the same purpose: to provide adequate support to the middle urethra. However, the results do not seem to depend exclusively on the surgical technique, since the characteristics of the employed mesh may be as important or more important than the technique itself[6].
Objectives
To evaluate short and long-term results, complications and security obtained from ambulatory surgical treatment of feminine stress urinary incontinence (SUI), by using polypropylene simple mesh transobturator sling (TOT) with a single Contasure-Needleless incision (Neomedic-International).
Presentation of the Contasure Needleless Sling
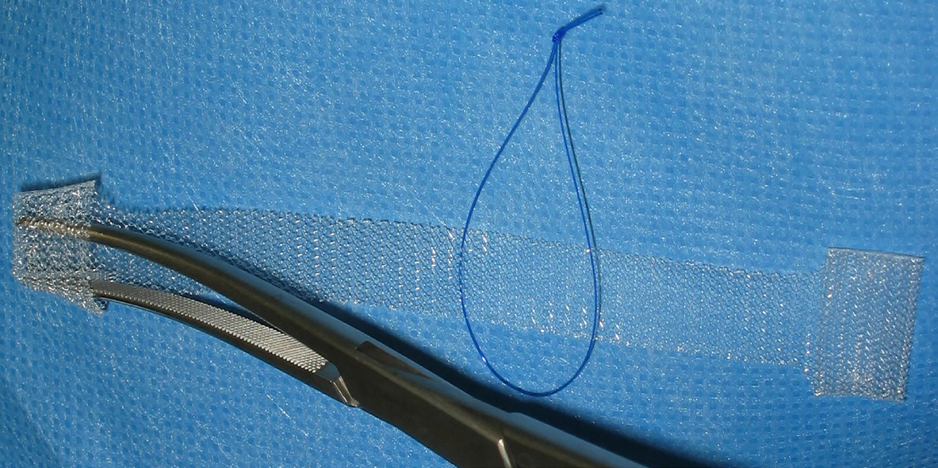
The mesh of the Contasure Needleless device is composed of monofilament polypropylene of 0.4 mm thickness, macropore (Amid I) and a porosity of 55% with dimensions of 114 mm in length and 12 mm in width, except at both ends, where they finish in a pocket-like shape with 22 mm of width (Figure 1). These pockets are of great help for the placement, support and stability of the mesh, since at first, they help to maintain the sling and later, provide greater support to the mesh as a result of the fibrosis they cause.
Figure 1: Needleless sling.
Patients and Methods
Between January 2007 and December 2015, prior approval of the Ethics Committee of our institution, we intervened of SUI by placing this suburethral sling on an outpatient basis to 215 patients aged between 42 and 85 years (mean 66,2). All patients were evaluated clinically and urodynamically, presenting a pure SUI 170 (79%) and a mixed SUI with predominance of effort the remaining 45 (21%). For the urodynamic study, a multichannel Medical Measurement System (MMS) model UP-2000 was used. Patients who presented genital, urinary or enteric concomitant prolapse that required correction in the same act were excluded. Those who had previously undergone another surgical anti-incontinence technique were included, a circumstance that occurred in 36 patients (17%); 4 of them having a history of previous TVT, 15 of TOT and 17 of sub-urethral mini-band.
Regarding the physical condition of the patients, we followed the surgical-anesthetic risk criteria of the American Association of Anesthesiologists (ASA). We included patients ASA I, ASA II and ASA III stable at the time of surgery. Thus, 43% of the patients were ASA I (93 patients), 40% (85 patients) ASA II and 17% (37) ASA III.
In all patients, the procedure was performed by the following operative sequence: Instillation of 5 cc of 2% xylocaine gel in the urethra and vagina about 30 - 40 minutes prior to the intervention. Lithotomy position not exceeding 60º bending. Placement of Foley catheter nº 18 Ch attempting to empty the bladder completely. Infiltration with local anesthetic (8-10 cc of lidocaine 2%) at 1 cm from the urethral meatus from the anterior vaginal side on both sides of the urethra, first with a thin hypodermic needle 25G and then with a 22G spinal needle that we had previously angulated to facilitate its penetration in the direction towards the obturator hole. The depth of the infiltration was of 5 to 6 cm on each side of the middle line. Incision of 10 mm in the vaginal mucosa, in the middle third sub-middle urethral, 1 cm from the urethral meatus. Dissection of the paraurethral spaces with Metzembaum scissors towards both sides (at 10 and 2 o’clock) until touching with the tip of the scissors the descending ischiopubian branch. A Pean or Bengolea clamp was placed inside the mesh pocket, making a hyperextension and closing the clamp again, trapping the mesh. The clamp was inserted with the pocket of the mesh folded in the paraurethral space until a clicking sound revealed the perforation of the internal obturator muscle. Furthermore, we proceeded to open the clamp to allow the pocket to extend leaving the Needleless mesh fixed, gently closing the clamp to extract it from the vagina without dragging the mesh. The maneuver was repeated on the contralateral side, completely inserting the mesh. However, it may still be repositioned by re-inserting the clip into the pockets of the mesh and pushing a little more. Likewise, the pressure of the mesh on the urethra may also be reduced by pulling the central thread, thus loosening the tension of the mesh. When the mesh is perfectly placed in contact with the urethra, but without tension, the central thread is removed by cutting it and pulling on one end. Suture of the vaginal mucosa, with 1 or 2 loose points of polygalactin 3/0. The Foley catheter is removed.
In all cases antibiotic prophylaxis was performed, using a single-dose regimen (cefuroxime 750 mg intravenously) prior to the surgical procedure.
The recommended postoperative treatment consisted in the administration of minor analgesics (oral magnesium metamizole, up to 2 g every 6 hours).
After the intervention, all patients remained under observation for approximately one to three hours, being discharged after spontaneous micturition and checking the absence of significant post-void residue. Postoperative controls were performed at 24 hours and a month. Subsequently, they were performed on an annual basis, in which a clinical history was carried out, an ICIQ-SF questionnaire and a physical examination with a full bladder stress test.
We consider objective cure when the patient in the physical examination performed in the consultation with a full bladder presents a negative stress test. To evaluate the subjective healing, we check the results of the ICIQ-SF questionnaire in addition to the postoperative satisfaction question, for which we used a visual analog scale.
Regarding the statistical analysis of the results, data is expressed with the mean, standard deviation and rank. The analysis was performed using the statistical package SPSS 19 (SPSS Inc., Chicago, IL). When necessary to make a comparison between means, T-Student test was used, considering statistical significance when p < 0.05. When needed to compare qualitative aspects, we used the chi-square test.
Results
We operated all patients with local anesthesia, requiring between 8 and 10 ml of 2% lidocaine anesthetic solution. In all cases, we performed additional pseudoanalgesia by perfusion of propofol and remifentanil during paraurethral dissection and insertion of the mesh.
Average time used in the surgical intervention was about 5 minutes (range 4 - 7).
After intervention, patients remained under observation for an average of 110 minutes (range 90 - 150) accompanied by a family member and controlled by nurses until they were discharged after two spontaneous micturitions. None of them required hospitalization due to immediate intraoperative or postoperative complications. In 15 patients (7%) there was discrete vaginal bleeding that was resolved by hemostatic pressure with a vaginal plug that was removed within a few minutes. Postoperative urinary retention was not observed in any case.
The mean follow-up time was 57 ± 29 months (range 12-120). The lost cases from the controls from the first postoperative year to the tenth were 3, 12, 26, 38, 45, 59, 67, 81, 90 and 98 respectively.
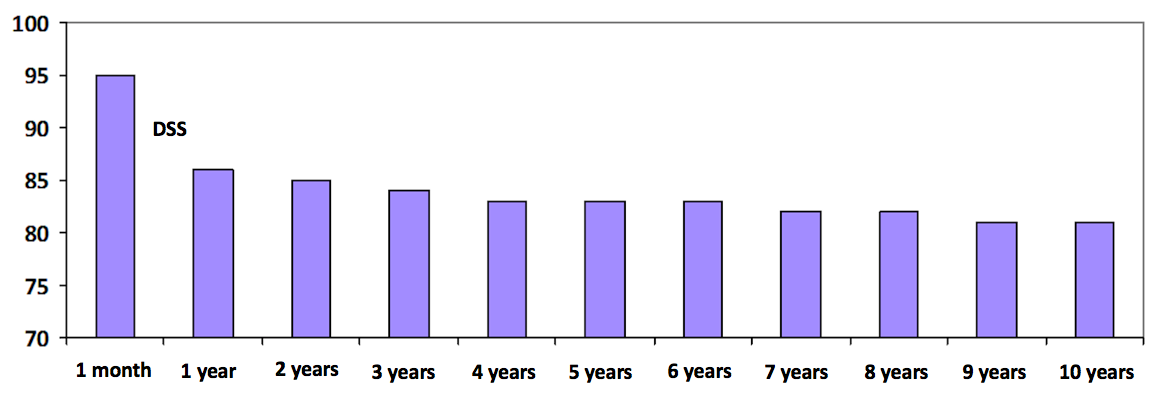
In the first review performed one month after the intervention, the objective cure rate, assessed by the exercise test, was 95% of patients; per year, the rate decreased significantly (p < 0.05) to 86%. In the following annual reviews, this rate varied between 85 and 81%, with no statistical significance for their differences.
Figure 2: Percentage of objective cures by means of stress test (DSS: statistically significant differences).
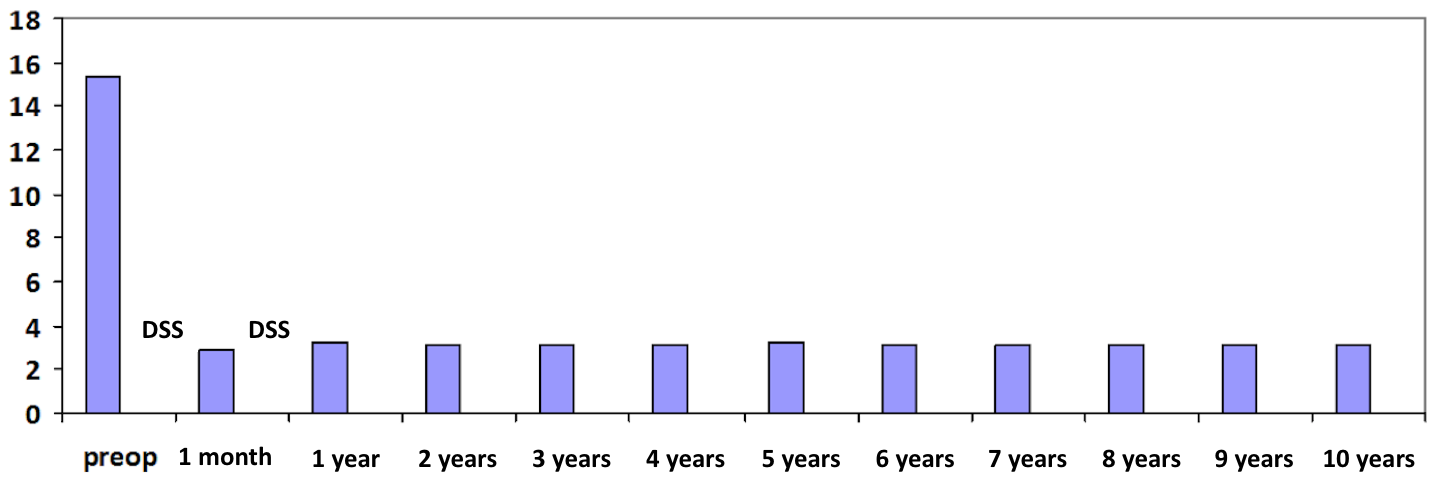
The mean score of the questionnaire on symptoms and quality of life (ICIQ-SF) made before the intervention was 15’3 ± 3’2 points, becoming significantly lower (p < 0.00001) a month later (2’ 8 ± 0.9 points). In the first-year revision, it was of 3’1 ± 1’2, being significantly higher (p < 0’05) than the previous score. In subsequent annual reviews, the mean scores of the questionnaire varied between 3’2 ± 1’3 and 3’1 ± 1’2 points, there being no statistically significant differences between them.
Figure 3: Percentage of subjective cures through the ICIQ-SF questionnaire (DSS: statistically significant differences).
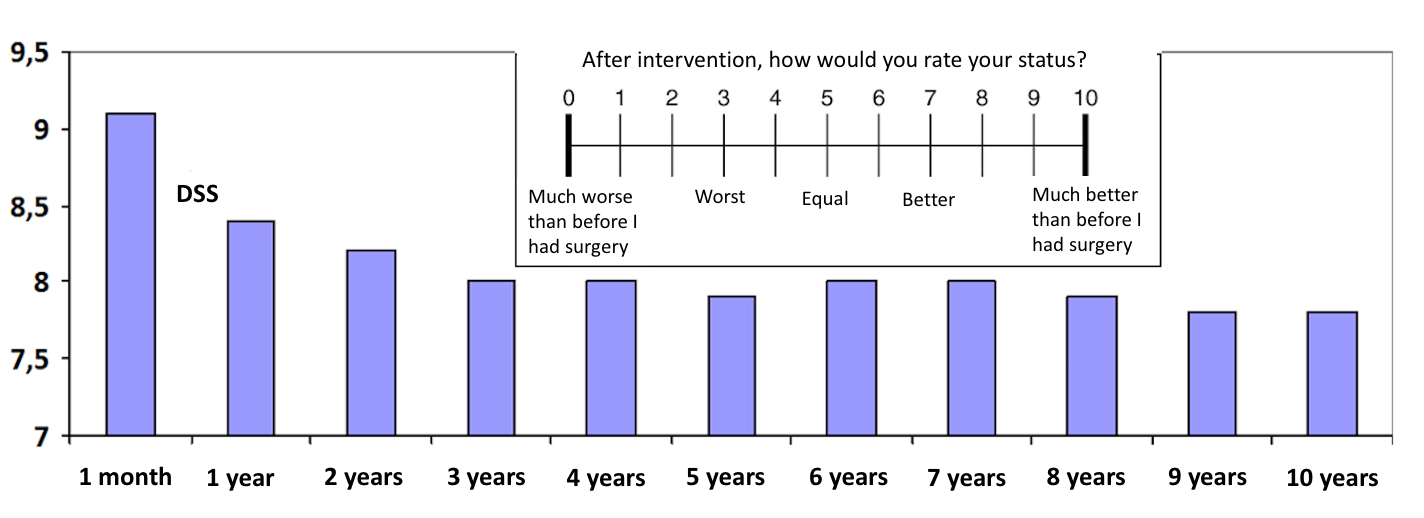
In the question about the degree of postsurgical satisfaction, which is done using the scale from 0 to 10 shown in Figure 4, where 0 corresponds to “much worse than before” and 10 to “much better than before”, the mean of values at the month of intervention was 9’1 ± 1’8. In the first year revision, it was significantly (p < 0’05) lower: 8’4 ± 2’0. In subsequent annual reviews, mean scores varied between 8’2 ± 2’1 and 7’8 ± 2’7, there being no statistically significant differences between them.
Figure 4: Degree of postoperative satisfaction through visual analog scale (DSS: statistically significant differences).
Discussion
First generation suburethral tapes were the retropubic TVT. Their long-term efficacy is proven with follow-up publications older than 10 years and in fact today it is the “gold standard” with which all other surgical techniques for stress urinary incontinence must be compared. As a result of the potential serious injuries that can occur with this technique and the possible bladder injury to the passage of needles that requires cystoscopy, in 2001 (Delorme) and 2003 (Leval) appeared the second generation ribbons with transobturator approach 5 - 8 with a lower percentage of serious injuries and obviating the need for cystoscopy. In 2006 (TVT-Secur) and 2007 (MiniArc) the third generation of ribbons emerged, in which their length was reduced by 2/3, from 20 - 21 cm to 8 - 8.5 cm[8-10].
In 2006 the Contasure Needleless sling, of Spanish patent and manufacture, emerged. They may be considered as a “hybrid” of the second (TOT) and third generation meshes (mini slings), with which it is intended to reduce the attributable complications of the passage of needles through the obturator orifice and at the same time provide a greater stability of the mesh. This is acquired by virtue of a greater length of the mesh in respect to the mini slings as well as the support that provides the termination in the form of pockets that it has at both ends, allowing their placement in a similar way to the latter since they do not require cutaneous incision, which facilitates their use in ambulatory regime[11-13].
Although in this study we have established the presence of pelvic prolapses as a criterion for exclusion of patients, since we believe that their treatment is out of the competence of outpatient surgery, the Contasure Needleless sling can be used together with other techniques of pelvic floor repair without increasing the number of complications; this combination only produces an increase in surgical time and hospital stay, and can be done safely and effectively[13-18]. Age, menopause, obesity or associated surgeries did not seem to increase risk of failure. Likewise, the history of previous performance of other anti-incontinence surgeries did not seem to influence the results or complications[19-22] and in our experience, we also did not find greater difficulty in the surgical technique.
As a local anesthetic, we prefer lidocaine to other amidic compounds (mepivacaine, bupivacaine and ropivacaine), since it has less cardiotoxic effect in case of direct entry of the anesthetic to the vascular torrent, has a faster anesthetic action and is the one that causes a less painful sensation during its infiltration[23]. We also prefer its use because it is the same compound that has the xylocaine gel that has previously been applied to the patient in the urethra and vagina about 30 - 40 minutes before the intervention to anesthetize the mucous membranes. It has the disadvantage of causing a shorter anesthetic action time than the rest, but usually it is short-term interventions that in our experience have always been less than an hour, and in no case, have we had to repeat the infiltration due to depletion of the anesthetic effect before finalizing the intervention.
Regarding the degree of mesh tension that should remain suburethrally, we consider inappropriate the idea suggested by some authors to invite the patient to cough during the surgical act after filling the bladder with saline to adjust the mesh until it ceases to have urine leakage during the Valsalva maneuver[24] since the lithotomy position is not the ideal one for its evaluation, for its correct verification, this test would have to be practiced in standing position. The placement of TVT tapes or TOT tapes is recommended to interpose the surgical scissors between the band and the urethra to avoid direct contact between both. Adjustment of the Needleless Contasure is done by leaving the mesh in direct contact with the urethra, but trying to keep it without tension. We also believe that it is preferable to leave the mesh with little tension (running the risk of early recurrence of incontinence, easily solved by interposing another mesh in a second procedure) than applying excessive tension leaving the patient hypercorrelated with the consequent side effects due to obstruction of the lower urinary tract. Thus, in our experience, most of recurrences occurred during the first year of follow-up, is probably a consequence of the insufficient tension applied to the mesh to avoid the side effects of overcorrection. However, in subsequent follow-ups, once the fibrosis and stability of the sling is established, the rates of objective and subjective cures as well as the degree of postsurgical satisfaction remain constant, with our long-term results being superimposable to those published for conventional sling procedures performed with hospital admission and under general or spinal anesthesia[13,20,25].
Regarding the discussion raised by some authors about the use or not of urethrovesical catheter and vaginal tamponade during the postoperative period after the placement of the mesh, we consider its systematic use unnecessary. We believe that the risk of hemorrhage and hematoma is practically non-existent with this type of meshes and in opposition causes a more uncomfortable and annoying postoperative. Thus, in our experience, only 15 patients (7%) had discrete vaginal bleeding resolved by haemostatic pressure with a vaginal plug that was removed within a few minutes.
Conclusion
Practically all patients suffering from stress urinary incontinence are candidates to be included in an outpatient surgery program, ostensibly improving the cost-effectiveness ratio, not diminishing the quality of care or the degree of satisfaction and providing excellent and long-lasting results, both medium and long term.
References
1. Ulmsten, U., Henrikson, L., Johnson, P., et al. Ambulatory surgical procedures under local anesthesia for treatment of female urinary incontinence. (1996) Int Urogynecol J Pelvic Floor Dysfunct 7(2): 81-85.
2. Petros, P., Ulmsten, U.I. An integral theory of female urinary incontinence. Experimental and clinical considerations. (1990) Acta Obstet Gynecol Scand Suppl 153: 7-31.
3. Patel, A.K., Chapple, C.R. Urodynamics in the management of female stress incontinence-which test and when? (2008) Curr Opin Urol 18(4): 359-364.
4. Navalón, P., Zaragoza, C., Ordoño, F., et al. Tratamiento quirúrgico ambulatorio de la incontinencia urinaria de esfuerzo femenina. (2005) Arch Esp Urol 58 (9): 915-924.
PubMed||Crossref||Others
5. Delorme, E. Transobturator urethral suspensión: miniinvasive procedure in the treatment of stress incontinence in women. (2001) Prog Urol 11(6): 1306-1313.
PubMed||Crossref||Others
6. Galmés, B.I., Díaz, G.E. ¿Son iguales todos los sistemas empleados para corregir la incontinencia urinaria mediante mallas libres de tensión? (2004) Actas Urol Esp 28(7): 487-496.
7. Pardo Schanz, J., Ricci Arriola, P., Tacla Fernández, X., et al. Cinta trans-obturadora (TOT) en la corrección de la incontinencia de orina de esfuerzo. Experiencia de tres años con 200 pacientes. (2007) Actas Urol Esp 31(10): 1141-1147.
PubMed||Crossref||Others
8. Jimémez Calvo, J., Hualde, A., Raigoso, O., et al. Our experience whit mini tapes (TVT Secur and Miniarc) in the surgery for stress urinary incontinence. (2008) Actas Urol Esp 32(10): 1013-1018.
9. Solá, V., Ricci, P y., Pardo, J. Malla sub-medio uretral de tercera generación: Experiencia con 110 TVT-Secur. (2009) Arch Esp Urol 62(5): 376-388.
PubMed||Crossref||Others
10. Jiménez Calvo, J., Hualde, A., Cebrián, J.L., et al. Nuestra experiencia con minicintas MiniArc en la cirugía de la incontinencia urinaria de esfuerzo. (2010) Actas Urol Esp 34(4): 372-377.
PubMed||Crossref||Others
11. Navazo, R., Moreno, J., Hidalgo, C., et al. Contasure Needleless: TOT de una sola incisión para el tratamiento de la incontinencia de orina de esfuerzo. (2009) Arch Esp Urol 62(9): 719-723.
PubMed||Crossref||Others
12. Navalón, V., Navalón, P., Pallás, Y., et al. Outpatient. surgical treatment of female stress urinary incontinence under local anesthesia-sedation with contrasure needleless incision. (2014) Actas Urol Esp 38(1): 49-54.
13. Amat, L., Martínez Franco, E., Lailla, J.M. Contasure Needleless compared with transobturator-TVT for the treatment of stress urinary incontinence. (2011) Int Urogynecol J 22(7): 827-833.
14. Rezapour, M., Novara, G., Meier, P.A., et al. A 3 month preclinical trial to assess the performance of a new TVT-like mesh (TVTx) in sheep model. (2007) Int Urogynecol J Pelvic Floor Dysfunct 18(2): 183-187.
15. Nambiar, A., Cody, J.D., Jeffery, S.T. Single-incision sling operations for urinary incontinenci in women. (2014) Cochrane Database Syst Rev (6): CD008709.
16. Nambiar, A., Cody, J.D., Jeffery, S.T., et al. Single-incision sling operations for urinary incontinence in women. (2017) Cochrane Database Syst Rev 7: CD008709.
17. Ford, A.A., Rogerson, L., Cody, J.D., et al. Mid-urethral sling operations for stress urinary incontinence in women. (2015) Cochrane Database Syst Rev (7): CD006375.
18. Ford, A.A., Rogerson, L., Cody, J.D., et al. Mid-urethral sling operations for stress urinary incontinence in women. stress urinary incontinence in women. (2017) Cochrane Database Syst Rev 7: CD006375.
19. Palmieri, S., Frigerio, M., Spelzini, F., et al. Risk factors for stress urinary incontinence recurrence after single-incision sling. (2018) Neurourol Urodyn
20. Jiménez-Calvo, J., Montesino-Semper, M., Hualde-Alfaro, A., et al. Tratamiento de la incontinencia urinaria de esfuerzo femenina con minicintas Miniarc: Resultados a 4 años. (2015) Actas Urol Esp 39(1): 47-52.
PubMed||Crossref||Others
21. Song, P., Wen, Y., Huang, C., et al. The efficacy and safety comparison of surgical treatments for stress urinary incontinence: A network meta-analysis. (2018) Neurourol Urodyn
22. Escribano, G., Hernández, C., Subirá, D., et al. Incontinencia urinaria de esfuerzo femenina. Corrección quirúrgica con técnicas de cabestrillo pubovaginal”. (2002) Arch Esp Urol 55: 1093-1105.
PubMed||Crossref||Others
23. Navalón, P., Pallás, Y., Navalón, V., et al. “A Twelve-Year Experience in Ambulatory Surgery within Urology. (2012) ISRN Urology 2012: 383642.
24. Gutierrez, J.L., Martín, B., Portillo, J.A., et al. Utilidad de la determinación de la presión abdominal de fuga en el diagnóstico de la incontinencia de orina femenina en la época del TVT. (2004) Actas Urol Esp 28(7): 506-512.
PubMed||Crossref||Others
25. Natale, F., Illiano, E., La Penna, C., et al. Mixed urinary incontinence: A prospective study on the effect of trans-obturator mid-urethral sling. (2017) Eur J Obstet Gynecol Reprod Biol 221: 64-69.