Magnitude of Pre-Lacteal Feeding Practice and Associated Factors among Mothers having Children Less than 2 Years of Age in Fitche Town, North Showa, Ethiopia
Dejene Hailu Beyene, Zeleke Argaw Menji
Affiliation
1Mizan Tepi University School of Nursing, Ethiopia
2Jimma University school of nursing and Midwifery, Ethiopia
3Addis Ababa University collage of Health Science School of Nursing and Midwifery, Ethiopia
Corresponding Author
Admasu Belay Gizaw, Jimma University School of nursing and Midwifery Office, P.O. Box: 378, Ethiopia, Tel: 251925270512; E-mail: admasu2004@gmail.com
Citation
Gizaw, A.B., et al. Magnitude of Pre-Lacteal Feeding Practice and Associated Factors among Mothers having Children Less than 2 Years of Age in Fitche Town, North Showa, Ethiopia. (2018) Lett Health Biol Sci 3(1): 12- 19.
Copy rights
© 2018 Gizaw, A.B. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Infant feeding practice; Pre-lacteal feeding; Fitche town
Abstract
Background: Pre-lacteal feed is food and/or fluid provided to a new-born before initiating breastfeeding. Initiation of complementary feedings before six months can lead to displacement of breast milk which may increase risk of infections such as diarrhoea, weight loss and malnutrition. This study was aimed to assess magnitude of pre-lacteal feeding practice and associated factors.
Methods: Community based cross-sectional study was conducted among mothers having children less than two years by using systematic sampling technique. Interviewer administered structured questionnaires were used to collect data then interred in to EPI data version 3.1. Finally the data was exported to SPSS version 22 for analysis. Descriptive statistics and logistic regression were done. P-value of less than 0.05 was taken as statistically significant.
Results: The magnitude of pre-lacteal feeding practice was 24.4%. The common type of prelacteal feeding was plain water; 39(12.2) followed by butter; 25(7.8%). Those mothers who didn’t get counselling on breast feeding were seven times more likely practice pre-lacteal feeding compared to those who were counselled (AOR: 7.07 (95% CI: 1.67, 29.88)). Mothers who are not knowledgeable about risk pre-lacteal feeding were 8.56 times more likely practice prelacteal feeding compared to knowledgeable mothers (AOR: 8.56 95% CI: 2.65, 27.64).
Conclusion: About one fourth of mothers (24.4%) practice pre-lacteal feeding which makes breastfeeding practices sub-optima at the study area. Absence of counselling on breast feeding and being not knowledgeable about the risk of prelacteal feeding was significantly associated with pre-lacteal feeding practice among the study participants.
Introduction
Starting breastfeeding in the first one hour after birth can reduced risk of neonatal morbidity and mortality and improve maternal health outcomes[1]. Giving pre-lacteal feeds is a key factor for early termination of full breastfeeding which can affect infant and childhood health status[2]. Study results revealed that, more than 80% of neonates receive breast milk across the globe, but only about half began breastfeeding within the first hour of life in contrast to WHO recommendations[2] Breastfeeding is the most important factors of child survival, birth spacing, and the prevention of childhood illness and infections. The positive effects of breastfeeding depend on its initiation, duration, and weaning time[3].
Oxford and Mariam Webster dictionaries defined pre-lacteal as feed that is given to a new-born infant before the mother has begun to breastfeed. It is a major barrier to exclusive breastfeeding[4] which is the cornerstone of adequate infant nutrition. Despite different interventional measures acknowledged by Baby Friendly Hospital Initiative (BFHI) of in ensuring optimal infant nutrition, pre-lacteal feeding within the first day of life is still a common problem[4].
Across many countries pre - lacteal feeding is a common cultural practice can be considered as an important factor late initiation of breast feeding. These delays the milk let down reflex and could contribute to lactation failure[5]. Despite the demonstrated benefits of breast milk, the prevalence of breastfeeding, in particular exclusive breastfeeding in many developing countries including in our country is lower than the international recommendations[6].
The increased problem of under nutrition in the first two years of life suggests problems of poor infant feeding practices. Adequate nutrition is essential for children’s health and development since growth during the first year of life is very crucial. Breast milk provides immunologic protection against morbidity and mortality from diseases like diarrhoea, respiratory infections, otitis media, pneumonia and meningitis[7,8].
Pre - lacteal feeding is a common practice which is prevalent in almost all the communities throughout the World invariably of any background, belief and nation. Mostly, it is established as a tradition in different communities and treated as a part of culture. Study done in Indian revealed mental, physical and medical conditions of mothers during postnatal period affects infant feeding practice in addition to culture[8].
Worldwide about 4,000 infants and young children die daily due to diarrhoea and pneumonia secondary to poor practice of breast feeding. From these deaths, more than two folds are among 0 - 5 month old infants. It was associated with having repeated infections, slow growth and increases death among 2 - 28 days infant six times than children who receive early breast milk[9,10]. Inappropriate feeding practices causes more than 35% of deaths in children less than five years of age of which more than two-thirds occur during the first year of life[11]. A result of study in Nepal showed 26.5% were provided with Pre-lacteal feeding[1].
It is also common practice in Indian subcity like; Tamilnadu = 14.85%, pure block of Jammu and Kashmir = 88%, 48%, Pondicherry 42.7 % and Maharashtra and Luck now city 50.6% [3,12-15]. Study done in Egypt at Mansoura also showed about 58% of new born initiated pre - lacteal feeds before breast.
Evidences revealed that, sugar or glucose water (39.6%), infant formula (28.6%), and herbs (21.7%) are commonly given as pre - lacteal feedings. Tradition (61.0%) and poor maternal advice (58.3%) are reported as the most common reasons[16].
Report from developing countries showed, early initiation of breastfeeding minimizes death due to diarrheal disease and lower respiratory tract infections and saves about 1.45 million lives each year[17,18]. A cross sectional descriptive study done on Slum Children revealed most of the mothers (84%) gave pre-lacteal feedings[19].
Study done in Nigeria revealed that more than one third (38.8%) of mothers gave pre-lacteal feeding for their infants[20,21] another study conducted in Harari showed (45.4%) of mothers gave pre-lacteal feedings for their infants[22]. In Ethiopia, diarrhoea is a major contributor of illness and death among young infants and children, particularly in urban areas, due to inappropriate breastfeeding and pre-lacteal feeding practice[23].
Although pre-lacteal feeding is widely practiced in Ethiopia, extent of the problem and contributing factors were not well investigated in the study area. Therefore, the purpose of this study was to determine the magnitude and associated factors of pre-lacteal feeding practice among mothers having children less than two years of age in Fitche town, North show Ethiopia.
Materials and Methods
Study area and period: The study was conducted at Fitche Town the capital city of North Shewa Zone of Oromia National Regional State. Fitche is found at 115 km from Addis Ababa on the way to Gojam. The town has four kebeles. Based on central statistical agency in 2010 the town has the total population of 39,910 where 18,774 are male and 21,136 are female. 8832 of them are women of reproductive age group (15 - 49), 6,558 are under five children and 2,276 are children less than two years of age. Each kebele has three urban Heath Extension Workers. The town has one hospital, two health centers, 6 private health institutions and 6 drug stores. The studies was conducted from February1 to March 1, 2016.
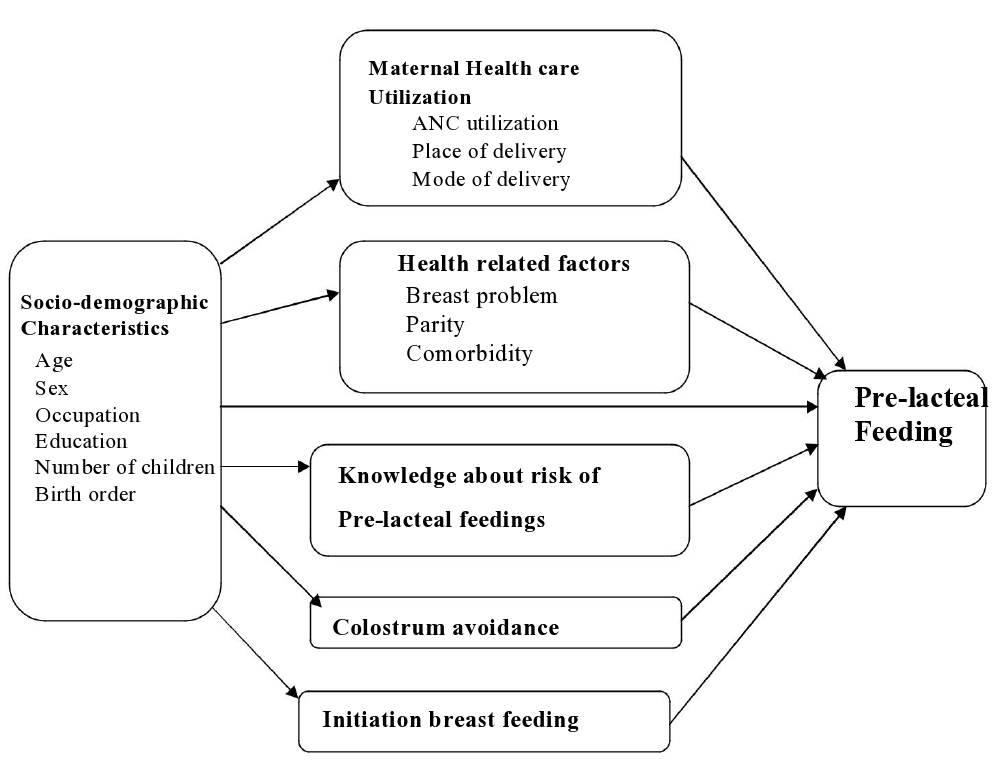
Figure 1: Conceptual framework developed after review of literatures on assessment of pre-lacteal feeding practice and associated factors among mothers having children less than two years[3,14,24,27,33].
Study Design: Community based cross - sectional study was conducted.
Source population: Mothers having children less than two years of age living in Fitche town were the source population.
Study population: Mothers having children less than two years and living in the selected kebeles.
Inclusion and Exclusion criteria
Inclusion criteria: Mothers having children less than two years of age and who stayed more than six months in the town.
Exclusion criteria: Mothers who were seriously ill, mental problem (unable to communicate).
Sample Size Determination
The sample size was determined by the formula used to estimate a single population proportion and using 17.0% prevalence (17) and 5% margin of error with 95% confidence level.
n = (zα/2)2p (1 - p) = (1.96)20.17(1 - 0.17) = 217
d2 (0.05)2
Where, Z = Standard normal variable at 95% confidence level (1.96), p = Estimated proportion of pre - lacteal feeding (17%) d = margin of error (5%)
Since, the population was less than 10,000 correction formulas was used
nf = n * N / n + N = 217 * 2276/217 + 2276 = 198
Where, N = the target population = 2276, n f = 218 after considering 10% for non-response rate. Finally design effect was taken into consideration then the final sample size was 1.5 * 218 = 327
Sampling procedure
The town has 4 kebeles and each of the two kebeles was selected randomly by lottery methods from the existing four kebeles. In order to obtain the sample size from each 2 kebeles proportional allocation to sample size was done. Participating households from the selected Keble’s was identified using systematic sampling technique from the urban HEWs registry book as sampling frame. Finally every Kth mother from each house hold of the two Kebeles was identified until the required sample size fulfilled and the starting household was selected using a lottery method.
Study variables
Dependent variable: Pre-lacteal feeding
Independent variables
Socio-demographic characteristics
Health care service utilization
Health related factors
Knowledge about risk associated with pre-lacteal feedings
Colostrum avoidance
Initiation time of breast feeding
Data collection instruments
The data collection instrument was adapted from different national and international literatures[38,40] then modified and contextualized to the local situation. The English version questions was translated into ‘Afan Oromo’ and ‘Amharic’ then back translated into English by fluent speakers of both ‘afan Oromo and Amharic’ languages to check its consistency. The instrument has three parts; the first part contains socio demographic characteristics, the second part contains infant feeding practice and the third part contains factors influencing pre-lacteal feeding.
Data collection procedure
Face to face interview using structured questionnaires was used to collect data. Two days training was given for data collectors to ensure completeness and consistency of information during data collection. Three diploma and one senior BSc nurses were recruited for data collection process.
Data quality assurance
The pre-test was conducted on 5% of the sample size at kebele 01 to check accuracy, clarity and to determine the length of time needed for interview. After review of the instruments all suggested revision was made prior to actual data collection. The investigator and supervisor checked all questionnaires from each data collectors on spot. Short term meeting and discussion was undertaken to ensure that all the information was properly collected.
Data processing and analysis
Data was entered into EPI data version 3.1, cleaned and exported to IBM SPSSversion 22 for analysis. Descriptive statistics were used to describe socio-demographic characteristics of the study variables. Bivariate and multivariable logistic regression was done to see the statistical association between dependent and independent variables. P-values less than 0.05 were considered as statistically significant and Adjusted Odds Ratio (AOR) with 95% Confidence Interval to measure the strength of the associations.
Ethical consideration
Ethical clearance was assured from Addis Ababa University, College of health science department of nursing and midwifery institutional ethical review Board and supportive letter was written to Fitche town health Bureau then permission letters was obtained from Fitche town health bureau. Finally, informed consent was obtained from study participants to confirm their willingness for participation after explaining the objective of the study. The respondent was notified that they have the right to refuse or terminate at any point of the interview and as information provided by each respondent was kept confidential.
Results
Socio demographic characteristics
Among 327 mothers the investigator planned to conduct interview, 320 agreed to participate resulting a response rate of 97.9%. Out of the total respondents 100 (31.3%) were in the age range of 25 - 29 years 11 (3.4%) had age less than 19 years. The mean age of 29.31 (±5.8) years and the rest were as shown on table 1. Regarding marital status majority 241(75.3%) of them were married. Concerning family size, 156 (48.8%) of them had 4 - 5 children and the rest 125 (39%) and 39 (12.2%) had 3 and less and 6 and above children. One fourth of them (79 (24.7%)) cannot read and write; 220 (68.8%) orthodox Christians religion followers and the rest are protestant and muslimsa. 221(69.1) Oromo and the remaining are Amhara, gurage and Tigray. Concerning study participants occupation, 73 (22.8%) were civil servant, 66 (20.6%) trader, 60 (18.8%) of them were house wife, and the rest were daily labourer, private employee, farmers and student. One hundred forty four (45.0%) of them had monthly income of 500 - 1000 (local currency). The mean age of infants was 12 months with (SD ± 6.9) months (Table 1).
Table1: Socio-demographic characteristics among mothers having children less than 2 years of age in Fitche town, North Shewa Ethiopia, 2016 (N = 320).
| Socio-Demographic variables | F | % |
|---|---|---|
| Age of mothers | ||
| < 19 | 11 | 3.4 |
| 20 - 24 | 57 | 17.8 |
| 25 - 29 | 100 | 31.3 |
| 30 - 34 | 81 | 25.3 |
| 35 - 39 | 58 | 18.1 |
| > 39 | 13 | 4.1 |
| Family size | ||
| <= 3 | 125 | 39.0 |
| 4 - 6 | 156 | 48.8 |
| > 6 | 39 | 12.2 |
| Marital Status | ||
| Single | 22 | 6.9 |
| Married | 241 | 75.3 |
| Divorced | 34 | 10.6 |
| Widowed | 23 | 7.2 |
| Educational Level | ||
| Cannot read and write | 79 | 24.7 |
| Can read and write | 48 | 15.0 |
| Grade 1 - 8th | 66 | 20.6 |
| Grade 9 - 12th | 50 | 15.6 |
| College diploma and above | 77 | 24.1 |
| Religion | ||
| Orthodox | 220 | 68.8 |
| Protestant | 69 | 21.5 |
| Muslim | 31 | 9.7 |
| Ethnicity | ||
| Oromo | 221 | 69.0 |
| Amhara | 69 | 21.6 |
| Gurage | 23 | 7.2 |
| Tigre | 7 | 2.2 |
| Occupation | ||
| Student | 11 | 3.4 |
| Private employee | 40 | 12.5 |
| Civil servant | 73 | 22.8 |
| Daily Labourer | 47 | 14.7 |
| Trader | 66 | 20.6 |
| Farmer | 23 | 7.2 |
| House wife | 60 | 18.8 |
| Income | ||
| < 500 | 49 | 15.3 |
| 500 - 1000 | 144 | 45.0 |
| 1001 - 1500 | 30 | 9.4 |
| >= 1500 | 97 | 30.3 |
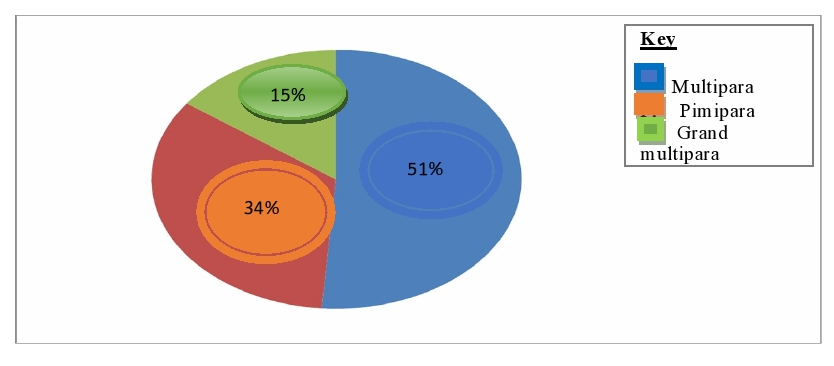
Out of the total respondents one 108 (33.8%), 164(51.2%) and 48 (15.0%) were Pimipara, Multipara and grand multipara mothers respectively (Figure 2).
Figure 2: Parity status among mothers having chi1dren less than 2 years of age, in Fitche town, North shewa Ethiopia, 20l6 (n = 320).
Health care service utilization
Regarding maternal health care service utilization, 267(83.4%) mothers were attending ANC and among these 130(40.6%) utilized ANC two to three times and followed by; 124 (38.8%) utilized greater than or equal to four ANC. Majority, 250 (78.1) got breast feeding Counselling during ANC follow-up in which 169 (52.8%) counselled on the benefits of breast feeding and 125 (39.1%) on exclusive breast feeding. Regarding place of delivery, 235 (73.4%) delivered their child at governmental health facility, 266(83.1%) with spontaneous vaginal delivery and 250 (78.1%) delivery was assisted by health care professionals (Table 2).
Table 2: Health care service utilization among mothers having children less than 2 years ofage at Fitche town, North shewa, Ethiopia, 2016 (N = 320).
| Variables | Frequency (N = 320) | Percentage (%) |
|---|---|---|
| Attending antenatal care | ||
| Yes | 267 | 83.4 |
| N0 | 53 | 16.6 |
| Utilization of Antenatal care | ||
| 1 times | 13 | 4.0 |
| 2 - 3 times | 130 | 40.6 |
| >= 4 times | 124 | 38.8 |
| Get breast feeding | ||
| Yes | 250 | 78.1 |
| No | 70 | 21.9 |
| Place of Delivery (N = 320) | ||
| Governmental facility | 235 | 73.4 |
| Private clinic | 15 | 4.7 |
| At Home | 48 | 15.0 |
| TBAs place | 22 | 6.9 |
| Mode of Delivery (N = 320) | ||
| C/S delivery | 48 | 14.4 |
| Spontaneous delivery | 266 | 83.1 |
| Instrumental delivery | 8 | 2.5 |
| Delivery attendants | ||
| Health professionals | 250 | 78.1 |
| Traditional birth attendants | 70 | 21.9 |
Infant feeding practice
Out of 320 who had ever breastfed their child, 78 (24.4%) were reported as they are giving pre-lacteal feeds within the first three days. The most common types of pre-lacteal feeding were plain water 39 (12.2%), butter 25 (7.8%), Cow milk 17 (5.3%), Sugar with water 14 (4.4 %), water 10 (3.1%) and formula milk 9 (2.8 %).
The major Reason for pre-lacteal feeding were; cultural practice 35 (10.9%), for cleaning of infants bowel, throat and mouth 33 (10.3%) and 32 (10%) gave pre-lacteal feeding for child growth. Study participant reported that advice of giving pre-lacteal feeding was from Grandparents traditional birth attendants and mothers own decision. Majority of mothers 248 (77.5%) gave colostrum for their infants within the first five days after delivery and only 72 (22.5%) of them avoid.
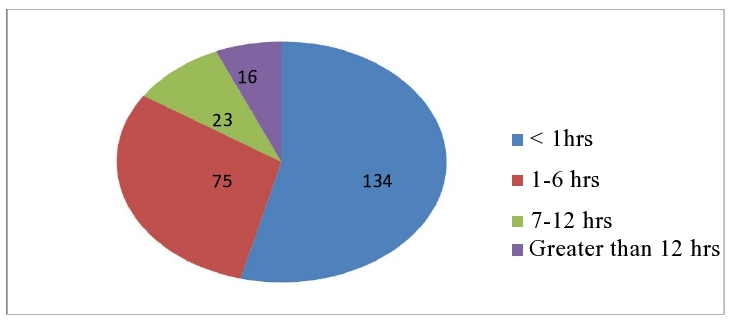
Out of the respondents who feed colostrum; 134 (41.9 %) mothers was initiated breast feeding in the first hour and the rest 75 (23.4%) were initiated within one to six hours after delivery.
In this study only 118 (36.9%) mothers know the Disadvantages of pre-lacteal feeding and the rest 202 (63.1%) of mothers did not report any disadvantages. One hundred ninety 190 (59.4 %) mothers had knowledge on the risk with pre-lacteal feeding whereas the rest 130 (40.6%) of mothers didn’t have knowledge on risk with pre-lacteal feeding. List of problems mentioned by the study participant due to pre-lacteal feeding include diarrhoea 116 (36.3%), infection 110 (34.4%), poor growth 127 (39.7%) and vomiting 100 (31.3%) (Figure3).
Figure 3: Breast feeding initiation among mothers having children less than 2 years of age in Fitche town, North shewa Ethiopia, 2016 (N = 248).
Table 3: Pre-lacteal feeding practices among mothers having children less than 2 years of agein Fitche town, North shewa Ethiopia, 2016 (N = 320).
| Variables | Frequency | Percentage (%) |
|---|---|---|
| Pre-lacteal feeding | ||
| Yes | 78 | 24.4 |
| No | 242 | 75.6 |
| Types of pre-lacteal feedings | ||
| Plain water | 39 | 12.2 |
| Sugar or Glucose water | 14 | 4.4 |
| Cow milk | 17 | 5.3 |
| Water and ‘tenadam ‘(rue) | 10 | 3.1 |
| Butter | 25 | 7.8 |
| Formula milk | 9 | 2.8 |
| Total | 78 | 24.4 |
Factors associated with pre-lacteal feeding practice
The binary logistic regression analysis showed that level of education, breast feeding counselling, delivery attendant; Knowledge of about disadvantage of pre-lacteal feeding were statistically associated with pre-lacteal feeding. Mothers whose educational level were primary and secondary were 2.32 (95% CI: 1.01, 5.32), 5.80 (95% CI: 2.35, 14.29) times more likely to give pre-lacteal feedings as compared to those mother who were college and above level of education respectively. Mothers who didn’t get breast feeding counselling were 8.14 (95% CI: 4.51, 14.68) times more likely give pre-lacteal feedings as compared to those mothers who got breast feeding counselling. Mothers whose delivery was assisted by traditional birth attendants were 4.42 (95% CI: 2.50,7.82) times more likely practice pre-lacteal feeding as compared to delivery assisted by health professionals. Mothers who know the purported pre-lacteal feeding advantage were 2.7 (95% CI: 1.60, 4.56) times more likely practice pre-lacteal feeding as compared to those mothers who didn’t know the advantages of PLF. Mothers who didn’t have knowledge on risks associated with pre-lacteal feeding were 5.93(95% CI: 3.41, 10.32) times more likely give pre-lacteal feeding as compared to those mothers who had knowledge on risks associated with pre-lacteal feeding. In multivariable logistic regression analysis mothers who didn’t counselled on breast feeding and not knowledgeable about risks associated with pre-lacteal feeding were statistically significantly associated with pre-lacteal feeding practice. Mothers who didn’t get breast feeding counselling were 7.07 (95% CI:1.67,29.88) times more likely give pre-lacteal feeding than those who did got breast feeding counselling. Mothers who didn’t have knowledge on the risks associated with pre-lacteal feeding were 8.56 (95% CI: 2.65,27.64) times more likely give pre-lacteal feeding practice as compared to those mothers who had knowledge on the risks of pre-lacteal feeding (table 5).
Table 4: Knoweldge of mothers having children less than 2 years of age on pre-lactealfeeding in Fitche town,North Shewa Ethiopia, 2016 (N = 320).
| Variables | Frequency | Percentage (%) |
|---|---|---|
| Disadvantages of pre-lacteal feedings | ||
| Yes | 118 | 36.9 |
| No | 202 | 63.1 |
| Knowledge on risk with PLF | ||
| yes | 190 | 59.4 |
| No | 130 | 40.6 |
| Information about problems of PLF | ||
| Diarrhea | 116 | 36.3 |
| Poor growth | 127 | 39.7 |
| Infection | 110 | 34.4 |
| Vomiting | 100 | 31.3 |
Table 5: Factors associated with pre-lacteal feeding practices among mothers having childrenless than 24 months of age in Fitche town, North Shewa, Ethiopia, 2016.
| Variables | Pre-lacteal feeding | Crude OR | Adjusted OR | |
|---|---|---|---|---|
| Yes (%) | No (%) | (CI: 95%) | (CI: 95%) | |
| Level of education | ||||
| Illiterate | 29 (36.7) | 50 (63.3) | 1.28 (0.60,2.74) | 0.39 (0.07,2.17) |
| Able to read and write | 15 (31.3) | 33 (68.8) | 1.67(0.82,3.42) | 0.27 (0.47,1.60) |
| Primary education | 17 (25.8) | 49 (74.2) | 2.32 (1.01,5.32)⃰ | 0.31 (0.06,1.50) |
| Secondary education | 10 (20.0) | 40 (80.0) | 5.80 (2.35,14.29)⃰ | 0.35 (0.05,2.35) |
| College and above | 7 (9.1) | 70 (90.9) | 1 | 1 |
| Place of delivery | ||||
| Health facility | 43 (55.1) | 207 (85.5) | 1 | 1 |
| Home | 35 (44.9) | 35 (14.5) | 4.81 (2.72,8.53)⃰ | 0.62 (0.01,83.07) |
| Breast feeding counseling | ||||
| Yes | 37 (47.4) | 213 (88.0) | 1 | 1 |
| No | 41 (52.6 | 29 (12.0) | 8.14 (4.51,14.68)⃰ 7.07 (1.67,29.88)⃰ | |
| Delivery attendant | ||||
| Health professionals | 44 (56.4) | 206 (85.1) | 1 | 1 |
| TBAs | 34 (43.6) | 36 (14.9) | 4.42 (2.50,7.82) | 5.07 (0.04,72.84) |
| Disadvantages of pre-lacteal feedings | ||||
| Yes | 52 (66.7) | 61 (25.2) | 2.70 (1.60,4.56)⃰ | 0.75 (0.25,2.27) |
| No | 26 (33.3) | 181 (74.8) | 1 | 1 |
| Knowledge on risk associated with pre-lacteal feedings | ||||
| Yes | 32 (41.0) | 158 (65.3) | 1 | 1 |
| No | 46 (59.0) | 84 (34.7) | 5.93 (3.41,10.32)⃰ 8.56 (2.65,27.64)⃰ | |
Discussion
The study result showed as the magnitude of pre-lacteal feeding was among the study populations were 24.4%. This makes breastfeeding practices sub-optimal due to additional feeds. This finding is lower when compared with Ethiopian Demographic and Health Survey that reported 27% and consistent with different region (21.9%), (25.2%), (23.4%) and (25.6%) in Oromia region, Addis Ababa city, Benishangul Gumuze region and Tigray region, respectively[24,25,38]. The similarity might be due to common cultural practice, relatively similar methods of maternal counselling at health institutions and knowledge levels of mothers. The finding is also similar with study in Nepal in which prevalence of prelacteal feeding was (26.5 %)[1]. This might be due to age category of study participants and cultural similarities among the two countries.
The study result showed magnitude of pre-lacteal feeding among the study participant is lower compared with study conducted Raya Kobo district (38.8%), Harari regional state (45.4%) and West Gojam zone (48.3%) respectively[24]. This may be due to duration so the study and study setting in which study in these three areas include both urban and rural community.
Lack of breast feeding counselling and knowledge on risk of pre-lacteal feeding practice were positive predictors of pre-lacteal feeding practice. Those mothers who didn’t counselled on Breast feeding were seven times more likely practice pre-lacteal feedings compared to those mothers who got counselling (AOR:7.07;95% CI:1.67, 29.88). This result is consistent with study done in Vietnam[33] and Maharashtra India in which it was reported as pre-lacteal practices are found to be more among the respondents who did not receive counselling about the breast feeding as compare to those who received[14].
This study showed that mothers who didn’t have knowledge on risk associated with pre-lacteal feeding were 8.56 times more likely practice pre-lacteal feeding as compared to those mothers who knows the risks associated with pre-lacteal feeding (AOR:8.56;95% CI:2.65,27.64). This is consistent with study done in Raya Kobo district; North Eastern Ethiopia and in Vietnam that reports feeding Pre-lacteal practice decreased with increased breastfeeding knowledge[27,36,37]. The reason for the mother to provide the pre-lacteal feeding practice were cultural practices, receiving advice from family members especially grandmothers, the maternal belief that pre-lacteal feeding was used to clean mouth, throat and bowel and also keeps it as moisture.
The other possible explanation may be lack of Antenatal care services, not supporting about breast feeding at health facility (lack of breast feeding counselling) may affect the maternal knowledge and attitude towards early initiation of breast feeding and exclusive breast feeding.
Conclusion
The result of this study showed that almost one out of four mothers (24.4%) gave pre-lacteal feedings for their new born baby who makes breastfeeding practice sub-optimal and can increase child morbidity and mortality in the study area. The most common type of pre-lacteal feedings is plain water followed by butter. The major reason for providing pre-lacteal feeding were cultural practice, for cleaning of infant’s bowel, throat and mouth and for child growth. Lack of breast feeding counselling and knowledge of mothers about the risk of prelacteal feeding were identified as factors associated with pre-lacteal feeding practices.
Recommendations
Effective Breast feeding should be promoted by all health care sectors in the zone and there should be plan for health information dissemination to bring behavioural change at all household, community, health facility, regional and national levels by focusing on reduction of pre-lacteal feedings. Need to work on promoting behavioural change and increase awareness of mothers about risks associated with prelacteal feeding during ANC, FP and postnatal care services. Interventions should be considered grandparent and Traditional birth attendant in the community. Health care workers should take training on the dangers of giving pre-lacteal feedings. Health care professionals working at the town should provide appropriate counselling on breast feeding for the mothers during ANC follow up, postnatal delivery, immunization and family planning.
Competing Interests: All authors declare there is no conflict of interests.
Author’s Contribution
Dejene Hailu initiated the study, contributed to the study design, coordinated the data collection process and analysed the data. Zeleke Argaw contributed to the study design, reviewed survey instruments, participated on data analysis and commented on the manuscript. Admasu Belay contributed to the study design, survey instrument development, and data analysis and wrote the manuscript. All authors read and approved the final manuscript.
Acknowledgments: I would like to extend my sincere gratitude to all my friends and family members who supported in all aspects of my academic success and for all study participants!
References
- 1. Debes, A.K., Kohli, A., Walker, N., et al. Time to initiation of breastfeeding and neonatal mortality and morbidity: a systematic review. (2013) BMC Public Health 13(3): 19.
- 2. Sobhy, S.I., Mohame, N.A. The effect of early initiation of breastfeeding on the amount of vaginal blood loss during the fourth stage of labour. (2004) J Egypt Public Health Assoc 79 (1–2): 1-12.
Pubmed||Crossref||others
- 3. Victora, C.G., Bahl, R., Barros, A.J., et al. Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect.(2016) Lancet 387(10017): 475-490.
- 4. Mahmood, S.E., Srivastava, A., Shrotriya, V.P., et al. Infant feeding practices in the rural population of north India. (2012) J FAM Community Med 19(2): 130-135.
- 5. Khanal, V., Adhikari, M., Sauer, K., et al. Factors associated with the introduction of prelacteal feeds in Nepal : findings from the Nepal Demographic and Health Survey 2011. (2013) Int Breastfeed J 8(1): 9.
- 6. Yotebieng, M., Chalachala, J.L., Labbok, M., et al. Infant feeding practices and determinants of poor breastfeeding behavior in Kinshasa, Democratic Republic of Congo: a descriptive study. (2013) Int Breastfeed J 8 (1): 11.
- 7. Ibadin, O.M., Ofili, N.A., Monday, P., et al. Prelacteal feeding practices among lactating mothers in Benin City, Nigeria.(2013) Niger J paed40(2): 139-44.
Pubmed||Crossref||others
- 8. Kanagasabapathy, S., Muthukumar, S. Pre lacteal feeding practice among rural mothers in Tamilnadu-A questionnaire based study. (2015) Int J Biomed Adv Res 6(06): 484-487.
- 9. Alemayehu, T., Haidar, J., Habte, D. Determinants of exclusive breastfeeding practices in Ethiopia. (2009) Ethiop J Health Dev 23(1): 12-18.
Pubmed||Crossref||others
- 10. Sriram, S., Soni, P., Thanvi, R., et al. Knowledge, attitude and practices of mothers regarding infant feeding practices. (2013)Natl J Med Res 3(2): 1-4.
Pubmed||Crossref||others
- 11. Gosvami, A. Analytical study of prevalent and traditional prelacteal feeding practices and their relevance. (2009) Indian J Prev Soc Med 40(3): 219-224.
Pubmed||Crossref||others
- 12. Infant and young child feeding. (2004) FMOH-E.
Pubmed||Crossref||others
- 13. Community-Based Sub-Component of Ethiopian National Nutrition Program. (2009) Baseline Survey Report.1-76.
Pubmed||Crossref||others
- 14. Raina, S.K., Mengi, V., Singh, G. Determinants of Prelacteal Feeding Among Infants of RS Pura Block of Jammu and Kashmir, India. (2012) J Fam Med Prim Care 1(1): 27-29.
- 15. Prasad, K.N. Profile of Pre Lacteal Feeding, Exclusive and Continued Breast Feeding Practices among Families in Rural Community of Pondicherry. (2015) Sch Acad J Biosci 3(6): 509-514.
Pubmed||Crossref||others
- 16. Dawal, S., Inamdar, I.F., Saleem, T., et al. Study of Pre Lacteal Feeding Practices and its Determinants in a Rural Area of Maharashtra. (2014) Sch J Appl Med Sci 2(4): 1422-1427.
Pubmed||Crossref||others
- 17. Beyene, T.T. Predictors of Nutritional Status of Children Visiting Health Facilities in Jimma Zone, South West Ethiopia. (2012) Int J Adv Nurs Sci Pract 1(1): 1-13.
Pubmed||Crossref||others
- 18. Gupta, P., Srivastava, V.K., Kumar, V., et al. Pre-lacteal feeding practices among newborn in urban slums of Lucknow city UP, India. (2012) Open J Prev Med 2(4): 510-513.
- 19. Abdel-hady, D.M. Abdel-Hady, E. G. Newborn First Feed and Prelacteal Feeds in Mansoura, Egypt. (2014) Biomed Res Int: 1-7.
- 20. Hailemariam, T.W., Adeba, E., Sufa, A. Predictors of early breastfeeding initiation among mothers of children under 24 months of age in rural part of West Ethiopia.(2015) BMC Pub H15: 1076.
- 21. Akhtar, K., Haque, M.E., Islam, M.Z., et al. Feeding Pattern and Nutritional Status of Under Two Years Slum Children. (2012) J Shaheed Suhrawardy Med Col 4(1): 3-6.
- 22. Acoecpnoi, C., Maduforo, A.N., O NK. Infant Feeding Practices among Mothers and Their Infants Attending Maternal and Child Health in Enugu, Nigeria. (2014) J Biol Agric Health 4(10): 130-139.
Pubmed||Crossref||others
- 23. Bekele, Y., Mengistie, B., Mesfine, F. Prelacteal Feeding Practice and Associated Factors among Mothers Attending Immunization Clinic in Harari Region Public Health Facilities, Eastern Ethiopia. (2014) Open J Prev Med 4(7): 529-534.
- 24. Kebede, Z. Determinants of Optimum Breastfeeding among Mothers of Child Less than Two Years in Bishoftu Town, East Shewa Zone of Oromia Region, Ethiopia. (2015) Sci J Public Heal 3(4): 544-551.
- 25. Khanal, V., Lee, A.H., Karkee, R., et al. Prelacteal Feeding of Newborns in Post conflictTimor-Leste. (2014) JPGN 59(2): 162-166.
Pubmed||Crossref||others
- 26. Ramesh, K., Kumar, K.P. Student PG, Medicine C. Knowledge and Attitude of Post Natal Mothers Towards Breast Feeding in A Tertiary Care Hospital , Bellary , Karnataka.(2014) Med Sci 3(4): 368-370.
- 27. Shaili, V., Parul, S., Kandpal, S.D., et al. A community based study on breastfeeding practices in a rural area of Uttarakhand. (2012) Natl J Community Med 3(2): 283-287.
Pubmed||Crossref||others
- 28. Yadavannavar, M.C., Shailaja, S.P. Socio cultural factors affecting breast feeding practices and decisions in rural women.(2011) Int J Plant, Anim Environ Sci 1(2): 46-50.
Pubmed||Crossref||others
- 29. Nguyen, P.H., Keithly, S.C., Nguyen, N.T., et al. Prelacteal feeding practices in Vietnam : challenges and associated factors. (2013) BMC Public Health13: 932.
- 30. Adetunji, O., Joseph, A., Olusola, E., et al. Pre-Lacteal Feeding Practices of Doctors and Nurses in a State and Teaching Hospital in Western Nigeria : A Cause for Concern. (2006) Internet J Nutr Wellness 3(1): 1-5.
Pubmed||Crossref||others
- 31. Kokebie, T., Aychiluhm, M., Degu, G. Community Based Essential New Born Care Practices and Associated Factors among Women in the Rural Community of Awabel District, East Gojjam Zone, Amhara, Ethiopia. (2013) Int J Adv Sci Res 2015; 01(01): 17- 27.
- 32. Sandor, M., Dalal, K. Influencing factors on time of breastfeeding initiation among a national representative sample of women in India. (2013) Health 5(12): 2169-2180.
- 33. Kumar Anil Obulareddy, R., Narreddy, R.R. Study on breast-feeding practices among urban and rural women in Kakinada. (2015) Int J Res Heal Sci (1): 66-70.
Pubmed||Crossref||others
- 34. Devang Raval, Jankar, D.V., Singh, M.P. A study of breast feeding practices among infants living in slums of Bhavnagar city, Gujarat, India. (2011) Healthline: 2(2).
Pubmed||Crossref||others
- 35. Knowledge and belief regarding pre-lacteal feeding in relation to educational status of rural areas in Aligarh. (2006) Indian J Prev Soc Med 37(3): 3-7.
Pubmed||Crossref||others
- 36. Memon, S., Shaikh, S., Kousar, T., et al. Assessment of infant feeding practices at a tertiary care hospital. (2015) J Pak Med Assoc 60(12): 1010-1015.
- 37. Gupta, R.K., Nagori, G. A study on changing trends and impact of ante-natal education and mother’s educational status on pre-lacteal feeding practices. (2012) J Pharm Biomed Sci 19(19): 2011-3.
Pubmed||Crossref||others
- 38. Fadnes, L.T., Engebretsen, I.M.S., Wamani, H., et al. Infant feeding among HIV-positive mothers and the general population mothers : comparison of two cross-sectional surveys in Eastern Uganda. (2009) BMC Public Health 14: 1-14.
- 39. Ethiopia Demographic and Health Survey 2011. Addis Ababa, Ethiopia and Calverton, Maryland, USA: Central Statistical Agency and ICF International. (2012) Central Statistical Agency [Ethiopia] and ICF International.
Pubmed||Crossref||others
- 40. Nutritional baseline survey report for the national nutrition program of Ethiopia. (2010)EHNR.
Pubmed||Crossref||others
- 41. Ethiopia Demographic and Health Survey 2011. (2012) Central Sta Age Addis Ababa, Ethiopia ICF.
Pubmed||Crossref||others