Metastatic Sarcoma: A rare case of left ventricular outflow tract obstruction
Erica Okene, Ankit Parikh , Michael R. Clay , Robinson Williams
Affiliation
Department of Medicine, Emory University, School of Medicine, Division of Cardiology, Atlanta, GA
Corresponding Author
Stephen D. Clements Jr. M.D, Department of Medicine, Emory University School of Medicine, Division of Cardiology, Atlanta, GA. Tel: 404-778-2898; Fax: 404-778-5490; E-mail: sclemen@emory.edu
Citation
Clements, S.D., et al. Metastatic Sarcoma: a rare case of left ventricular outflow tract obstruction. (2015) J Heart Cardiol 1(1): 10-11.
Copy rights
©2015 Clements, SD. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License
Keywords
Sarcoma; Left ventricular outflow tract; CT scan; Echocardiogram
Abstract
We present a patient with cardiac involvement by a metastatic high-grade pleomorphic sarcoma. The tumor metastasized to the endocardium of the left ventricle as well as the lungs, adrenal glands, and thoracolumbar spine. The sarcoma obstructed the left ventricular outflow tract. Approximately 5 months after diagnosis, despite chemotherapy, our patient died suddenly. The exact cause of death is unknown, but presumably cardiac in origin
Introduction
Cardiac tumors, both metastatic and primary, are uncommon in the general population with frequencies ranging from 0.0017% and 0.33%[1]. The complications of cardiac tumors include: obstruction of blood flow and disturbance of valve function; local invasion causing arrhythmias; tamponade from pericardial effusion; peri-tumoral thrombus or tumor fragment embolization. Patients may be asymptomatic or present with a variety of symptoms including dyspnea, fever, malaise, weight loss, and chest pain. These may overlap with those seen with advanced malignancy[2]. Approximately 95% of cardiac tumors are metastatic[1]. When these tumors are present, a high index of suspicion is required for complete diagnosis[1]. Although resection can be an effective operative treatment for patients with primary cardiac tumors, it is much less feasible for patients with metastatic tumors to the heart[2].
Patient Presentation
A 32-year old man-initially presenting with fatigue, anorexia, weight loss, chills and fever-was diagnosed as having undifferentiated high-grade pleomorphic sarcoma involving the upper right thigh. A grade III/IV systolic murmur was described at the right sternal border. Aside from dyspnea on exertion, our patient had no additional cardiac symptoms at presentation.
At our institution, further immunohistochemical analysis including pancytokeratin, S-100 protein, and CD34 was negative-showing no evidence of differentiation. Hematoxylin and eosin (H&E) stained sections from the right thigh specimen showed sheets and poorly formed fascicles of pleomorphic cells. Entrapment of mature adipocytes was present (Figure 1A). The tumor cells were spindled to ovoid in shape and had hyperchromatic centrally located nucleoli (Figure 1B). Overall, the findings were those of an undifferentiated pleomorphic sarcoma (formerly malignant fibrous histocytoma).
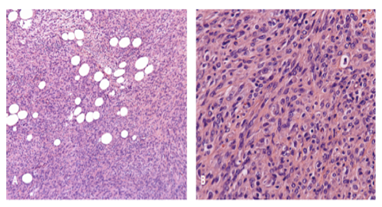
Figure 1: A Hematoxylin and eosin stained tissue, 200x magnification. Fascicles of pleomorphic cells displaying fat entrapment with no indication of specific differentiation. B Hematoxylin and eosin stained tissue, 400x magnification. Moderate pleomorphism of ovoid-shaped cells with irregular nuclear contours, hyperchromasia, and prominent central nucleoli.
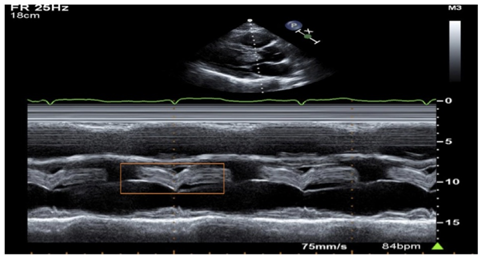
Transthoracic echocardiography (TTE) demonstrated a normal-sized left ventricle with a large fleshy mass involving left ventricular cavity that extended into the left ventricular outflow tract (LVOT) (Figure 2). The mass had its origin laterally from the anterolateral papillary muscle area toward the base of the mitral annulus. A portion of the mass freely prolapsed into the LVOT just below the aortic valve (Figure 3A). The echocardiogram also revealed that the mass measured at least 5.8 by 7.2cm. The diameter of the LVOT measured by echo from the two-dimensional parasternal long axis view to be 75% narrowed by the tumor. The left ventricular ejection fraction (LVEF) was normal at 60% and the calculated peak instantaneous gradient by continuous wave Doppler across the LVOT and aortic valve area was an estimated 40-45 mmHg. There was early systolic closure of the aortic valve and systolic fluttering of the valve leaflets after the early closure. A negative filling defect was present in the LVOT on color Doppler (Figure 3B). CT scan confirmed a large mass projecting into the left ventricular cavity (Figure 4A) and revealed the origin to be the endocardium the anterolateral and posterior lateral walls at the base of the heart (Figure 4B).
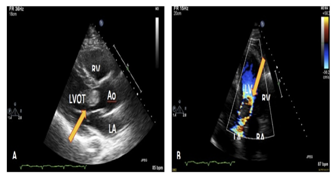
Figure 3: A Two-dimensional TEE in peristernal long axis view displays mass extended from the anteriolateral papillary muscle area to the LVOT. B Apical 4-chamber, two-dimensional TEE displays mass narrowing the LVOT by 75%. Doppler imaging displays negative filling defect in the LVOT.
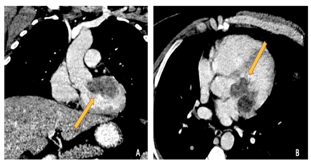
Figure 4: Computed tomography (CT scan) displaying A Mass attached to anterolateral wall and extending into the LVOT. B Five chamber view displaying mass projecting into the left ventricular cavity and extending into the LVOT. In this view, the mass is demonstrating the origin from the posterior wall.
Our patient showed clinical improvement after chemotherapeutic treatment with gemcitabine and docetaxel. This improvement continued until 5 cycles of treatment with chemotherapy, when pain in lumbar and shoulder region was investigated with CT scan and revealed extensive metastasis to adrenals and spine. The left ventricular soft tissue mass was unchanged.
Since treatment had been exhausted, our patient received palliative radiation care and expired 5 months after the diagnosis.
Discussion
Metastatic tumors to the heart, as seen with our patient is 20-40 times more common than primary cardiac tumors and are often incurable[3,4]. For this diagnosis, a high index of suspicion is needed. From an overall perspective, tumors of the lung and breast are the most common to metastasize to the heart[5]. Melanoma has the greatest tendency to metastasize to the heart; however, sarcoma also has this tendency along with renal, hepatic, adrenal and thyroid malignancy[5]. Metastatic tumors to the heart tend to show preference to the pericardium, epicardium, and myocardium in that order[6]. Endocardial metastasis, as observed in our patient, is rare –accounting for 3-5% of all cardiac metastases found in autopsy and can potentially obstruct inflow or outflow areas[6,7]. Our patient showed metastasis to the endocardium of the left ventricle and subsequently obstructed the LVOT of the left ventricle.
Conclusion
Our patient is one of the very few recorded in literature with metastasis of an undifferentiated sarcoma to the endocardium. Although secondary cardiac tumors are more common than primary cardiac tumors, they can rarely be treated by operative intervention[8]. Our patient had advanced-stage sarcoma at presentation with widespread metastasis. Symptoms from cardiac involvement depend on the location, the type of tumor, and the extent of the lesion[9]. When the endocardium is exclusively involved, cardiac symptoms may not be present until embolization or obstruction of inflow or outflow occurs[9]. In the late stages his condition, our patient became cachectic. Since the patient was at home when he passed, we cannot be certain of the exact cause of death. We can only speculate the patient suffered from some additional LV outflow obstruction, a malignant arrhythmia or tumor embolization.
Our patient presented with a rare undifferentiated sarcoma originating in the left thigh and metastasizing to the endocardium of the left ventricle, and subsequently obstructing the LVOT. He died suddenly some 5 months after identification of the cardiac involvement, illustrating the unfavorable prognosis of this rare and unusual condition.
References
- 1. Petris, A.O., Alexandrescu, D.M., Cosatche, II. Cardiac tumors. (2014) Rev Med Chir Soc Med Nat lasi 118(2): 289-292.
- 2. Agaimy, A., Rosch, J., Weyand, M., et al. Primary and metastatic cardiac sarcomas: a 12-year experience at a German heart center. (2012) Int J Clin Exp Pathol 5(9): 928-938.
- 3. Silverman, N. Primary Cardiac Tumors. (1980) Ann Surg 191(2): 127-138.
- 4. Fairman, E.B., Mauro, V.M., Cianciulli, T.F., et al. Liposarcoma causing left ventricular outflow tract obstruction and syncope: a case report and review of literature. (2005) Int J Cardiovasc Imaging 21: 513-518.
- 5. Kassop, D., Donovan, M.S., Cheezum, M.K., et al. Cardiac Masses on Cardiac CT: A Review. (2014) Curr Cardiovasc Imaging Rep 7(8): 9281.
- 6. Goldberg, A.D., Blankstein R., Padera, R.F., Tumors Metastatic to the Heart. (2013) Circulation 128: 1790–1794.
- 7. Son, J., Hong, G., Unusual Left Ventricular Endocardial Metastasis from Primary Lung Cancer. (2012) J Cardiovasc Ultrasound 20(3): 157–160.
- 8. Hornick, J.L., Bosenburg, M.W., Mentzel, T., et al. Pleomorphic liposarcoma: clicopathologic analysis of 57 cases. (2004) Am J Surg Pathol 28(10): 1257-1267.
- 9. Tong, E.C.K., Rubenfeld, S. Cardiac metastasis from myxoid liposarcoma emphasizing its radiosensitivity(1968). Am J Roentgenol Radium Ther Nucl Med 103: 792-799.