Modelling and Supporting Complex Behavior Change Related to Obesity and Diabetes Prevention and Management with the Compensatory Carry-over Action Model
Affiliation
- 1Jacobs Center on Lifelong Learning and Institutional Development (JCLL), Health Psychology, Jacobs University Bremen, Germany
- 22Bremen International Graduate School for Social Sciences, Bremen, Germany
Corresponding Author
Sonia Lippke, Health Psychology, Jacobs University Bremen gGmbH, Campus Ring 1, 28759 Bremen,Germany, Tel: +49-421-200-4730; Fax: +49-421-200-49-4730; E-Mail: s.lippke@jacobs-university.de
Citation
Lippke, S. Modelling and Supporting Complex Behavior Change related to Obesity and Diabetes Prevention and Management with the Compensatory Carry-over Action Model (2014) J Diabetes Obes 1(2): 39- 43.
Copy rights
© 2014 Lippke S. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Diet, Eating behavior; Food intake; Multiple behavior change; Physical activity; Exercise
Abstract
Diabetes and obesity directly related to an imbalance between energy intake and energy expenditure, namely, a healthy lifestyle. Physical activity and diet can prevent excess body weight and obesity, and help to manage diabetes. To guide prevention and management of diabetes and obesity more efficiently, this paper introduces a new theory, which explicitly models different health behaviors in unison.
The Compensatory Carry-Over Action Model (CCAM) proposes five axioms for modeling different health behaviors: (1) Different health behaviors (in this case, physical activity and nutrition) are interrelated, and they are driven by (2) emotionally relevant higher- level goals. (3) Each single behavior needs to be intended; this intention translated into behavior via planning, and the process is moderated by self-efficacy. (4) Carry-over mechanisms enable inter-behavioral learning, and compensatory cognitions can facilitate but also hinder the execution of both behaviors. (5) The outcome can result in the reduction of the stress response and the increase of well-being.
There is little previous research on the CCAM's assumptions, which necessitates further investigations. Likewise, the evidence- and theory-based axioms should guide interventions targeting obesity and diabetes, as well as many other health challenges and diseases. Prevention and management of diabetes and obesity can become more efficient when using the CCAM for designing and evaluating interventions.
Introduction
Health behavior change related to diabetes and obesity
Being obese is the main risk factor for many diseases, such as cancer, coronary heart disease, diabetes, skeletal disease and stroke. Both diabetes and obesity are directly related to an imbalance between energy intake and energy expenditure[1,2]. Lifestyle changes consisting of regular physical activity and a balanced diet can prevent or reduce excess body weight and obesity[3]. Therefore, designers of interventions should take both of these behaviors and their antecedents into account[4-6].
However, there is a lack of theoretical understanding of such multiple and complex behavior interrelations like physical activity and diet, which can explain past problems with changing those different behaviors[3,7]. Thus, the purpose of this paper is to contribute to the understanding and facilitation of both physical activity and healthy eating together, and thus help to prevent or manage obesity and diabetes more effectively.
A new theory on healthy lifestyles and complex behavior change
There is currently initial evidence on how behaviors interrelate[8,9]. However, this evidence exists mainly with regard to modelling and changing single behaviors. For single behaviors, it has been found that social-cognitive factors play a key role[10,11]. Thus far, we know rather little about the mechanisms of multiple health behavior change (MHBC). At present, only parts of MHBC have been modeled in theories, and comprehensive theories are still missing[12]. Such comprehensive theories should model mechanisms that drive different behaviors, such as energy expenditure (i.e. physical activity) and energy intake (i.e. nutrition) in unison; though, little systematic knowledge is currently available about such mechanisms in practice. In the following, this paper outlines a novel theory, with the aim to close this gap.
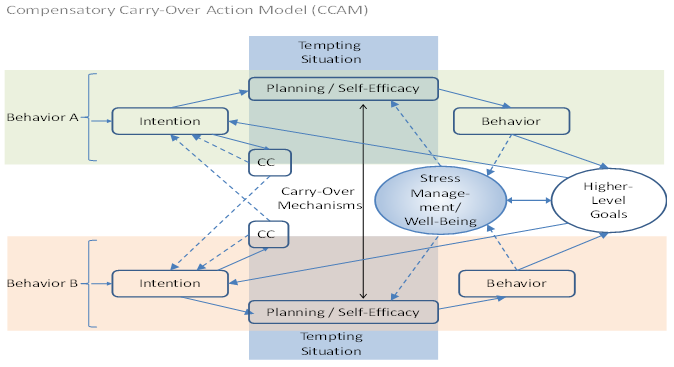
The Compensatory Carry-over Action Model (CCAM, Figure 1) integrates state-of-the-science research: It combines different social-cognitive factors for single health behaviors, which in turn facilitate multiple single behaviors. These social- cognitive assumptions on single behaviors stem from the Health Action Process Approach (HAPA)[13], which results in the CCAM consisting of self-efficacy, intention and plans (Figure 1, and section below). In addition, the CCAM models multiple health behavior change the mechanisms such as carry-over mechanisms and compensatory cognitions (Figure 1, and section below). Furthermore, higher-level goals or so-called life goals[14,15] are assumed to drive the different single behaviors (Figure 1, and section below), and finally, the different behaviors influence stress-management and well-being, which in turn influence individuals' planning and self-efficacy beliefs (Figure 1).
Figure 1: The Compensatory Carry-Over Action Model. CC = Compensatory Cognition.
Behavior A = physical activity, non-smoking, detection behavior such as feet checking, or blood sugar tests etc. Behavior B = nutrition, moderate/no alcohol consumption, or medical compliance etc.
Specifically, the CCAM predicts that each single behavior change starts with the formation of a regarding intention (e.g., "I intend to be physically active three times a week for 30 minutes or longer"). This intention must be translated into plans (e.g., "I have precisely planned when, where and how I will be physically active") also known as implementation intentions[16]. If plans are specific in terms of what to do in certain situations and in the face of potential barriers, individuals can eventually execute their intentions and plans more automatically. This also improves goal pursuit and makes performance of the behavior more likely[17].
Self-efficacy, which refers to one's belief in their own ability to do something in face of barriers (e.g., "I am capable of adopting an activity schedule in spite of inner temptations") is another important factor that determines goal pursuit and behavior performance[18,19]. However, many people face problems when pursuing health goals, which are often a consequence of other health behaviors. It is therefore important to pay attention to inter-behavioral aspects, such as compensatory cognitions and carry-over mechanisms, and to higher-level goals, which are both drivers of single behaviors (Figure 1, and section below).
Compensatory cognitions
The assumptions of compensatory cognitions stem from the Compensatory Health Beliefs Model[20]. Compensatory Health Beliefs can exist in all individuals (such as other beliefs like attitudes) and can be activated if an intention failed to be translated into behavior, or as justification for unhealthy behaviors. This activation can happen either prior to the actual situation in which the behavior should be enacted (as reasoning for not doing it), or afterwards (as an explanation for unfulfilled goals, also known as dissonance).
Compensatory Cognitions (CC) emerge if individuals perceive a discrepancy between their intentions (e.g., perform physical activity three times a week) and their actual behavior performance (e.g., performing physical activities only one time per week[20]). Dissonance is a perception, which people try to reduce by cognitive or behavioral actions. Cognitive dissonance reductions could lead to adjust the intention "three times a week" to "one time per week". At the same time, CCs can have an effect on subsequent complex behavior performance: For example, a diabetes patient received the recommendation to perform daily physical activity and not eat any candy any more, but has huge difficulties with both behaviors. Then the CC "if I have performed my daily physical activity I can eat a little candy" might help to adopt the physical activity behavior. After some time, he might experience that physical activity results in positive experiences and that candy is not needed any more to trigger the physical activity behavior.
In other words, CCs can function as intentions, post-hoc explanations or subjective beliefs. CCs can be measured by items like, for example, "One might compensate for not exercising as planned by exercising later on" or "One can make up for too little physical activity with eating healthier". CCs can determine when and how people act in accordance with their intentions or not, and what the possible psychological consequences are. For example, the above described diabetes patient had originally formed the intention to eat no candy and to be physically active every day for 30 minutes or more. During the first 2 weeks, he could only manage to get physically active by rewarding himself with candy, which is opposing the intention not eating candy, but in accordance with his CCs that eating unhealthy can compensated by physical activity. However, maintaining the intention not eating candy helps him to alter the rewarding stimuli of the candy with the reward by the physical activity itself like feeling more relaxed or happy. In previous studies, CCs found to correlate positively with risk behaviors and symptoms[20-22], to determine self-regulation failure and lower goal-attainment[23]. In addition, CCs have been associated with fewer health behaviors and motivational stage movements[22].
This clearly indicates that previous research on CCs exists; however, it faces two major problems. Firstly, correlational research might have overlooked non-linear patterns, i.e. medium CCs might have a positive effect on behavior enactment (like in the example with the candy, after the first 2 weeks candy eating could be given up); whereas too high CCs hinder it (in the example with the candy if the CCs would block the intention to eat no candy and consequently, only physical activity would be changed but candy eating would be maintained over time instead of giving this risk behavior up). Secondly, past studies have not investigated whether CCs work specifically and depending on the individual's motivation and previous behaviors (cf. Table 1). CCs can be harmful if they cause individuals to give up an intention. Nevertheless, theoretically CCs can also set the stage for a new intention and the relevant behavior (dotted lines in Figure 1). Therefore, the CCAM theorizes CCs as unique factors with specific functions (see Table 1).
Table 1: Prediction of the impact of compensatory cognitions (CCs) under the condition
| - | No previous Behavior B | Previous Behavior B |
|---|---|---|
| No previous Behavior A | If CCs are (too) high: undermining the intention and goal attainment - i.e. no behavior change in both domains (Behavior A and B) | If CCs are (too) high: effective for behavior B maintenance, but behavior A is not performed |
| Previous Behavior A | If CCs are (too) high: effective for behavior A maintenance; but behavior B is not performed | If CCs are (too) high: both behaviors are at risk of being discontinued |
Behavior A and Behavior B are not adopted yet, or have been performed before but not habituated.
Note. Behavior A=physical activity, non-smoking, detection behavior such as feet checking, or blood sugar tests etc. Behavior B=nutrition, moderate/no alcohol consumption, or medical compliance etc.
If the aim of a MHBC intervention is to optimize two or more behaviors at a time (e.g., nutrition and physical activity), it is imperative to (1) prevent CCs from leading to giving up the formed intention (e.g., nutrition), and to (2) foster medium CCs regarding another behavior (e.g., activity) - which actually facilitate both behaviors. By doing so, these CCs should be or become as specific as possible (like plans). Only then, will individuals make use of their CCs and adopt a new behavior. Thus, it is important to monitor that people translate their CCs into compensatory behavior via intentions and plans. Theoretically, this can achieved by forming a new intention, as modelled in the CCAM (see Figure 1, dotted lines). This assumption, however, has not received sufficient attention in the past research and future research needs to examine it systematically.
Carry-Over mechanisms
Other factors that work specifically in the volitional processes of health behavior change are Carry-Over Mechanisms (COM) between different behaviors. COM are also known as Transfer[24,25] or Spill-Over[26]. One can measure COM as a mechanism carrying over resources from one domain to another, or in terms of one behavior serving as a gateway for another[27-31]. Generally, experiences, skills, knowledge and self-efficacy can be carried-over to different behaviors and domains. While a substantial amount of research exists on transfer in educational and occupational areas, studies in the health behavior domain testing transfer and comparable concepts are comparatively few.
The first preliminary findings on COM stem from studies investigating correlations of behaviors or clusters of individuals. One such study is that by Lippke, Nigg, and Maddock[9], in which one group of participants performed some behaviors at an optimal level (e.g., physical activity) and was motivated to change the ones that were sub-optimal (e.g., nutrition). From this, one might assume that individuals were carrying-over their motivation (to perform physical activity on a regular basis) to change other behaviors as well (nutrition). Another group of study participants already maintained all behaviors optimally, so presumably had already carried-over all needed cognitions, resources and skills. Single studies are currently investigating this with longitudinal and quasi-experimental designs.
Selective evidence supporting the "gateway" assumption exists, suggesting that cognitive transfer and behavioral outcomes mainly occur with physical activity resources transferred to nutrition behaviors[28-30]. However, no study could found explicitly targeting transfer in a RCT, testing its effect in contrast to an active control group. This needs further attention in the future. The same holds true for examining the driver of different behaviors, which is hypothesized by the CCAM as higher-level goals (see below).
Emotionally relevant higher-level goals
The CCAM includes life goals or higher-level goals (e.g., "Currently, my main goal in life is..." "...changing my weight," "...being successful with my career," or "...preventing having to take medication to regulate my diabetes"). If they are emotionally relevant (e.g., "when I do something in accordance with these goals I feel content and happy"; see Figure 1, right side), they determine to what extent different behaviors are intended and performed. This originates from the Motivational Theory of Life-Span Development[14] and the Revised Adaptation Theory of Well-Being[32].
Higher-level goals can differ in terms of when or how specific the outcomes of the behaviors can expected. Long-term goals (such as health that can result from physical activity) unfold their effect only in the long run, while short-term goals (such as enjoyment, which can directly result from physical activity) contrarily have more immediate[33,34], and sometimes even adverse effects on health. Moreover, the emotional relevance of the higher-level goals determines whether individuals form an intention and change their behavior.
Only when goals are emotionally relevant and incorporated into self-identity will they be strong enough to change behaviors. One higher-level goal (e.g., to change body weight) can motivate specific behaviors (usually physical activity and nutrition). At the same time, such a goal should not conflict with other goals, which could inhibit health behaviors and support obesity or hinder diabetes prevention and management[35]. Conflicting goals could be to invest all energy into ones career, which seems to leave no time for investing time into physical activity and eating healthy. In that case, the different goals need to harmonized, which is an important element in complex behavior interventions. This can be done for instance by clarifying the role of health and long-term well-being for working efficiently and being successful with one's career.
Although most people tend to be motivated by emotionally relevant goals, which are short-term oriented[32], e.g., to strive for enjoyment or rest, the majority of health promotion programs for adults address mainly long-term goals, i.e. health related outcomes[36]. At the same time, individuals exhibit problems recognizing and engaging in long-term goals[37], which is true especially if one feels stressed, making impulsive actions more likely (such as eating unhealthily to regulate negative mood, or to not sticking to exercising goals because of acute exhaustion; see following section).
Only if individuals have a higher-level goal at a sufficiently high level can they feed into an intention to change behaviors[15]. One higher-level goal (e.g., to change body weight, or to manage diabetes without medication) can affect intentions and engagement towards different behaviors (usually physical activity and nutrition). In this sense, higher-level goals are similar to outcome expectancies, which are regarded in many theories as important for intention formation and goal pursuit[38,39]. Thus, different intentions to perform health behaviors (see Figure 1, left side) are influenced by higher-level goals, and higher-level goals are quite generic (i.e., are related to both behaviors). Higher-level goals can also change during the lifetime[14] making a developmental perspective, age and experience are important.
Stress management with health behaviors
Most people experience different stressors, which can interfere with adopting and maintaining health behaviors. If individuals have set a goal and are not reaching this goal (e.g., because of CCs, or situations such as work stress), their well-being is affected[40]. Many theories have stated this before (e.g., Demand-Control Model[41] and Effort-Reward Imbalance Model[42]), and since then the body of evidence has continued to grow. However, the CCAM explicitly incorporates stressors (tempting situations, daily hassles and chronic stressors), and how well people cope with them through health behaviors.
On the other side of this, previous evidence has demonstrated that a healthy lifestyle (i.e. regular physical activity and low-caloric food) prevents stress[1,43]. Furthermore, physical exercise in particular was found to buffer the negative effect of stress on health[44,5]. The two-ended arrows between stress management and higher-level goals (Figure 1) indicate these effects. In conclusion, the CCAM predicts the following axioms.
Conclusion
Axioms of the CCAM
Taking all assumptions of the CCAM together, the following axioms are proposed based on previous research and theories:
1. Different health behaviors (such as activity and nutrition) interrelate.
2. Emotionally relevant higher-level goals (e.g., "my main goal in life is to reduce my weight") drive different health behaviors by initiating and strengthening behavior-specific intentions (e.g., "I intend to be physically active every day for 30 minutes or more").
3. Within each behavior domain, individuals translate their intentions into behavior via planning (e.g., "I always go for a run after work"). Self-efficacy (e.g., "I am confident that I will go for a run every day, even if I have time pressure at work") is a significant moderator of planning, and additionally affects behavior directly.
4. Behavior-specific processes for behavior A (physical activity) and behavior B (nutrition) interrelate via carry-over mechanisms (e.g., "I have learned how to manage going for a run every day even if something comes up, and I can make similar plans for eating healthy products even if my friends and acquaintances eat fast food"), and via compensatory cognitions (e.g., "If I eat unhealthy now I can make up for that by exercising").
5. A healthy lifestyle consists of multiple health behaviors, which reduce the stress response and increase well-being.
Research Agenda and Outlook
The CCAM provides options for explaining and improving healthy lifestyles to prevent and manage obesity and diabetes. All assumptions of the CCAM need to be tested more systematically in the future, especially in the context of obesity and diabetes prevention and management.
The Axioms (see above) can be studied individually or the model's assumptions (Figure 1) may be tested as a whole. Different research approaches should be used and theory refinements should be applied based on the findings. Most importantly, the theoretical and evidence-based assumptions should guide interventions targeting the prevention and management of obesity and diabetes, as well as many other health challenges and diseases.
Acknowledgements
The work, which lead to this paper, was funded by a research grant from the German Ministry of Education and Research (Bundesministeriums für Bildung und Forschung, BMBF, within the framework "Engagement-Learning-Competence Development: Innovation for a Modern Working World" ["Arbeiten-Lernen-Kompetenzen entwickeln. Innovationsfähigkeit in einer modernen Arbeitswelt"], Grant No. 01HH12002).
References
- 1. Mouchacca, J., Abbott, G.R., Ball, K. Associations between psychological stress, eating, physical activity, sedentary behaviors and body weight among women: a longitudinal study. (2013) BMC Public Health 13: 828.
- 2. Wing, R., Goldstein, M., Acton, K., et al. Behavioral science research in diabetes: lifestyle changes related to obesity, eating behavior, and physical activity. (2001) Diabetes Care 24(1): 117-123.
- 3. Geliebter, A., Ochner, C.N., Dambkowski, C.L., et al. Obesity-related hormones and metabolic risk factors: a randomized trial of diet plus either strength or aerobic training versus diet alone in overweight participants. (2014) J Diabetes Obes 1(1): 1-7.
- 4. Dombrowski, S.U., Knittle, K., Avenell, A., et al. Long term maintenance of weight loss with non-surgical interventions in obese adults: systematic review and meta-analyses of randomised controlled trials. (2014) Brit Med J 348: 2646
- 5. Reiner, M., Neirmann, C., Jekauc, D., et al. Long-term health benefits of physical activity – a systematic review of longitudinal studies. (2013) BMC Public Health 13(1): 813.
- 6. Johnson, S.S., Paiva, A.L., Mauriello, L., et al. Coaction in multiple change interventions: consistency across multiple studies on weight management and obesity prevention. (2014) Health Psychol 33(5): 475-480.
- 7. Sweet, S.N., Fortier, M.S. Improving physical activity and dietary behaviors with single or multiple health behavior interventions? A synthesis of meta-analyses and reviews. (2010) Int J Environ Res Public Health 7(4): 1720-1743.
- 8. Hu, D., Taylor, T., Blow, J., et al. Multiple health behaviors: patterns and correlates of diet and exercise in a Hispanic college sample. (2011) Eat Behav12(4): 296-301.
- 9. Lippke, S., Nigg, C.R., Maddock, J.E. Health-promoting and health-risk behaviors: theory driven analyses of multiple health behavior change in three international samples. (2012) Int J Behav Med 19(1): 1-13.
- 10. Guillaumie, L., Godin. G., Vézina-Im, L.A. Psychosocial determinants of fruit and vegetable intake in adult population: a systematic review. (2010) Int J Behav Nutr Phy Act 7:12.
- 11. Rhodes, R.E., Pfaelli, L. Mediators of physical activity behavior change among adult non-clinical populations: a review update. (2010) Int J Behav Nutr Phy Act 7:37.
- 12. Morabia, A., Constanza, M.C. Multiple health behavior change interventions: tell us what you see. (2010) Prev Med 50(1-2): 1-2.
- 13. Schwarzer, R., Lippke, S., Luszczynska, A. Mechanisms of health behavior change in persons with chronic illness or disability: the Health Action Process Approach (HAPA). (2011) Rehabil Psychol 56(3): 161-170.
- 14. Heckhausen, J., Wrosch, C., Schulz, R. A motivational theory of life-span development. (2010) Psychol Rev 117(1): 32-60.
- 15. Riediger, M., Freund, A.M., Baltes, P.B. Managing life through personal goals: intergoal facilitation and intensity of goal pursuit in younger and older adulthood. (2005) J Gerontol B Psychol Sci Soc Sci 60(2): 84-91.
- 16. Gollwitzer, P. M., Sheeran, P. Implementation intentions and goal achievement. A meta-analysis of effects and processes. (2006) Adv Exp Soc Psychol 38: 69-119.
- 17. Adriaanse, M.A., Vinkers, C.D., De Ridder, D.T., et al. Do implementation intentions help to eat a healthy diet? A systematic review and meta-analysis of the empirical evidence. (2011) Appetite 56(1): 183-193.
- 18. Ashford, S., Edmunds, J., French, D.P. What is the best way to change self-efficacy to promote lifestyle and recreational physical activity? A systematic review with meta-analysis. (2010) Brit J Health Psych 15(2): 265-288.
- 19. Bandura, A. Health promotion by social cognitive means. (2004) Health Educ Behav 31(2): 143-64.
- 20. Knäuper, B., Rabiau, M., Cohen, O., et al. Compensatory health beliefs: theory and measurement. (2004) Psychol Health 19(5): 607-624.
- 21. Peolman, M.P., Vermeer, W.M., Vyth, E.L., et al. 'I don't have to go to the gym because I ate very healthy today': the development of a scale to assess diet-related compensatory health beliefs. (2013) Public Health Nutr 16(2): 267-273.
- 22. Radtke, T., Scholz, U., Keller, R., et al. Smoking is ok as long as I eat healthily: compensatory health beliefs and their role for intentions and smoking within the health action process approach. (2012) Psychol Health 27(2): 91-107.
- 23. Kronick, I., Knäuper, B. Temptations elicit compensatory intentions. (2010) Appetite 54(2): 398-401.
- 24. Barnett, S. M., Ceci, S. J. When and where do we apply what we learn? A taxonomy for far transfer. (2002) Psychol Bull 128: 612-637.
- 25. Hofstetter, H., Dusseldorp, E., van Empelen, P., et al. A primer on the use of cluster anlaysis or factor analysis to assess co-occurrence of risk behaviors. (2014) Prev Med 67: 141-146.
- 26. Mata, J., Silva, M.N., Vieira, P.N., et al. Motivational "spill-over" during weight control: increased self-determination and exercise intrinsic motivation predict eating self-regulation. (2009) Health Psychol 28(6): 709-716.
- 27. Dutton, G.R., Napolitano, M.A., Whiteley, J.A., et al. Is physical activity a gateway behaviour for diet? Findings from a physical trial. (2008) Prev Med 46(3): 216-221.
- 28. Fleig, L., Kerschreiter, R., Schwarzer, R., et al. 'Sticking to a healthy diet is easier for me when I exercise regularly': cognitive transfer between physical exercise and health nutrition. (2014) Psychol Health 29(12): 1361-1372.
- 29. Fleig, L., Küper, C., Schwarzer, R., et al. Cross-behavior associations and multiple behaviour change: a longitudinal study on physical activity and fruit and vegetable intake. (in press) J Health Psychol.
- 30. Fleig, L., Lippke, S., Pomp, S., et al. Intervention effects of exercise self-regulation on physical exercise and eating fruits and vegetables: a longitudinal study in orthopaedic and cardiac rehabilitation. (2011) Prev Med 53(3): 182-187.
- 31. Tucker, M., Reicks, M. Exercise as a gateway behavior for healthful eating among older adults: an exploratory study. (2002) J Nutr Educ Behav 34 (1): S14-S19.
- 32. Diener, E., Lucas, R.E., Scollon, C.N. Beyond the hedonic treadmill: revising the adaptation theory of well-being. (2006) Am Psychol 61(4): 305-314.
- 33. Latham, G.P., Locke, E. New developments in and directions for goal-setting research. (2007) Eur Psychol 12(4): 290-300.
- 34. Moore, S.N., Tapper, K., Murphy, S. Feeding goals soght by mothers of 3-5-year-old children. (2010) Br J Health Psychol 15(1): 185-196.
- 35. Presseau, J., Tait R.I., Johnston, D.W., et al. Goal conflict and goal facilitation as predictors of daily accelerometer-assessed physical activity. (2013) Health Psychol 32(12): 1179-1187.
- 36. Stuntz, C., Weiss, M. Motivating children and adolescents to sustain a physically active lifestyle. (2010) American Journal of Lifestyle Medicine 4(5): 433-444.
- 37. Noar, S.M., Benac, C.N., Harris, M.S. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. (2007) Psychol Bull 133(4): 673-693.
- 38. Lippke, S., Ziegelmann, J.P. Theory-based health behavior change: developing, testing and applying theories for evidence-based interventions. (2008) Applied Psychology 57(4): 698-716.
- 39. Williams, D.M., Anderson, E.S., Winett, R.A. A review of the outcome expectancy construct in physical activity research. (2005) Ann Behav Med 29(1): 70-79.
- 40. Koestner, R., Lekes, N., Powers, T.A., et al. Attaining personal goals: self-concordance plus implementation intentions equals success. (2002) J Pers Soc Psychol 83(1): 231-244.
- 41. Karasek, R., Theorell, T. Healthy work: stress, productivity, and the reconstruction of working life. (1990) New York, NY: Basic Books. 89-103.
- 42. Seigrist, J. Adverse health effects of high-effort/low reward conditions. (1996) J Occup Health Psychol 1(1): 27-41.
- 43. Zschucke, E., Renneberg, B., Dimeo, F., et al. The stress-buffering effect of acute exercise: evidence for HPA axis negative feedback. (in press) Psychoneuroendocrino.
- 44. Gerber, M., Pühse, U. Review article: do exercise and fitness protect against stress-induced health complaint? A review of the literature. (2009) Scand J Public Health 37(8): 801-819.