Pelvic Abscess with Uterine Wound Dehiscence Post Cesarean Section, Rare Presentation with Modified Management: Case Report & Literature Review
Hamadeh Sameer1*, Addas Bishr1, Hamadeh Nasreen1, Alghanmi Ibraheem2, Rahman Jessica1, Rahman M.S1
Affiliation
- 1Department of Obstetrics & Gynaecology, King Fahd Teaching Hospital, Alkhobar, KSA
- 2Department of Radiology, King Fahd Teaching Hospital, Alkhobar, KSA
Corresponding Author
Sameer Hamadeh, Department of Obstetrics & Gynaecology, King Fahd Teaching Hospital, Alkhobar, KSA, E-mail: sameer_hamadeh@hotmail.com
Citation
Sameer, H., et al. Pelvic Abscess With Uterine Wound Dehiscence Post Caesarean Section, Rare Presentations With Modified Management: Case Report & Literature Review. (2016) J Gynecol Neonatal Biol 2(1): 9-12.
Copy rights
© 2016 Sameer, H. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Postpartum fever; Caesarean section; Postpartum pelvic abscess; Uterine dehiscence; Percutaneous transabdominal aspiration
Abstract
The rate of caesarean section rate is increasing worldwide, the ideal rate being from 10 to 15% according to WHO. Various complications are associated with this operative procedure, such as intraoperative hemorrhage, wound and chest infections, abdominal wound dehiscence, from anesthesia, deep vein thrombosis, and pulmonary embolism to name a few. Uterine wound dehiscence is a very rare complication of cesarean section that presents with PPH[1]. Postoperative pyrexia may result from various causes, pelvic abscess being a very rare one, occurring in < 1% of patients with post cesarean endometritis[2]. This report describes anunusual cause of fever following cesarean delivery and presentation of its sequelae, our method of management, its outcome with comparison to similar cases presented in the literature. This the first case report in literature of post-operative pelvic abscess with uterine wound dehiscence, a rare presentationthat was managed with radiological intervention and assistance.
Introduction
Postpartum pelvic abscess is a very rare complication occurring in < 1% of patients with postpartum endometritis[2]. Suspected clinically after a history of persistent fever unresponsive to antibiotics therapy. It isan unexpected cause of postpartum pyrexia without clinical evidence of postpartum endometritis. Uterine dehiscence is another rare complication post-caesarean section, frequency ranges between 0.06 and 3.8%[3,4]. It presenteither as postpartum haemorrhage, localized or generalized peritonitis, andif it is associated with endomyometrtitis and abscess, hysterectomy is recommended[1,5]. We present a patient with postpartum pelvic abscess complicated by uterine wound dehiscence post caesarean section. This patient complained of postpartum fever, developed pelvic abscess over a very short time,with no clinical signs suggestive of endometritis. The clinical impression was established after development of uterine scar dehiscence presenting with copious vaginal discharge of pus. She was managed effectively by radiological interventionas the first line of therapy with dramatic and immediate improvement symptomatically and clinically without waiting the effect of antibiotics response, thus avoiding the need of other surgical interventions and prolonged hospital stay. She was discharged from the hospital with good outcome.
Case Presentation
A 38 year old, P7 + 0, Not known to have any medical disease, had an emergency caesarean section in other hospital due to cord prolapse with unremarkable post-operative period, apart from mild lower abdominal pain, treated with analgesics. She was discharged from hospital on day six post operationbut presented again to the same hospital emergency room after two days complaining of moderate suprapubic pain, distension and dysuria. Physical examination was unremarkable. Total white blood cells count was normal. She was initially diagnosed to have cystitis. A MSU sample for culture and sensitivity collected followed by administration of antibiotics. Few hours later she developed a high pyrexia of 38.5°C, associated with sweating, chills and rigors relived partially by analgesia. There was no history of nausea, vomiting, constipation or other symptoms. She sought medical advice in primary heath care centre, was continued on the same antibiotics with an impression of UTI. One day later, she complained of copious, pussy, vaginal discharge with mild improvement of her symptoms, apart from the fever. She presented to our emergency room 11 days postoperation. She does not look distressed. Her vital signs revealed a temperature of 38.1°C with resting tachycardia, stable blood pressure and respiratory rate. Pertinent physical exam findings included normal breast andlower limbs. The abdomen was soft, lax with no sign of peritonitis, mild suprapubic distension and tenderness, sub-involuted uterus at the level of umbilicus, will healed caesarean section skin incision with no signs of infection. Speculum examination showed a normal vagina and cervix apart from little amount of foul smelling, pussy fluid coming through the cervix. Vaginal and cervical swab were taken for culture and sensitivity. Bimanual examination revealed no adnexal mass or tenderness, no cervical excitation. Larger amounts of pussy fluid exuded from the vagina. Abdominal and pelvic ultrasound were carried outand revealeda normal size uterus with clear endometrial lining and slight fluid in the uterine cavity. There was a collection anterior to the uterus,measuring 8.3 x 7.8 cm, thought to be sub-rectal collection [Figure 1]. Her investigations showed normal Hb, platelet and WBC count with elevated ESR and CRP. Bacterial vaginitis was reported on the HVS. An abdominal and pelvic CT scan was done to confirm a large contained subserosal uterine abscess collection anterior to the uterus, superior to the bladder, measuring 12.8 x 8.1 x 9.7 cm (in caraniocaudal, anteroposterior & transverse diameter). The endometrial cavity was fluid filled with multiple air pockets, finding could be attributed to a large abscess with Endometritis and worrisome wound dehiscence. No fluid collection was noted in the peritoneal cavity (Figure 2). The patient was admitted and IV Tazocin was commenced with a plan to perform immediate percutaneous aspiration under ultrasound guide. Aspiration was done by inserting 85 F pigtail drainage catheter under ultrasound guide, and approximately 350 ml dark brownish fluid was obtained. No acute complication was encountered during the procedure. Culture and sensitivity of the fluid showed E.coli. The fever subsided immediately post drainage and the patient was symptomless. She was hospitalised for a week to complete the course of IV antibiotics. Repeat pelvic ultrasound and CT before discharge of the patient showed interval reduction of previously noted anterior uterine intraperitoneal fluid collection with surrounding inflammatory reaction. The remaining fluid measured approximately 1.7 x 1.3 x 4.6 cm with 2.3 x 2.7 x 6.23 cm (in transverse, anteroposterior & caraniocaudal diameter respectively). No newly detected collection, free fluid or air was noted (Figure 3). She was discharged in satisfactory condition. And followed in the OPD one week later. As the patient had no complaints, no further follow was given.
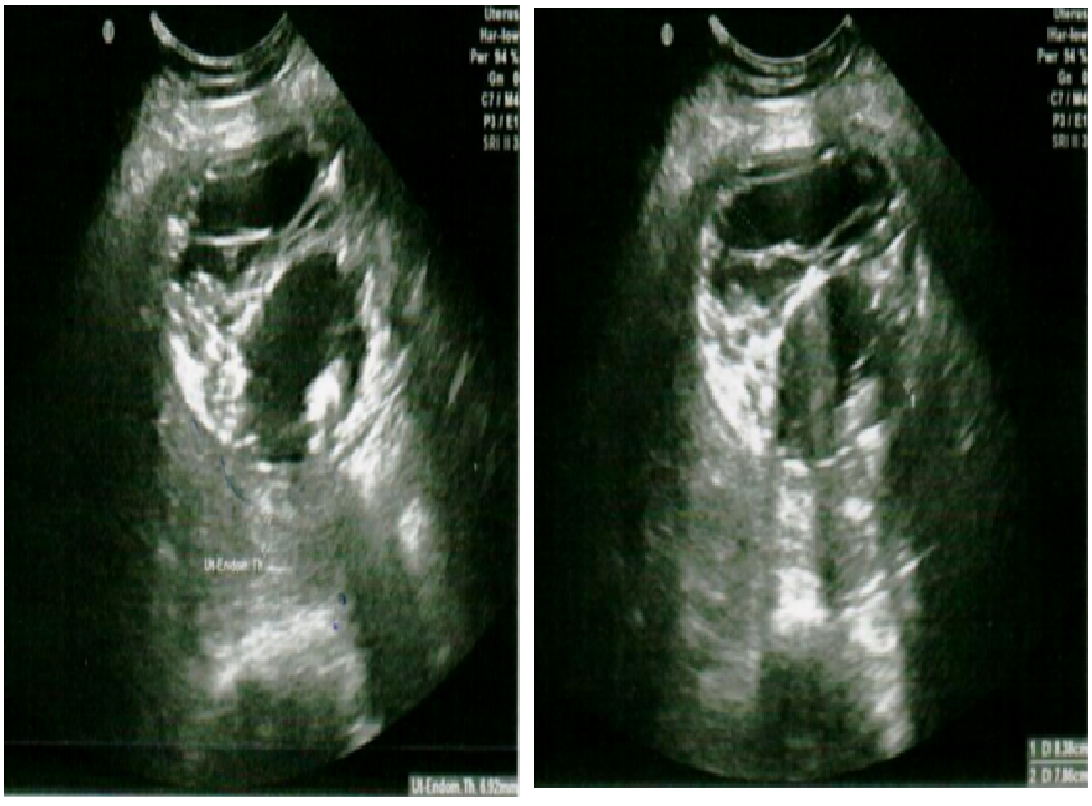
Figure 1: Gray scale appearance, showing the presence of collection anterior to the uterus confined measuring 8.3 x 7.8 cm thought to be sub-rectal collection
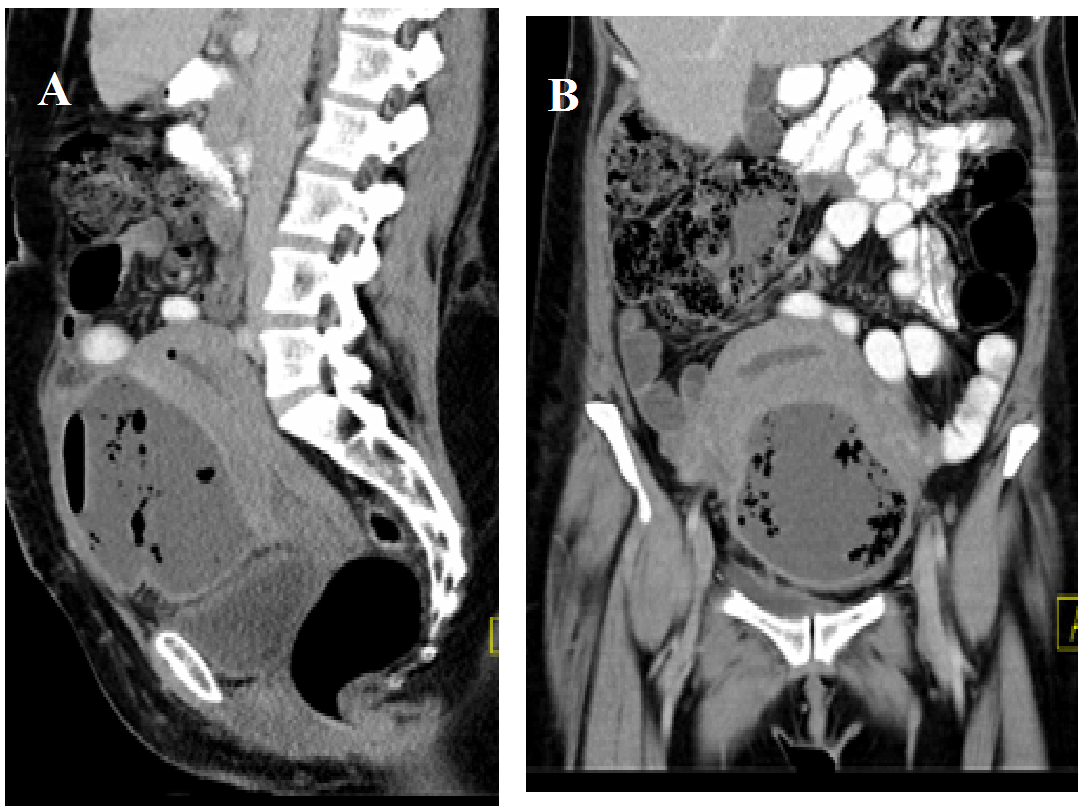
Figure 2: Post contrast enhancement CT scan Coronoal (A) & sagittal (B) showed large contained sub-Serosal uterine abscess collection with multiple air pocket, no pelvic collection
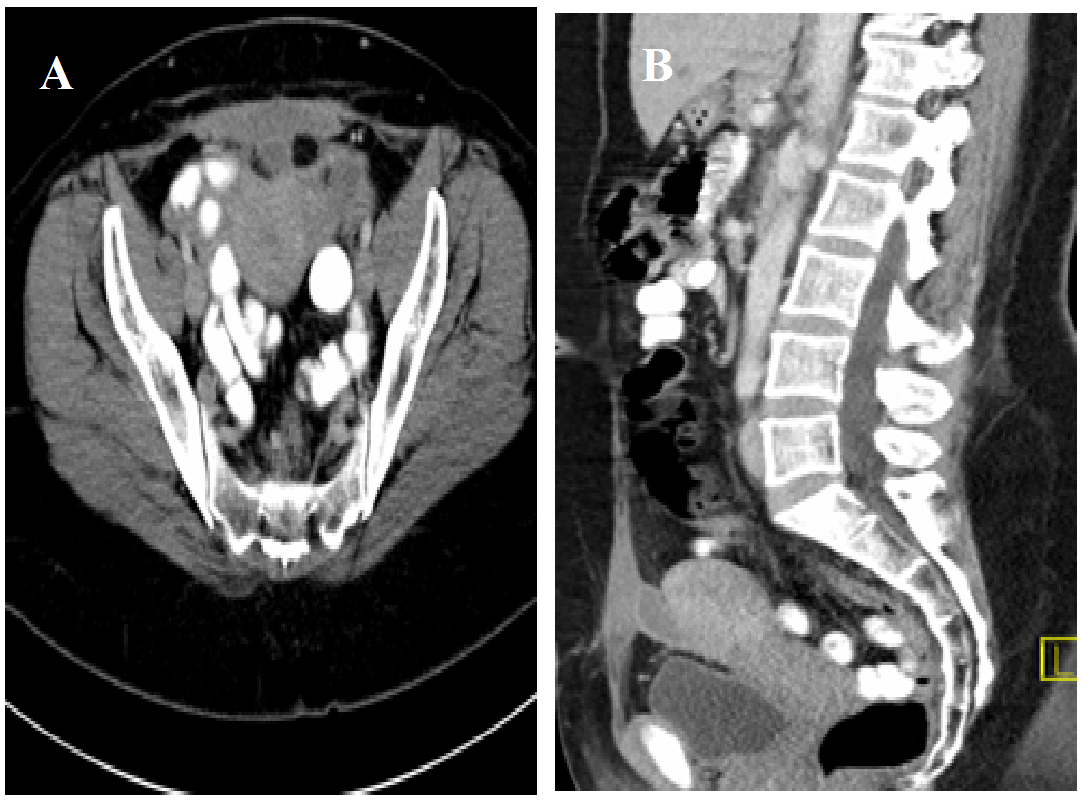
Figure 3: Post percutaneous collection, enhanced CT scan axial (A) & sagittal (B) showed almost complete subserosal uterine collection drained
Discussion
Pelvic abscess is a rare cause of postpartum fever; its incidence being less than 1% of patients undergoing obstetrics and gynecology procedures[1]. It usually results from under treatment or delayed treatment with endometritis post cesarean section. These patients usually have persistent pyrexia, despite treatment. The location of abscess can be either in posterior cul-de-sac, anterior lay, between the uterine wall and urinary bladder or in the broad ligament. The causative agents are anaerobic bacteria and aerobic Gram negative bacilli. These patients usually look ill, tachycardic, and tachypneic with lower abdominal pain and possible signs of peritonitis depending on the spread of abscess. On pelvic examination, there may be uterine or adnexal tenderness, or a fluctuant mass palpable, depending on the location of the abscess. The patient usually has an elevated white blood cell count with a shift to the right. Pelvic ultrasound is required to confirm the diagnosis. CT scan is performed when there is doubt about the diagnosis or location of the abscess[4]. The patients should be treated with broad-spectrum parenteral antibiotics[6,7]. Aspiration of abscess under ultrasound guide depends on its site[8]. Drainage may be accomplished by insertion of a catheter under ultrasound or CT guidance for abscesses located anterior or lateral to the uterus, or via a small colostomy for patients with an abscess in the posterior cul-de-sac. This method of treatment was reported mainly in cases of pelvic abscess post gynecological procedures[9,10], never in patients after cesarean section with uterine scar dehiscence. Laparotomy may be necessary to ensure complete drainage. If uterine scar dehiscence is associated with signs of fulminating infection direct laparotomy is recommended[5]. The patient looked well with a non-septic appearance at her presentation with mild suprapubic pain,urinary symptoms and later fever, rigors, but no signs of abdomino-pelvic tenderness. CBC showed no leukocytosis, ESR and CRP were elevated. There were no signs of peritonitis because the abscess was concealed by the visceral peritoneum between the anterior uterine wall and urinary bladder accommodating more than 350 ml of puss without resultant rupture. Compression of the urinary bladder causing difficult urination was thought initially to be due to cystitis or UTI when she developed pyrexia and was managed accordingly. The classical symptoms and signs of endometritis were masked and thus its possibility and sequela were over looked. When she developed uterine dehiscence,it became very suspicious, especially with the passage of copious pussy vaginal discharge. The symptoms began to improve after the abscess was drained. Asdiagnosis by ultrasound was not conclusive, CT followed to confirm it, further localizing the size and site of the abscess. The patient was started on parenteral antibiotics and it was decided to immediately to undertake percutaneous transabdominal drainage under ultrasound guidance as first line therapy without waiting 2 - 3 days for antibiotics cover, considering the imminent risk of rupture or leak of this large abscess (Figure 1,2). Drainage of the abscess resulted in dramatic and remarkable clinical improvement of the patient. Further surgical interventions was not necessary, and the patient was discharged in satisfactory condition, after completion of the course of IV antibiotic for which there was no oral substitute. At the OPD follow up visit, two weeks later, the patient was well and symptom free.
Conclusion and Recommendations
Pelvic abscess post-cesarean section can occur without clinical signs suggestive of endometritis and should remain one of the differential diagnosis of any patient with pyrexia after cesarean section. Percutaneous trans abdominal drainage under ultrasound guide can be tried as a first line therapy in patients with pelvic abscess post cesarean section with large, localized abscess, even if associated with uterine scar dehiscence and endometritis in clinically stable patient. This would prevent its spontaneous rupture and avoiding the need for direct laparotomy as the sole treatment for such conditions. Transabdominal drainage of the drainage resulted in immediate improvement of the clinical condition of the patient.
Acknowledgement:
To the patients who allowed us to report the cases & provide us with signed permission for its publications.
Conflict of Interest:
No conflicts of interest
References
- 1. Dhar, R.S., Misra, R. Postprtum Uterine Wound Dehsince Leading to Secondary PPH: Unusal sequelae. (2012) Case Rep Obstet Gynecol.
- 2. Alwani, M., Mishra, S., Thakur, R. Generalized peritonitis with uterine incision necrosis with dehiscence following cesarean section presenting as genitourinary fistula: a unique complication. (2014) J Med 3(3): 762-766.
- 3. Jurkovic, D., Hillaby, K., Wolfer, B., et al. First-trimester diagnosis and mangment of pregnancies implanted into the lower uterine segment Cesarean section scar. (2003) Ultrasound Obstet Gynecol 21(3): 220-227.
- 4. Royo P., Garacia M.M., Olratectoechea, B., et al. Two-dimensional power doppler-three-dimensional ultrasound imaging of cesarean section dehiscence with utero-peritoneal fistula: a case report. J Med Case Reports 3: 42.
- 5. Rivlin, M.E., Carroll, C.S., Morrison, J.C. Infection necrosis with dehiscence of uterine repair complicating cesarean delivery: a review. (2004) Obstet Gynecol Surv 59(12): 833-837.
- 6. Wagner, M.S., Bedard, M.J. Postpartum uterine wound dehiscence: a case report. (2006) JOGC 28(8): 713-715.
- 7. Usta, M.I., Hamdi, M.A., Musa, A.A., et al. Pregnancy outcome in patients with previous uterine rupture. (2007) Act Obstetrics et Gynecologica Scandinavica 86(2): 172-176.
- 8. Kathrene, T., Wayne, T., Thomas, J.O.N., et al. Ultrasound assessment of postpartum fever-lifelong learning. (2013) J Ultrasound Obstet Gynecol 7(2): 219-230.
- 9. Ahmed S.E.A. Postpartum uterine caesarean incision necrosis & Pelvic abscess managed by hysterectomy: A complication of puerperal endomyometrtitis. Res J Med Sci 8(2): 53-55.
- 10. Ida, A., Kubota, Y., Nosaka, M., et al. Successful management of a cesarean scar defect with dehiscence of uterine incision by using wound lavage: Case report. (2014) Obstet Gynecol.