Prevalence and Clinical Impact of Sinusitis in Liver Graft Recipients
Ibrahim Yel1, Clara Groh1, Kamilla Sztwiertnia1, Andreas A Schnitzbauer2, Wolf O Bechstein2, Timo Stöver3, Katrin Eichler1, Nina Weiler4, Stefan Zeuzem4, Thomas J Vogl1, Boris Bodelle1,#, Martin-Walter Welker4*#
Affiliation
1Institute of Diagnostic and Interventional Radiology, University Hospital Frankfurt, Theodor-Stern-Kai 7, 60590 Frankfurt, Germany
2Department of General and Visceral Surgery, University Hospital Frankfurt, Theodor-Stern-Kai 7, 60590 Frankfurt, Germany
3Department of Otolaryngology, University Hospital Frankfurt, Theodor-Stern-Kai 7, 60590 Frankfurt, Germany
4Medical Clinic 1, University Hospital Frankfurt, Theodor-Stern-Kai 7, 60590 Frankfurt, Germany
# Both authors contributed equally to this work
Corresponding Author
Martin-Walter Welker, University Hospital Frankfurt, Medical Clinic 1, Theodor-Stern-Kai 7, 60590 Frankfurt am Main, Germany, E-mail: martin-walter.welker@kgu.de
Citation
Yel I et al. Prevalence and Clinical Impact of Sinusitis in Liver Graft Recipients. (2019) J Gastrointest Disord Liver Func 5(1): 21-27.
Copy rights
© 2019 Welker, MW. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Sinusitis; Liver transplantation; Surgery; Computer tomography
Abstract
Objectives: The evaluation program in liver transplant candidates is often based on centre protocols due to a lack of sufficient data defining the necessity of distinct investigations. Prevalence of rhinosinusitis (RS) and respective impact on mortality in liver transplantation (LT) candidates and subsequent LT in European countries has not been conclusively determined. Aim of this study was to clarify whether screening for RS by computed tomography of paranasal sinus (CTpns) is mandatory in unselected LT candidates.
Material and Methods: Patients evaluated for LT between 01/July/2011 and 31/December/2016 at a tertiary German LT center who received a standardized CT pns were included. Prevelance and severity of RS were graduated. Frequency, outcome of sinus surgery, as well as mortality and frequency of infectious complications in patients with and without RS was assessed prior and up to one year after LT.
Results: RS was present in 43/234 (18%) patients. In the majority, RS was mild (n=36) or moderate (n=6). Sinus surgery was done in 8/43 (19%) LT candidates showing RS Serious complications associated with RS surgery were not observed. LT was performed in 59/234 patients including 12 patients with RS. Overall survival and infectious complications did not differ between patients with or without RS.
Conclusions: Coincidental RS is frequently observed in LT candidates, but mainly mild or moderate. Therefore, routine CTpns may not be recommended in unselected LT candidates.
Introduction
Liver transplantation (LT) is an established treatment option in selected patients with advanced liver disease including decompensated liver cirrhosis (LCI) and early hepatocellular carcinoma (HCC)[1-3]. A major part of the evaluation process of patients for LT is to identify contraindications which may prevent a successful course after LT. Recently, infections have been identified as a trigger of acute or chronic liver failure in patients even with compensated LCI, a complication burdened with significant mortality[4,5]. The main complications beside early rejection episodes within the first year after initially successful LT are considered surgical and infectious due to the intense immunosuppression in this time period[2,6]. Thus, unresolved infections may be considered a contraindication for liver transplantation and thorough screening for localized and systemic infections is recommended before LT[7-10].
Acute and chronic rhinosinusitis (RS) is a common health problem in the general population and may be overt, oligo- or asymptomatic[11]. Although it seems reasonable that even asymptomatic RS may cause major infectious complications in LT candidates, prevalence and clinical impact of RS for the outcome after LT have not been determined concluding, so far[12,13]. Thus, it is unknown; whether evaluation protocols in LT candidates should include screening for RS by paranasal sinus computed tomography (CT pns) independent from clinical symptoms.
In general, screening for RS before LT may be considered reasonable, if the overall prevalence in the target population is relevant, the clinical course is meaningfully altered by coincidental RS and furthermore patients identified can be safely treated, e.g. by nasopharyngeal surgery. Of note, patients with liver cirrhosis undergoing elective and emergency surgery including abdominal and orthopedic procedures are on risk of acute or chronic liver failure burdened by significant mortality[14,15].
The aim of the current study was to clarify whether screening for RS by CT pns should be considered mandatory in the evaluation process for LT. In our center, the evaluation protocol in liver transplant candidates includes a CT pns in patients with and without clinical evident RS. Therefore, the overall prevalence of acute and chronic RS in liver transplant candidates identified by CT pns should be assessed. Furthermore, the clinical impact of resolved and unresolved RS on the clinical course for patients before and after LT was to be determined.
Materials and Methods
Study design
All consecutive patients evaluated for LT between 01/July/2011 and 31/December/2016 who received CT pns were included in this study. Thus, patients were prospectively screened for RS, but data collection and analysis was done retrospective. Study approval was obtained by the local Ethics Committees for Medical Research in accordance with the 1975 Declaration of Helsinki. Biochemical and clinical data were collected from medical records at the evaluation for LT, the time point of LT itself and up to 12 months after transplantation.
Assessment of sinusitis and grading of sinusitis
Sinusitis screening was performed on a 2x192-detector row, third-generation dual-source computed tomography (CT) system (Somatom Force, Siemens Healthcare, Forchheim, Germany). The scan protocol consisted of a high-pitch (pitch, 2.2) examination of the paranasal sinuses by using a tube voltage of 100-kV and a tube current of 50 mAs. A detailed listing of the CT parameters for the examination protocol is given in Table 1. Radiologic investigation of patients was done in supine position, slightly reclining the head to obtain a parallel alignment of the upper jaw to the gantry, thus minimizing dental artefacts. The imaging ranged from the roof of the frontal sinus up to the maxilla in the craniocaudal direction. By default, 1-mm axial, 1-mm coronal, as well as 1-mm sagittal images (each with a bony and soft-tissue kernel) were reconstructed from the raw data set.
Table 1: CT acquisition parameters
|
CT unit |
Third-generation DSCT |
|
Examination mode |
SECT |
|
Tube voltage |
100-kV |
|
Tube current |
50 mAs |
|
Pitch |
2.2 |
|
Table movement speed |
507 mm/s |
|
Rotation time |
0.25 s |
|
Collimation |
192x0.6 mm |
|
Slice thickness |
1 mm |
|
Increment |
1 mm |
CT, computed tomography; DSCT, dual-source CT; SECT, single-energy CT.
All images were reviewed by two radiologists (three and ten years of experience in evaluating CT of paranasal sinuses). Definition of RS included presence of peripheral mucosal thickening, air-fluid level, gas bubbles within the fluid and obstruction of the ostiomeatal complex (acute sinusitis) as well as sclerotic thickened bone involving the sinus wall in the presence of opacification and/orintrasinus calcification (chronic sinusitis). In patients with RS, disease severity was semi quantitatively assessed by the Lund-Mackay-score[16,17]. A score of 1-6 defined mild disease, 7-12 score points indicated moderate and 13-24 pointed severe RS[16,17].
Moreover, all patients were seen by a nasopharyngeal specialist. Treatment decisions including nasopharyngeal surgery were made in an interdisciplinary approach including hepatologists, radiologists, nasopharyngeal specialists and transplant surgeons and based on clinical and imaging results.
Radiation dose estimation
For the estimation of radiation doses, the dose–length product (DLP, given in mGy*cm) and volume-weighted CT dose index (CTDIVOL, given in mGy) were calculated from individual patient protocols. These data were automatically generated at the end of an examination and stored in the picture archiving and communication system. According to Deak et al. an appropriate conversion factor (k) of 0.0019 mSv/mGy*cm was used to estimate the effective dose (effective dose=DLP x k)[18].
Immunosuppression in patients undergoing liver transplantation
The standard immunosuppression protocol contained an induction treatment with basiliximab and methylprednisolone during transplantation. Maintenance immunesuppression was in general based on tacrolimus (target through level 5-8 ng/ml) in combination with mycophenolate mofetil, prednisolone or everolimus. In the latter, target tacrolimus and everolimus through levels ranged from 3-5 ng/ml and 3-8 ng/ml, respectively.
Statistical analyses
Clinical and biochemical characteristics of patients were expressed as mean ± standard deviation (SD). Gaussian distribution of all data was checked by the Kolmogorov-Smirnov-Lilliefors test. Between two variables unpaired t-test (normally distributed data) and Mann-Withney-U test (non-normal distributed data) was performed. The log-rank-test was used to determine the correlation between the presence of an acute or chronic sinusitis and survival. Competing-risk-analysis was applied to test a potential correlation of acute or chronic sinusitis and occurrence of infectious complications after LT. Unless indicated otherwise, all tests were two-tailed and p values < 0.05 were considered significant.
Statistical analysis was performed by using GraphPad Prism Version 7.0 (GraphPad Software; La Jolla, CA, USA), IBM SPSS Statistics Version 21 (IBM SPSS statistics; Armonk, NY, USA), and R Version 3.5.0 (R Core Team 2018. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/).
Results
Patients’ characteristics
Overall, 234 patients were included in the study. During the study period, 59/234 patients received a liver graft. Detailed clinical and biochemical data of patients at the time point of evaluation and LT are given in Table 2 and 3.
Table 2: Patients` characteristics at evaluation for liver transplantation
|
Parameter |
Patients (n=234) |
|
Demography |
|
|
Age [years; mean ± SD (range)] |
54.3 ± 9.6 (21–71) |
|
Gender distribution: male/female (n/n) |
163/71 |
|
BMI [kg/m²; mean ± SD (range)] |
26.5 ± 2.6 (21.4–33.6) |
|
General and transplant specific medical data |
|
|
Etiology of liver disease prior LT |
|
|
Autoimmune [n (%)] |
22 (9.4%) |
|
HCV [n (%)] |
72 (30.8%) |
|
HBV + HCV [n (%)] |
5 (2.1%) |
|
HBV +/- HDV [n (%)] |
24 (10.3%) |
|
Alcohol [n (%)] |
68 (29.1%) |
|
Cryptogenic [n (%)] |
17 (7.3%) |
|
NAFLD [n (%)] |
9 (3.8%) |
|
Others (e.g. haemochromatosis, PSC) [n (%)]a |
17 (7.3%) |
|
MELDscore [mean ± SD (min, max)] |
15.8 ± 6.4 (6–36) |
|
HCC [n (%)] |
70 (29.9%) |
|
HIV coinfection [n (%)] |
3 (1.3%) |
|
Biochemistry |
|
|
Albumin [g/dl; mean ± SD (min, max)] |
3.3 ± 0.6 (1.6–4.9) |
|
Bilirubin [mg/dl; mean ± SD (min, max)] |
4.8 ± 6.1 (0.2–41) |
|
Creatinine [mg/dl; mean ± SD (min, max)] |
1.1 ± 0.8 (0.3–6.5) |
|
INR [mean ± SD (min, max)] |
1.4 ± 0.4 (0.9–3.1) |
|
CRP [mg/dl; mean ± SD (min, max)] |
1.4 ± 2.4 (0.1–26.0) |
BMI, body mass index; HBV, Hepatitis B virus; HCV, Hepatitis C virus; HDV, Hepatitis D virus; NAFLD, nonalcoholic fatty liver disease; PSC, primary sclerosing cholangitis
Table 3: Patients` characteristics at liver transplantation.
|
Parameter |
Patients (n=59) |
|
Demography |
|
|
Age [years; mean ± SD (range)] |
56.8 ± 8.8 (24–69) |
|
Gender distribution: male/female (n/n) |
48/11 |
|
BMI [kg/m²; mean ± SD (range)] |
27.2 ± 3.6 (22.7–33.8) |
|
General and transplant specific medical data |
|
|
Etiology of liver disease prior LT |
|
|
Autoimmune [n (%)] |
5 (8.5%) |
|
HCV [n (%)] |
19 (32.2%) |
|
HBV + HCV [n (%)] |
4 (6.7%) |
|
HBV +/- HDV [n (%)] |
6 (10.2%) |
|
Alcohol [n (%)] |
15 (25.4%) |
|
Cryptogenic [n (%)] |
3 (5.1%) |
|
NAFLD [n (%)] |
3 (5.1%) |
|
Others (e.g. haemochromatosis, PSC) [n (%)]a |
4 (6.8%) |
|
MELDscore [mean ± SD (min, max)] |
20.4 ± 10.1 (6–40) |
|
HCC [n (%)] |
31 (52.5%) |
|
HIV coinfection [n (%)] |
1 (1.7%) |
|
Biochemistry |
|
|
Albumin [g/dl; mean ± SD (min, max)] |
3.3 ± 0.8 (1.1–4.9) |
|
Bilirubin [mg/dl; mean ± SD (min, max)] |
6.8 ± 9.2 (0.4–37.5) |
|
Creatinine [mg/dl; mean ± SD (min, max)] |
1.5 ± 1.2 (0.5–6.5) |
|
INR [mean ± SD (min, max)] |
1.7 ± 0.6 (1.0–3.6) |
|
CRP [mg/dl; mean ± SD (min, max)] |
1.4 ± 2.0 (0.1–11.8) |
BMI, body mass index; HBV, Hepatitis B virus; HCV, Hepatitis C virus; HDV, Hepatitis D virus; NAFLD, Non-alcoholic fatty liver disease; PSC, primary sclerosing cholangitis
Prevalence and severity of acute and chronic sinusitis and comparison of patients with and without sinusitis
The overall prevalence of RS in LT candidates was 43/234 (18%). In detail, acute and chronic RS was present in 22/234 (9%) and 21/234 (9%) patients, respectively. In the majority, sinusitis was classified as mild (n=36) or moderate (n=6) (Table 4, Figure 1 and 2). Patients with or without sinusitis did not differ with respect to age, gender or MELD score (p=n.s.), and overall mortality was independent of the presence of sinusitis, also (p=n.s.; Table 5). Nasopharyngeal surgery was performed in 8/43 (19%) LT candidates. Major complications including fatal courses associated with nasopharyngeal surgery were not observed. In the cohort of 59 patients, who received a liver graft during the study period, RS was present at evaluation in 12/59 (20%) patients. Only two out of these 12 patients had received nasopharyngeal surgery prior LT. No respective surgery was performed in the remaining 10 patients within the study period (up to one year after LT). Overall survival as well as infectious complicationsup to one year after LT were independent tothe presence of acute or chronic RS at evaluation or after LTX (p=n.s.) (Figure 3).

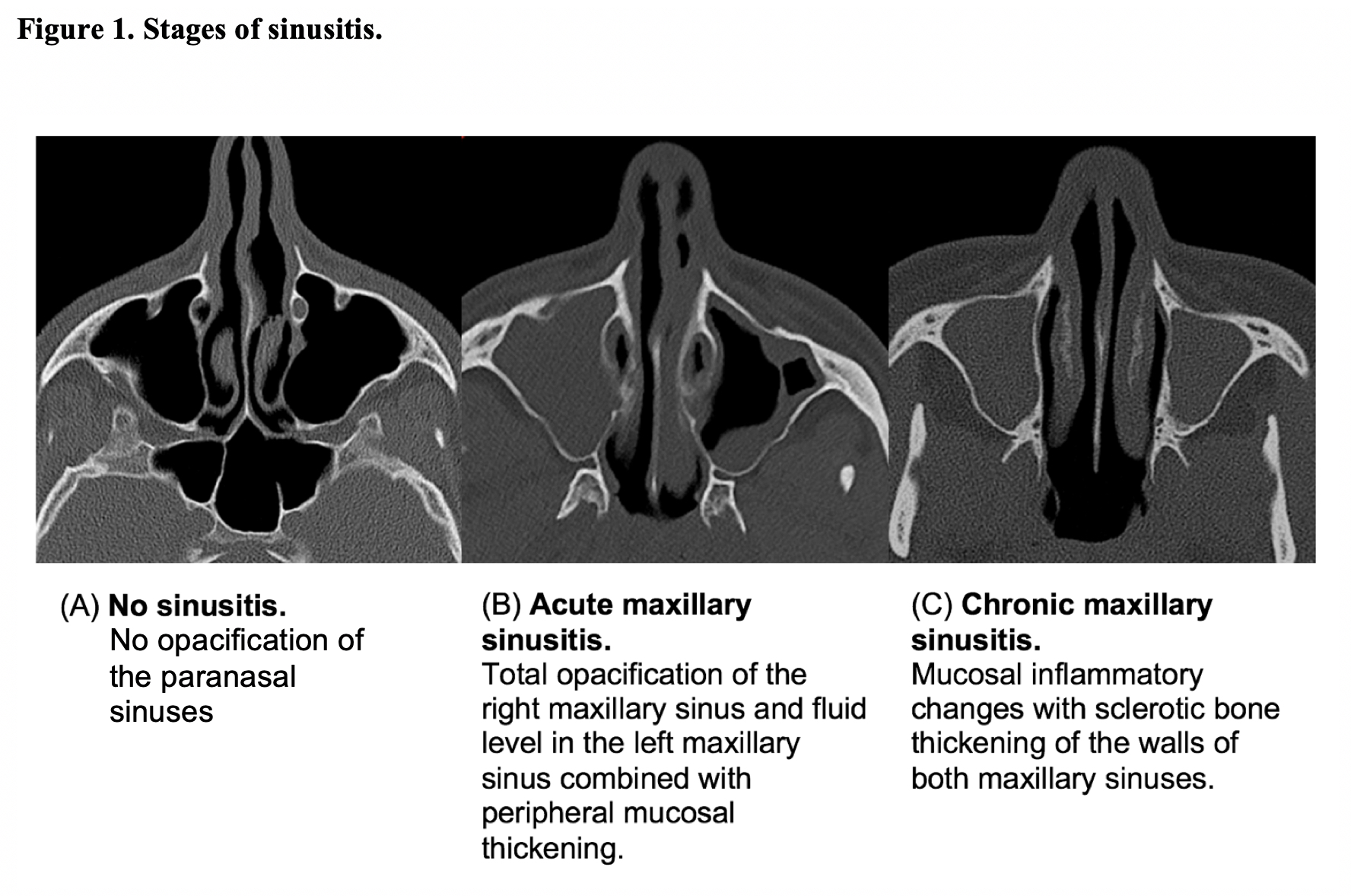

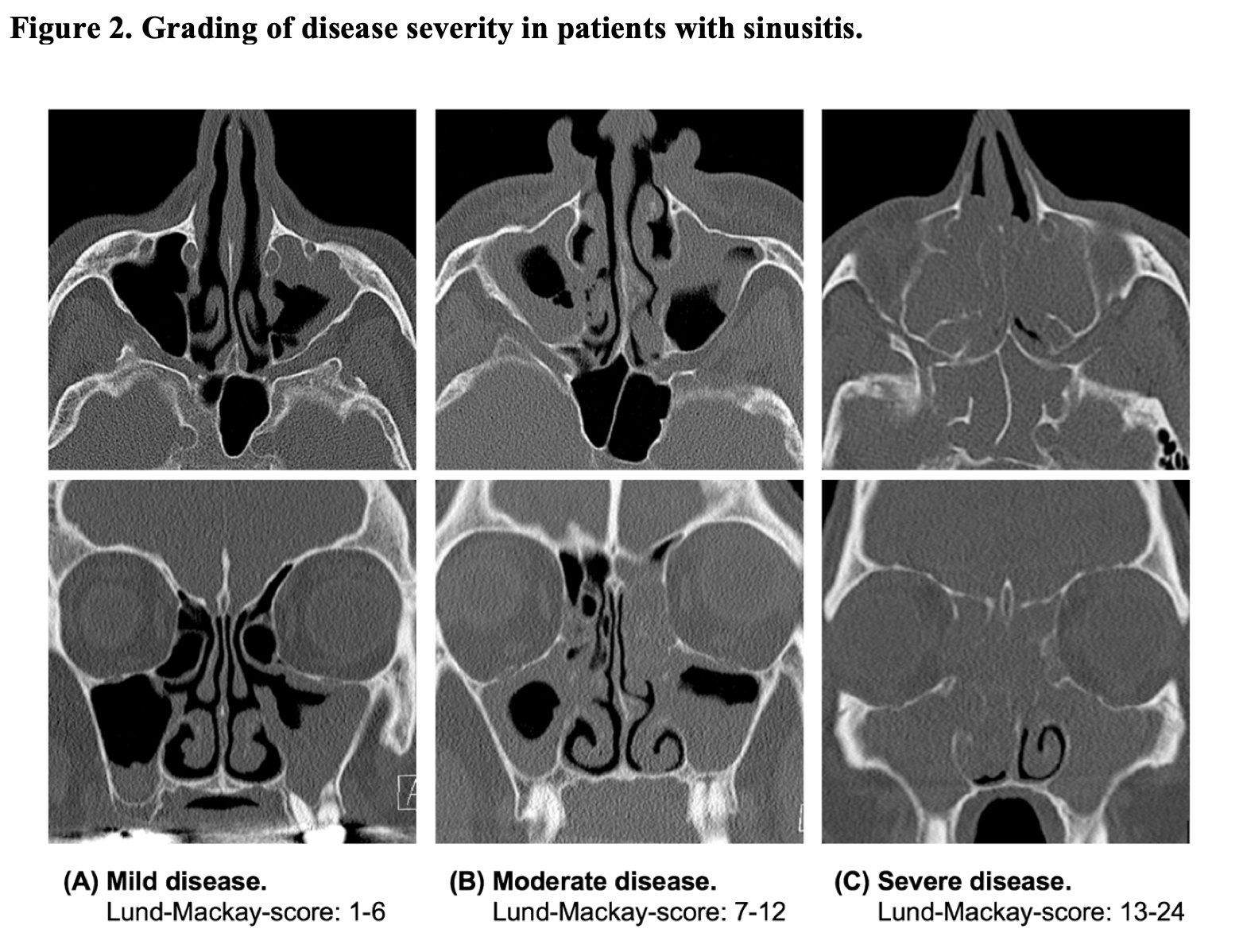
Table 4: Prevalence and severity of sinusitis according to Lund-Mackay-Score.
|
Parameter |
Patients (n=234) |
|
RS Status |
|
|
No RS present |
191 (81.6%) |
|
RS present |
43 (18.4%) |
|
Acute RS |
22 (9.4%) |
|
Chronic RS |
21 (9.0%) |
|
Severity of RS according to Lund-Mackay-Score |
|
|
Mild (Scores 1-6) |
36 (84.0%) |
|
Moderate (Scores 7-12) |
6 (14.0%) |
|
Severe (Scores 13-24) |
1 (2.0%) |
Table 5: Clinical data in correlation with the presence of RS.
|
|
Absences of RS |
Acute RS |
Chronic RS |
|
Age [years; mean ± SD (range)] |
54.1 ± 10.0 (21.2-71.0) |
54.2 ± 9.6 (34.7-67.9) |
56.0 ± 6.5 (47.1-70.0) |
|
Male [n (%)] |
130/163 (79.8)% |
16/163 (9.8)% |
17/163 (10.4)% |
|
Female [n (%)] |
61/71 (85.9)% |
6/71 (8.5)% |
4/71 (5.6)% |
|
MELD [mean ± SD (min, max)] |
15.7 ± 6.4 (6-36) |
16.4 ± 7.8 (6-34) |
15.3 ± 5.0 (7-26) |
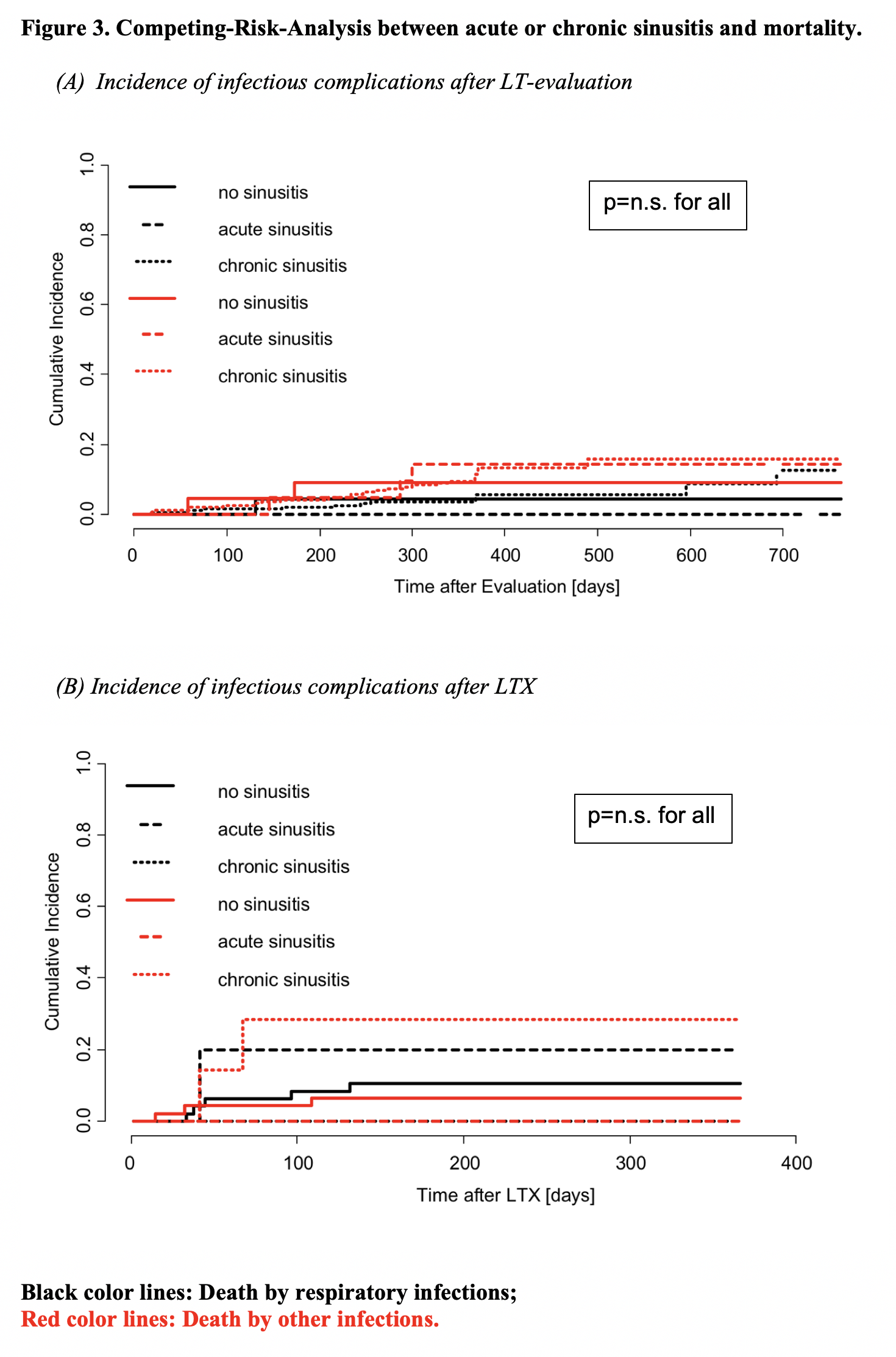
Table 6: Comparison of infectious complications after liver transplantation between patients with and without sinusitis distributed to nasopharyngeal surgery.
|
Infectious complications after LTX |
Patients with sinusitis without sinus surgery (n=10) |
Patients with sinusitis with sinus surgery before LTX (n=2) |
Patients without sinusitis (n=47) |
p-value |
|
No infectious complications |
2 (17%) |
0 (0%) |
9 (19%) |
p = 0.87 |
|
Respiratory infections/infections related to sinusitis |
7 (70%) |
2 (100%) |
21 (45%) |
p = 0.70 |
|
Other infections (e.g. urinary tract infections, cholangitis, pancreatitis) |
4 (40%) |
2 (100%) |
32 (68%) |
p = 0.88 |
Radiation dose estimates
CTDIVOL ranged between 2.2–3.1 mGy with a mean value of 2.7 ± 0.3 mGy. The mean DLP was 37.7±2.9 (range, 31.7–42.2). The effective dose during CT pns was noted between 0.6-0.8 mSv (mean, 0.07 ± 0.01 mSv).
Conclusion
A thorough evaluation of LT candidates is considered a prerequisite for a successful outcome after liver transplantation. Current guidelines give specific and detailed information on cardiopulmonary assessment and screening for generalized infections like cytomegalovirus infection, but hardly concrete recommendations concerning the work-up of infectious foci. Thus, LT centers are faced with the problem to conduct a comprehensive evaluation but also to avoid unnecessary and putative harmful diagnostics despite a lack of data and subsequently general recommendations. The prevalence of RS in the general population is substantial, and thus the management of LT candidates with RS a clinical important issue [11]. The current study is to our knowledge the largest assessment of RS in LT candidates in a Western population as only one former study investigated the prevalence of RS in 142 patients before solid organ transplantation including 79 patients scheduled for LT 19, while two other trials reviewed sinusitis in Asian liver graft recipients and were therefore not feasible to evaluate the prevalence in LT candidates[12,13].
The objective of the current study was to evaluate whether routine screening for sinusitis in unselected LT candidates by CT pns is mandatory and reasonable. Indeed, the overall prevalence of sinusitis was in a range that may justify CT pns screening. Moreover, the radiation exposure in the population of LT candidates has to be considered clinical not significant given the mortality of end-stage liver disease without LT. On the other hand, roughly eighty percent of screened patients did not show RS. Furthermore, even within the subcohort pf patients with acute or chronic RS, RS was mostly mild or moderate, which is in line with another study on different solid organ transplantation candidates[19]. Finally, presence of RS was not associated with mortality on the waiting list or after LT in our current study. Indeed, nasopharyngeal surgery, which was based on clinical symptoms and imaging, was done only in a minority of patients with RS identified by CT pns. The successful course in the patients with RS but without surgical treatment prior LT may indicate that at least mild RS is of minor clinical importance in LT candidates and with respect to the course after LT. Although our study was retrospective and the number of patients with RS who received respective surgery, it may be concluded that screening for RS bei CT pns in unselected patients is not mandatory. Nevertheless, radiological evaluation of RS seems reasonable in patients with symptomatic or prior history of RS, not least to decide about surgical treatment. Of note, nasopharyngeal surgery was not associated with major complications in LT candidates in our study, but the absolute number of patients with NS surgery was too low to draw any conclusions on this topic.
Two other studies have investigated prevalence and clinical impact in liver graft recipients, and thus not in the complete cohort of LT candidates. These studies have shown discrepant results concerning the issue whether the presence of unresolved RS was associated with increased mortality in the context of LT or not[12,13]. In detail, one study in Asian patients transplanted between 1995 and 2005 reported that chronic, untreated RS was not associated with mortality after LT[13]. In contrast, a further well conducted but also retrospective study reported that mortality after LT was higher in patients with unresolved chronic RS than in those who received nasopharyngeal surgery[12]. However, within this mentioned study, CT pns was performed in selected patients only. Moreover, liver graft recipients with untreated sinusitis had a higher MELD score and more infections compared to those with surgically treated sinusitis in this study. Although the differences were not statistically significant, it was suggested by the authors that the higher mortality rate might be associated rather with a more severe liver disease than unresolved sinusitis[12].
Strength of our current analysis is that prevalence and severity of RS in LT candidates by CT pns was determined prospectively without any pre-selection, and that the impact of resolved and unresolved RS on the clinical impact after LT was determined in a subgroup of the entire evaluation cohort, which may be assumed to reduce selection bias. Moreover, sinusitis was discriminated in acute and chronic course, and severity of RS was reliably determined by a validated score. Nevertheless, some limitations of the current study have to be taken into account. Data analysis was done retrospectively and the absolute number of patients with sinusitis was limited. Indication for nasopharyngeal surgery was based on an interdisciplinary but individual approach and respective criteria had not been defined by a study protocol. Therefore, analyses of subgroups, e.g. patients with or without surgically treated sinusitis, have to be considered not statistically resilient. Then again, our study is the largest analysis on this topic outside Asia, and given the limited number of analyses on this important issue, the data of our study may help to optimize the evaluation process in LT candidates.
In conclusion, although the prevalence of RS in LT candidates in a Western population detectable by CT pns is notable, most episodes are mild and the impact of RS on the clinical course prior and up to one year after LT seems of minor significance. The authors therefore suggest performing CT pns not in unselected LT candidates. Instead, a step-up approach and use of CT pns only in symptomatic patients or patients with a history of RS seems more reasonable. Nasopharyngeal surgery may be safely performed in LT candidates, but be offered preferable symptomatic patients with more severe disease prior LT.
Conflict of Interest: No conflicts of interest.
References
- 1. Schoening, W.N., Buescher, N., Rademacher, S., et al. Twenty-year longitudinal follow-up after orthotopic liver transplantation: a single-center experience of 313 consecutive cases. (2013) Am J Transpl 13(9): 2384-2394.
- 2. Adam, R., Karam, V., Delvart, V., et al. Evolution of indications and results of liver transplantation in Europe. A report from the European Liver Transplant Registry (ELTR). (2012) J Hepatol 57(3): 675-688.
- 3. Taniguchi, M. Liver transplantation in the MELD era--analysis of the OPTN/UNOS registry. (2012) Clin Transp l: 41-65.
- 4. Bajaj, J.S., O’Leary, J.G., Reddy, K.R., et al. Survival in infection-related acute-on-chronic liver failure is defined by extrahepatic organ failures. (2014) Hepatology 60(1): 250-256.
- 5. D’Amico, G., Morabito, A., D’Amico, M., et al. Clinical states of cirrhosis and competing risks. (2018) J Hepatol 68(3): 563-576.
- 6. Ohe, H., Hoshino, J., Ozawa, M. Factors affecting outcomes of liver transplantation: an analysis of OPTN/UNOS database. (2011) Clin Transpl 39-53.
Pubmed | Crossref | Others
- 7. European Association for the Study of the Liver. Electronic address: easloffice@easloffice.eu. EASL Clinical Practice Guidelines: Liver transplantation. (2016) J Hepatol 64(2): 433-485.
- 8. Martin, P., DiMartini, A., Feng, S., et al. Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. (2014) Hepatology 59(3): 1144-1165.
- 9. Fischer, S.A., Lu, K., AST Infectious Diseases Community of Practice. Screening of Donor and Recipient in Solid Organ Transplantation. (2013) Am J Transpl 13(s4): 9-21.
- 10. Fagiuoli, S., Colli, A., Bruno, R., et al. Management of infections pre- and post-liver transplantation: report of an AISF consensus conference. (2014) J Hepatol 60(5):1075-1089.
- 11. Dykewicz, M.S., Hamilos, D.L. Rhinitis and sinusitis. (2010) J Allergy Clin Immunol 125(2): S103-S115.
- 12. Hong, S.D., Jang, M.S., Cho, H.J, et al. Sinonasal evaluation and treatment before liver transplantation: a retrospective review of 982 patients. (2015) Eur Arch Otorhinolaryngol 272(4): 897-903.
- 13. Moon, B.J., Han, J.H., Jang, Y.J., et al. Effect of chronic rhinosinusitis on liver transplant patients. (2009) Am J Rhinol Allergy 23(5): 492-496.
- 14. Zielsdorf, S.M., Kubasiak, J.C., Janssen, I., et al. A NSQIP Analysis of MELD and Perioperative Outcomes in General Surgery. (2015) Am Surg 81(8): 755-759.
- 15. The, S.H., Nagorney, D.M., Stevens, S.R., et al. Risk Factors for Mortality after Surgery in Patients With Cirrhosis. (2007) Gastroenterology 132(4): 1261-1269.
- 16. Lund, V.J., Mackay, I.S. Staging in rhinosinusitus. (1993) Rhinology 31(4): 183-184.
Pubmed | Crossref | Others
- 17. Fulmer, S., Kim, S., Mace, J.C., et al. Hematopoietic stem cell transplantation and rhinosinusitis: the utility of screening sinus computed tomography. (2012) Laryngoscope 122(12): 2647-2651.
- 18. Deak, P.D., Smal, Y., Kalender, W.A. Multisection CT protocols: sex- and age-specific conversion factors used to determine effective dose from dose-length product. (2010) Radiology 257(1):158-166.
- 19. Tomazic, P., Neuschitzer, A., Koele, W., et al. Feasibility of routine paranasal sinus CT-scans in preoperative transplant patients. (2011) Ann Transpl 16(2): 31-35.












