Prevention of Blood Aspiration Syndrome due to Ruptured Uterus Associated with Birth Asphyxia in a Full Term Neonate
Wafaa Alharthy1, Atia Alzahrani1, Osama Alzyaat2, Mahmoud Aboalazm2
Affiliation
1Neonatal Intensive Care Unit, Maternity and Children Hospital, Makkah, KSA
2Department of Obstetrics & Gynecology, MCH, Makkah, KSA
Corresponding Author
*Corresponding Author: Ahmed Ahmed Elkhirshy, MRCPCH, MSc Paediatrics, MBBCH. Department of Neonatology, Maternity and Children Hospital, Makkah 21955, KSA.E-mail: akhirshy@yahoo.com
Citation
Elkhirshy, A.A. et al. Prevention of Blood Aspiration Syndrome due to Ruptured Uterus Associated with Birth Asphyxia in a Full Term Neonate. (2015) J Gynecol Neonatal Biol 1(2): 37-38.
Copy rights
©2015 Elkhirshy, A.A. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Blood aspiration syndrome; Respiratory distress; Surfactant; Birth asphyxia
Abstract
Blood aspiration syndrome is a distinct diagnostic entity that can result in significant respiratory distress in the neonate due to secondary surfactant deficiency. Few cases were reported with blood aspiration syndrome and surfactant therapy was tried in some cases. I reported one case of blood aspiration syndrome associated with birth asphyxia due to ruptured uterus, where blood aspiration using the meconium aspirator was done to decrease the blood load to the alveoli to prevent secondary surfactant deficiency. Blood aspiration syndrome, if suspected, a trial of blood aspiration should be tried to avoid secondary surfactant deficiency. More observations and judgments are needed to define and explain the indications for blood aspiration in cases of blood aspiration syndrome
Introduction
Blood aspiration syndrome is a distinct diagnostic entity that can result in significant respiratory distress in the neonate[1]. Blood in alveolus leads to a significant biochemical and functional disturbance of the surfactant system and inhibits production[2].
Secondary surfactant deficiency or dysfunction occurs in newborn respiratory disorders, including meconium aspiration syndrome, pneumonia and pulmonary hemorrhage. A variety of substances, including albumin, meconium and blood inhibit surfactant function[3-5].
I reported a case of prevention of imminent blood aspiration syndrome due to ruptured uterus associated with birth asphyxia in a full term neonate.
Case report
Full term neonate (38 Weeks) delivered by caesarian section (C.S.) to 30 years old mother with previous C.S., came to obstetrics emergency with labor pains shifted immediately to or due to fetal distress (CTG revealed fetal decelerations), where C.S. was done under general anesthesia, ruptured uterus was found due to scar dehiscence and the baby was in the abdominal cavity covered with blood, I received the baby flat (non-vigorous), covered with blood, HR was 80bpm, suction of the mouth and nose revealed blood and blood clots, positive pressure ventilation was done by self-inflating bag and mask with good response (HR was 120 and Spo2 was 90%) but no spontaneous breathing at the age of 2 minutes, so attempt of intubation by EET was tried which revealed good amount of blood coming through ETT, so blood aspiration syndrome was suspected. Blood aspiration was done using the meconium aspirator and ETT in the same technique used in meconium aspiration, blood was aspirated 3 times, then PPV was done followed by intubation by ETT as still no spontaneous breathing, at the age of 5 minutes and connected to mechanical ventilator, Spo2 was 96%, HR was 150 bpm. Apgar score was 1, 4, 4, 6 and 7 at 1, 5, 10, 15 and 20 minutes respectively and his cord blood gas was PH 6.9, Pco2 78.5, BE -15.9, Hco3 9.1. The baby was shifted to NICU with initial ventilator parameters (Dräger Babylog® 8000 plus) of AC mode PIP 18, PEEP 5, ventilator rate 50 and Fio2 0.3 with equal pre and post-ductal Spo2, maintaining vital signs with initial CBG of PH 7.39, Pco2 33.5, BE -3.8, Hco3 21.8.
The baby was fulfilling the criteria of hypothermia therapy (due to birth asphyxia) in the form of cord PH > 7, cord BE > -12, PPV for more than 10 minutes and Apgar score < 5 at 10 minutes, hypothermia was continued for 72 hrs and rewarming was done over 10 hrs.
The baby was weaned from mechanical ventilator and extubated at the age of 48 hrs to room air. Subtle seizures in the form of lip smacking and staring look were observed, so phenobarbital was added to the management, CT brain at the age of 4 days was normal with no more seizures. LDH and CPK were initially high, and fortunately other laboratory tests were within normal limits including full blood counts, renal function tests and liver function tests. The baby was doing fine and discharged home with normal neurological examination with full oral feedings.
Discussion
Aspiration of maternal blood has been previously implicated as a cause of respiratory distress in term and preterm newborns[6].
Gordon and his colleagues reported three cases of respiratory distress due to blood aspiration syndrome[1].
Elements in blood such as proteins and lipids cause surfactant dysfunction through several mechanisms that include competitive binding to the alveolar space[7].
Celik and his colleagues reported a case of blood aspiration syndrome needed a course of surfactant therapy due to secondary surfactant deficiency[2].
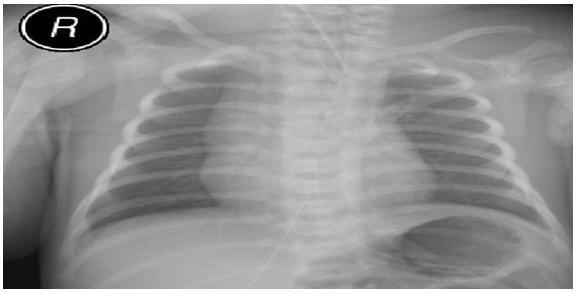
In our case, blood was aspirated by ETT using the meconium aspirator with expected decreased blood load to the alveoli with evident clear lung fields (Figure 1) and rapid weaning from mechanical ventilator, so surfactant therapy was not indicated.
Figure 1: Chest X-ray showing clear lung fields (4hrs of age).
To my knowledge this the first reported case of suspected blood aspiration syndrome where blood aspiration was done to decrease the blood load to the alveoli to avoid secondary surfactant deficiency.
In conditions such as ruptured uterus, blood aspiration syndrome should be suspected in non-vigorous babies and blood aspiration using same technique for meconium aspiration syndrome should be tried to decrease the blood load to the alveoli to prevent secondary surfactant deficiency.
In our case the patient was not fulfilling the typical criteria (clinically and radiologically) of Blood aspiration syndrome as blood was aspirated using the prescribed technique which prevented Blood Aspiration Syndrome from happening, which needs more research and trials.
More observations and judgments are needed to define and explain the indications for blood aspiration in cases of blood aspiration syndrome.
References
- 1. Gordon, E., South, M., McDougall, P.N., et al. Blood aspiration syndrome as a cause of respiratory distress in the newborn infant. (2003) J Pediatr 142(2): 200–202.
- 2. Celik, I.H., Demirel, G., Canpolat, F.E., et al. Surfactant therapy for maternal blood aspiration: an unusual cause of neonatal respiratory distress syndrome. (2012) Indian J Pediatr 79(10): 1358-1359.
- 3. Dargaville, P.A., South, M., McDougall, P.N. Surfactant and surfactant inhibitors in meconium aspiration syndrome. (2001) J Pediatr 138(1): 113–115.
- 4. Dargaville, P.A., Morley, C.J. Overcoming surfactant inhibition with polymers. Acta Paediatr (2000) 89(12): 1397–1400.
- 5. Tashiro, K., Kobayashi, T., Robertson, B. Dextran reduces surfactant inhibition by meconium. (2000) Acta Paediatr 89(12): 1439–1445.
- 6. Pender, C.B. Respiratory distress in the newborn infant due to blood aspiration in infant delivered by cesarean section. (1970) Am J Obstet Gynecol 106(5): 711-717.
- 7. Wang, Z., Notter, R.H. Additivity of protein and nonprotein inhibitors of lung surfactant activity. (1998) Am J Respir and crit care Med 158(1): 28-35.