Scrotal Swellings Synopsis of Differential Diagnosis (Part III)
Ruchi Sehgal , Deepa Sehgal , Shyam S Pandey , Syed S Amin , Sambit N Bhattacharya , Rakesh Oberai
Affiliation
- 1Dermato-Venereology (Skin/VD) Centre Sehgal Nursing Home, Panchwati, Delhi, India
- 2Department of Dermatology and Venerology, Institute of Medical Sciences, Banaras Hindu University, Varanasi
- 3Department of Dermatology and Venerology, J N Medical College, Aligarh Muslim University, Aligarh
- 4Dermatology and STD, University College of Medical Sciences and associated GTB Hospital, Delhi, India
- 5Department of Radiology, Sri Balaji Action Medical Institute Paschim Vihar, New Delhi, India
Corresponding Author
Virendra N. Sehgal, MD, Dermato-Venerology (Skin/VD) Center, Sehgal Nursing Home, A/6 Panchwati, Delhi-110 033, India, Tel: 9810182241; E-mail: drsehgal@ndf.vsnl.net.in ; sehgalvn@yahoo.co.in
Citation
Sehgal, V.N., et al. Scrotal Swellings Synopsis of Differential Diagnosis (Part III). (2016) Invest Dermatol Venereol Res 2(2): 84- 90.
Copy rights
© 2016 Sehgal, V.N. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Angioederma; Lichen simplex; Chronicus; Orchitis; Epididimitis; Epididmo- orchitis; Vericocele; Hydrocele; Inguinal hernia
Abstract
Scrotal swellings enshrine clinical conditions affecting dermis and /or sub-cutaneous tissue, and those of scrotal contents. A clear cut insight into their symptoms and signs are imperative to comprehend before arriving at their precise diagnosis. A concerted endeavor in this direction has been made to appraise the audience with their nomenclature origin, clinical variants, presentation and clear cut diagnostic criteria. Accordingly angioedema, lichen simplex chronicus, orchitis, epididymitis related epididymo- orchitis, varicocele, testicular torsion, and hydrocele formed the subject matter. The role of Ultrasonography, Ultrasonic colour doppler imaging and magnetic resonance imaging in evaluating scrotal swellings has succinctly been emphasized to enrich the core curriculum of the viewers.
Introduction
`Vivid recitation of anatomy and physiology is paramount to take stock of swelling(s) of any of the structures of the scrotum, the salient features of which formed walk the talk through illustrations[1]. Swelling, turgescence or tumefaction is a transient abnormal enlargement of a body part and /or its anatomical constituents not caused by proliferation of cells[2]. It is caused by accumulation of fluid in tissues. It can occur throughout the body (generalized), or a specific part or organ can be affected (localized). Scrotum being one of the pre-eminent parts. The scrotal swellings[3-5] are menacing challenging proposition affecting any of its structures starting with affliction of the skin in the form of angioderma[6]; acquired angioderma(AAE)[7] and hereditary angioderma (HAE)[8] and lichen simplex chronicus (LSC)[9]. Besides, inflammation of the testis, the orchitis[10,11], epididymis, the epididimitis[11-13], and /or epididmo-orchitis[14,15], pampiniform plexus, the Vericocele[16], testicular torsion[17], and collection of fluid in the tunica vaginalis testis, the Hydrocele[18] and exit/ slipping of small bowel into the scrotum, the inguinal hernia are its other presentations. It is, therefore, worthwhile to take stock of these conditions by their salient clinical presentation, diagnosis criteria including investigation like Ultrasonography[19], Ultrasonic colour Doppler imaging[20] and magnetic resonance imaging (MRI)[21,22] to form the perspective clinical diagnosis. Accordingly, their cardinal briefs are defined in the adjoining tables (table 1 to 4) for at a glance evaluation.
Scrotal swellings of dermis and sub-cutaneous tissue
Angioedema (Figure. 1a), lichen simplex chronicus (Figure. 2a & b): Nomenclature, clinical variants, salient presentation and diagnostic criteria are outlined in Table 1.
Figure 1: Scrotal swellings: Acquired angioedema affecting the scrotum.
Figure 2a&b: Scrotal swellings: Depicting lichen simplex chronicus.
Table 1: Scrotal Swellings: Angioedema and Lichen simplex chronicus (LSC).
| Nomenclature | Clinical variants | Presentation | Diagnostic criteria |
|---|---|---|---|
| Angioedema[6], angiooedema, /Quincke'sedema,/ angioneurotic edem | Acquired angioedema (AAE)[7] Recurrent transitory swelling affecting the face, lips, tongue, limbs, and genitals, meditation by angiotensin-converting-enzyme inhibitor (ACE inhibitor) Hereditary angioedema(HAE)[8] Caused by a genetic mutation inherited in an autosomal dominant form, distinguished by the underlying genetic abnormality. |
In addition to the clinical picture supplement of haemogram, serum, electrolytes, liver and kidney functions are mandatory | Clinical as well as laboratory test, inhibitor of complement enzyme, C1 esterase (C1INH) for HAE[23] |
| Rapid swelling, edema of the dermis, subcutaneous tissue, mucosa and sub mucosal tissues. | |||
| Lichen simplex chronicus (LSC) [9,24] | Lichen amyloidosis[10,25,26] | Intense, intermittent pruritus, scrotal erythema and edema Erectile dysfunction(ED)[27] | Stable pruritic plaque(s), marked by thickening, pigmentation exaggerated skin markings, the lichenification complemented by histopathology. |
| Thickening of the skin, variable scaling arising secondary to repetitive scratching / rubbing. | The re-crossed keratinocytes that forms keratinocytes-derived amyloid in the dermis. |
Scrotal swellings of the contents of the scrotum Orchitis, Epididymitis and Epididymo-orchitis (Figure 3). The origin of nomenclature, clinical variants, presentation and diagnostic criteria are succinctly defined in the adjoining (table 2)
Figure 3: Scrotal swellings: Epididymo-orchitis.
Table 2: Scrotal Swellings: Orchitis, Epididymitis and Epididymo-orchitis.
| Nomenclature | Clinical variants | Presentation | Diagnostic criteria |
|---|---|---|---|
| Orchitis[10,11,28] | Vide infra | painful urination/ ejaculation, Swollen and tender scrotum, Blood stained semen or abnormal discharge, Enlarged prostate, Enlarged groin lymph nodes and fever. | Inferno[29] Brown novel) colour Doppler ultrasound, a sign of orchitis. |
| Inflammation of the testicles caused either by bacteria or virus, affecting one or both | |||
| Epididymitis[11,12,28,30] Discomfort or pain[31] |
Acute, Chronic | Chills, low-grade fever, Pain/discomfort in the pelvic area, painful, red, warn and swollen scrotum, pain and tenderness in the testicles, enlarged groin lymph nodes, painful, frequent urination or bowel movements, painful intercourse and ejaculation. | Clinical Vide-infra see below |
| Epididymo-orchitis[14,15,32,33] | Acute gonococcal[34] / non-gonococcal urethritis (NGU)[35-40]/ non specific urethritis (NSU), Chronic | Rapid swelling of epididymis and testis in a short course, a day or so. Painful, enlarged, tender and red scrotum. |
Gram Stain of Urethral is charge with Intracellular Neisseria, gram-negative diplococcai Chlamydia trachomatis[41] Testing Sensitivity in Midstream urine specimens |
| Inflammation of the epididymis and/or testis |
Varicocele and testicular torsion: The origin of nomenclature, clinical variants, presentation, and diagnostic criteria are shown for at a glance diagnosis in (table 3)
Table 3: Scrotal Swellings; Varicocele; Testicular torsion
| Diagnosis | Clinical variants | Presentation | Diagnostic criteria |
|---|---|---|---|
| varicocele[16,28,42] enlargement of pampiniform plexus resulting from engorgement / swollen veins apparent as a testicular swelling, variable age group being 13-30 years. Classified into Grade 1: Smallest size Grade 2: Size between Grade 1 and 2 Grade 3: Largest size |
Idiopathic /Pri-mary varicocele Secondary varicocele |
Visible/palpable enlarged veins Dragging/ aching scrotal pain/ heaviness Atrophy of the testicle(s) Benign prostatic hyperplasia (BPH) Infertility[43,44] |
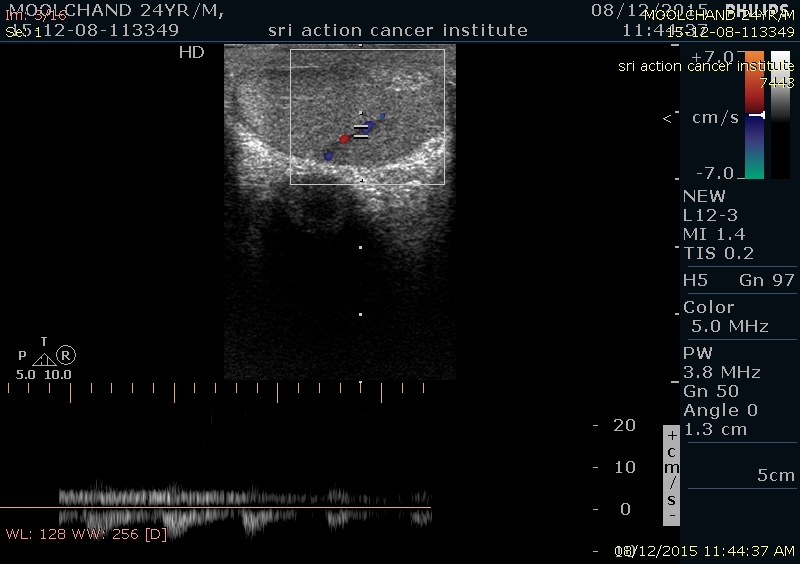
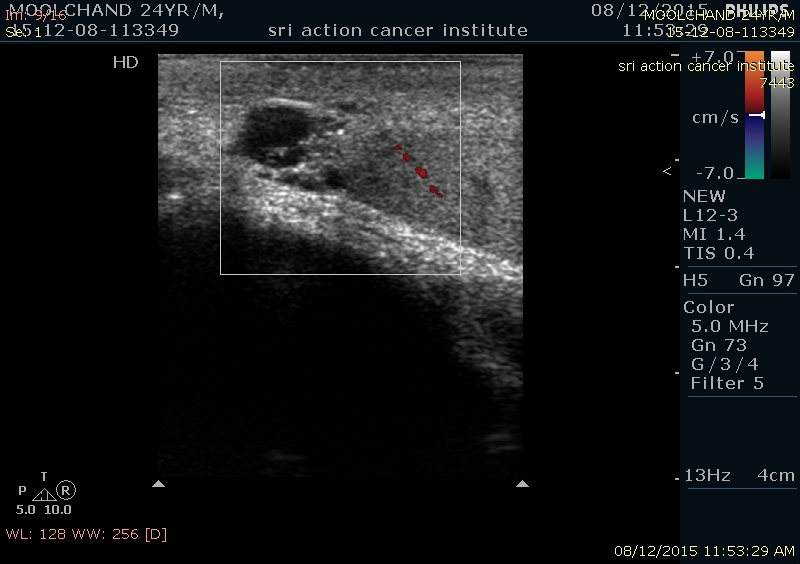
Changing levels of testosterone ColorDoppler ultrasound (CDU)[46] presence of a venous plexus and the sum of the diameters of veins in the plexus change of flow on Valsalva maneuver / manoeuvre (Fig. 4, fig. 5) |
| Testicular torsion:[17,47-49] Twisting of the spermatic cord resulting in ischemia of the testicles |
Congenital | Sudden, severe, testicular pain and tenderness in the groin and lower abdomen | Clinical color ultrasound scan of the scrotum, eliciting absence of blood flow in the twisted testicle[50] |
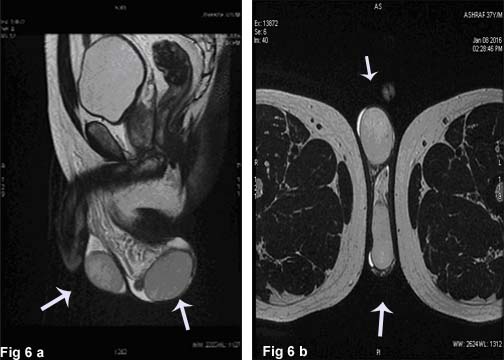
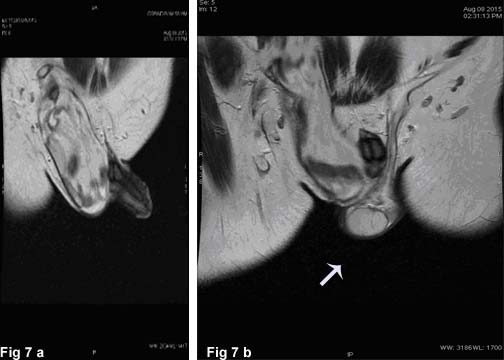
Hydrocele Testis and Inguinal Hernia: There nomenclature’s origin clinical variants, presentation, and diagnostic criteria are shown in table 4, Fig 4, 5 (Figure 6a & b)
Figure 4: Bilateral testis showing normal flow.
Figure 5: Color Doppler image showing multiple veins dilated and filling up on valselva maneuver. The pampiniform vein measures 4 mm.
Figure 6a&b: Scrotal swellings: Hydrocele depicting scrotal swelling.
Table 4: Scrotal Swellings: Hydrocele Testis and Inguinal Hernia.
| Diagnosis | Clinical variants[53] | Presentation | Diagnostic criteria |
|---|---|---|---|
| Hydrocele Testis[51-53] Hydrocele testis a painless swelling of the scrotum due to circumscribed collection of fluid in the tunica vaginalis testis |
Primary hydrocele | Soft, non-tender, large swelling, non palpable testis Trans-illumination positive |
Ultrasound mandatory for testicular visualization |
| Secondary hydrocele due to disease(s) of testis. Acute/chronic epididymo-orchitis,Torsion of testis Testicular tumor Hematocele Filarial hydrocele Post herniorrhaphy Hydrocele of an hernial sac |
Fluctualating, non-reducible swelling No cough impulse It is more of a symptom than an actual pathological entity Palpation of testis impossible except for funicular and encysted hydrocele Trans-illumination elicitable |
Diffusion-weighted MRI of the testis[54] Apparent diffusion co-efficient (ADC) Reduced ADC values of testis, indicating reduced diffusion of the testis, with an increasing amount of fluid.(Fig 7a & b) |
|
| Infantile hydrocele | Infertility(?)[55] | ||
| Congenital hydroceles | |||
| Encysted hydrocele of the cord | |||
| Inguinal hernia | Groin hernia Herniation of small bowel through the external inguinal ring to scrotum. |
Apparent, reducible scrotal swelling Pain/discomfort while coughing, exercise, or bowel movements. |
Magnetic resonance imaging (MRI)[57] a diagnostic tool of high predictive value |
| An exit/slipping of a bowel from the abdomen through the wall of the cavity into the scrotum[51,56]. It may either be direct or indirect hernias, which may or may not extend down to the scrotum. | |||
| Femoral hernia Herniation of part of the abdominal contents, passing through weak area, the femoral ring at the posterior wall of the femoral canal. These swellings do not extend to the scrotum but rather are found below and lateral to the superficial inguinal ring |
Worsens in the day comfortable while lying. severe pain on strangulation |
Figure 7a&b: Scrotal swellings: Axial T2 Weighted images showing mild fluid in left scrotal sac (white arrow- left testis, white arrowheadright testis)
Synopsis of differential diagnosis
Scrotal swellings may either be of dermis, subcutaneous tissue or contents of scrotum, the utility of this diversification may prove beneficial, while preparing the instant day to day clinical dissertation. Besides, the afore mentioned conditions sarcoidosis[58] presenting as hydrocele (vide supra) and juvenile dermatomyositis(JDM)[59] charactererised by edema of the penis and scrotum should also be considered.
Multiple choice questions (MCQs)
1. Which of these aspects of the clinical history would alert you to a possible diagnosis of hereditary angioedema in a patient with angioedema?
a. Early onset of angioedema before early adulthood
b. Angioedema but no wheals
c. Family history
d. No history of laryngeal oedema
e. Prodromal symptoms
i. a, b and c
ii. a, b, c and e
iii. a, b, d and e
iv. a and d
v. a, b, c and d
Answer: ii
1. Which of the following is not a factor in the development of urticaria?
a. Activation of sensory nerves
b. Vasodilatation
c. Extravasation
d. Recruitment of pro-inflammatory cells
e. Separation of epithelial cells
Answer: e
2. For lichen simplex chronicus what is the single most important treatment?
a. Topical corticosteroids
b. Oral corticosteroids
c. The patient must bathe regularly
d. The patient must stop scratching
Answer: a
3. The epididymis is a _____ and it functions to _____.
a. compartment inside a testis; secrete testosterone and form sperm
b. stage of spermatogenesis; form two sperm cells and semen
c. tightly coiled tube on the outside of the testis; store immature sperm as they mature
d. compartment that contains seminiferous tubules; ejaculate sperm and semen out of the penis
Answer: c
4. Although epididymitis is uncommon in children, the most common cause of epididymitis is the
a. H. influenzae
b. Coliforms
c. Staph. Aureus
d. C. trachomatis
Answer: d
5. Choose the correct statement: - Hydrocele of the canal of Nuck
a. Is mostly observed in males.
b. Is usually found affecting females.
c. Is formed due to fluid collection in the femoral canal.
d. Is seen in children as well as adults.
e. Is a painful, translucent and reducible swelling.
Answer: b
6. Which of the following are not usually observed in epididymo-orchitis:
a. The epididymal tail is often more swollen than the head.
b. In the majority of case there is some oedema and swelling of the testis.
c. In the majority of cases there is a large hydrocele containing debris.
d. In some cases there is swelling of the spermatic cord.
e. The mumps virus causes orchitis without epididymitis.
Answer: c & d
7. In torsion of the testicular appendix, which of the following is incorrect?
a. The condition causes only mild pain.
b. The testis is relatively hypo-vasular on Doppler Study.
c. There is often swelling of the spermatic cord.
d. The condition does not occur in adults.
Answer: a
8. Varicocele is more common in left testis because :
a. Left testicular vein drains into IVC which has high pressure
b. Left testicular vein drains into left renal vein and has poor valve mechanism
c. Left testis is lower situated
d. Compression of testicular vein by rectum
Answer: b
9. Which of the following statements about the causes of inguinal hernia is correct?
a. Excessive hydroxyproline has been demonstrated in the aponeuroses of herniapatients.
b. Obliteration of the processus vaginalis is a contributing factor for the development of an indirect inguinal hernia.
c. Physical activity and athletics have been shown to have a protective effect toward the development of inguinal hernias.
d. Elevated levels of circulating serum elastase activity have been demonstrated in patients with direct herniation who smoke.
Answer: d
References
- 1. Malhotra, A., Sehgal, V.N., Lal, J.B. Scrotal Swellings: Scrotal anatomy and physiology (part I). (2016) Invest Dermatol Venereol Res 2(2): 1-3.
- 2. Swelling. Dorland's Illustrated Medical Dictionary (31st ed.). (2007) Saunders.
- 3. Eardly, L. Testis and scrotum in Bailey and Love’s Short Practice of Surgery edited by Williams N. S., Bulstrode, C.J.K., O’Connell, P.R., Boca Raton Florida. (2013) CRC Press 26th edition: 1377-1391.
- 4. Sehgal, V.N., Sehgal, N., Sehgal, R., et al. Acute scrotum: An Unusual presentation of Non-gonococcal/Non Specific Urethritis, Epididymitis and Orchitis Part II. (2015) Invest Dermatol Venereol Res 2(1): 1-3.
- 5. Kavooussi, Parviz, K., Costabile, et al. "Disorders of scrotal contents: orchitis, epididimitis, testicular tortion, tortion of the appendages, and Fournier's gangrene". (2011) In Chapple, Christopher R.; Steers, William D. Practical urology: essential principles and practice, London. Springer-Verlag.
- 6. Axelrod, S., Davis-Lorton, M. "Urticaria and angioedema". (2011) The Mount Sinai journal of medicine New York 78(5): 784–802.
- 7. Fain, O., Gobert, D., Khau, C.A., et al. Acquired angioedema. (2015) Presse Med 44(1): 48-51.
- 8. Muñoz Peralta, F., Buller Vigueira, E., Cabello Pulido, J. Hereditary angioedema type I: a case report. (2016) Medwave16 (1): e6378.
- 9. Pleimes, M., Wiedemeyer, K., Hartschuh, W. Lichen simplex chronicus of the anal region and its differential diagnoses: A case series. (2009) Hautarzt 60(11): 907-912.
- 10. Gruenberg, H. Three unusual cases of chronic orchitis clinically resembling tumors of the testis. (1926) Frankfurt Z Pathol 33: 217–227.
- 11. Walker, N.A., Challacombe, B. Managing epididymo-orchitis in general practice. (2013) Practitioner 257(1760): 21-25, 2-3.
- 12. Weidner, W., Schiefer, H.G., Garbe, C. Acute nongonococcal epididymitis: etiological and therapeutic aspects. (1987) Drugs 1: 111–117.
- 13. Mittemeyer, B.T., Lennox, K.W., Borski, A.A. Epididymitis: a review of 610 cases. (1966) J Urol 95(3): 390–392.
- 14. Taylor, S.N. Epididymitis. (2015) Clin Infect Dis 61(Suppl 8): S770-773.
- 15. Walker, N.A., Challacombe, B. Managing epididymo-orchitis in general practice. (2013) Practitioner 257(1760): 21-25, 2-3.
- 16. "Varicocele". Oxford Dictionaries. Oxford University Press. Retrieved 2016-01-21.
- 17. Cubillos, J., Palmer, J.S., Friedman, S.C., et al. Familial testicular torsion. (2011) J Urol 185(6): 2469-2472.
- 18. Beard, J.H., Ohene-Yeboah, M., Devries, C.R., et al. Hernia and Hydrocele. Editors (2015) The International Bank for Reconstruction and Development / The World Bank vol.1, Chapter 9.
- 19. Rizvi, S.A., Ahmad, I., Siddiqui, M.A., et al. Role of color Doppler ultra-sonography in evaluation of scrotal swellings: pattern of disease in 120 patients with review of literature. (2011) J Urol Winter 8(1): 60-65.
- 20. Pilatz, A., Wagenlehner, F., Bschleipfer, T., et al. Acute epididymitis in ultrasound: results of a prospective study with baseline and follow-up investigations in 134 patients. (2013) Eur J Radiol 82(12): 762-768.
- 21. Parker, R.A., Menias, C.O., Quazi, R., et al. MR Imaging of the Penis and Scrotum. (2015) Radiographics 35(4):1033-1050.
- 22. Watanabe, Y. Scrotal Anatomy at MRI. (2012) Scrotal Pathology Part of the series Medical Radiology 55-66
- 23. Frazer-Abel, A., Giclas, P.C. Update on laboratory tests for the diagnosis and differentiation of hereditary angioedema and acquired angioedema. (2011) Allergy Asthma Proc 17-21.
- 24. Pleimes, M., Wiedemeyer, K., Hartschuh, W. [Lichen simplex chronicus of the anal region and its differential diagnoses: A case series.]. (2009) Hautarzt 60(11): 907-912.
- 25. Weyers, W. [Lichen amyloidosis-disease entity or the effect of scratching]. (1995) Hautarzt 46(3): 165-172.
- 26. Weyers, W., Weyers, I., Bonczkowitz, M., et al. Lichen amyloidosis: a consequence of scratching. (1997) J Am Acad Dermatol 37(6): 923-928.
- 27. Juan, C.K., Chen, H.J., Shen, J.L., et al. Lichen Simplex Chronicus Associated With Erectile Dysfunction: A Population-Based Retrospective Cohort Study. (2015) PLoS One 10(6): e0128869.
- 28. Dorland's illustrated Medical Dictionary. (1981) W.B. Sauders Company 26th edition.
- 29. Artul, S., Abu Rahmah, Y., Abu Shkara, H., et al. Inferno: colour Doppler ultrasound sign of orchitis. (2014) BMJ Case Rep.
- 30. Kim, S.D., Kim, S.W., Yoon, B.I., et al. The Relationship between Clinical Symptoms and Urine Culture in Adult Patients with Acute Epididymitis. (2013) World J Men’s Health 31(1): 53-57.
- 31. Michel, V., Pilatz, A., Hedger, M.P., et al. Epididymitis: revelations at the convergence of clinical and basic sciences. (2015) Asian J Androl 17(5):756-763.
- 32. Johnson, T.B., Davies, D.V., Davis, F. Grey’s Anatomy 35th edn. (1973).
- 33. Nicholson, A., Rait, G., Murray-Thomas. T., et al. Management of epididymo-orchitis in primary care: results from a large UK primary care database. (2010) Br J Gen Pract 60(579): e407-e422.
- 34. Anonymous. Neisseria gonorrhea and gonococcal infections. (1978) World Health Organ Tech Rep Ser (616): 1-142.
- 35. Rane, V.S., Fairley, C.K., Weerakoon, A., et al. Characteristics of acute nongonococcal urethritis in men differ by sexual preference. (2014) J Clin Microbiol 52(8): 2971-2976.
- 36. Horner, P., Blee, K., O’Mahony, C., et al. UK National Guideline on the Management of Non-gonococcal Urethritis. (2014) International Journal of STD & AIDS: 1–12.
- 37. Frølund, M., Lidbrink, P., Wikström, A., et al. Urethritis-associated Pathogens in Urine from Men with Non-gonococcal Urethritis: A Case-control Study. (2015) Acta Derm Venereol 96(5):689-694.
- 38. Bradshaw, C.S., Tabrizi, S.N., Read, T.R., et al. Etiologies of non-gonococcal urethritis: bacteria, viruses, and the association with orogenital exposure. (2006) J Infect Dis 193(3): 336-345.
- 39. Workowski, K.A., Berman, S. Sexually Transmitted Diseases Treatment Guidelines. (2010) MMWR 59(12): 1-110.
- 40. Blaivas, M., Sierzenski, P., Lambert, M. Emergency evaluation of patients presenting with acute scrotum using bedside Ultrasonography. (2001) Acad Emerg Med 8(1): 90-93.
- 41. Mangin, D., Murdoch, D., Wells, J.E. Chlamydia trachomatis testing sensitivity in midstream compared with first-void urine specimens. (2012) Ann Fam Med10 (1): 50-53.
- 42. Li, H., Zhang, Y. Case of varicocele (2015) Zhongguo Zhen Jiu 35:1288. Chinese
- 43. Kantartzi, P.D., Goulis, D.C.H., Goulis, G.D., et al. Male infertility and varicocele: myths and reality. (2007) Hippokratia 11(3): 99–104.
- 44. Shridharani, A., Owen, R.C., Elkelany, O.O., et al. The significance of clinical practice guidelines on adult varicocele detection and management. (2016) Asian J Androl 18(2): 269-275.
- 45. Kantartzi, P.D. Update on the role of varicocele in male infertility. Master degree dissertation. Thessaloniki: 2006.
- 46. Chiou, R.K., Anderson, J.C., Wobig, R.K., et al. Color Doppler ultrasound criteria to diagnose varicoceles: correlation of a new scoring system with physical examination. (1997) Urology 50(6): 953-956.
- 47. Ringdahl, E., Teague, L. "Testicular torsion". (2006) Am Fam Physician 74(10): 1739–1743.
- 48. Nason, G.J., Tareen, F., McLoughlin, D., et al. Scrotal exploration for acute scrotal pain: A 10-year experience in two tertiary referral pediatric units. (2013) Scand J Urol 47(5): 418-422.
- 49. Sharp, V.J., Kieran, K., Arlen, A.M. Testicular torsion: diagnosis, evaluation, and management. (2013) American family physician 88(12): 835–840.
- 50. Bhardwaj, P. Role of Color Doppler in Scrotal Lesions. (2009) Indian J Radiol Imaging 19(3): 187–190.
- 51. Palmer, L.S. Hernias and hydroceles. (2013) Pediatr Rev 34(10): 457-464.
- 52. Clarke, S. Pediatric inguinal hernia and hydrocele: an evidence-based review in the era of minimal access surgery. (2010) J Laparoendosc Adv Surg Tech A 20(3): 305-309.
- 53. Griffiths, J. Varieties of Hydrocele of the Tunica Vaginalis Testis and some Anomalous States of the Processus Vaginalis. (1894) J Anat Physiol 28(3): 291–302.
- 54. Gulum, M., Cece, H., Yeni, E., et al. Diffusion-weighted MRI of the testis in hydrocele: a pilot study. (2012) Urol Int 89(2): 191-195.
- 55. Politoff, L., Hadziselimovic, F., Herzog, B., et al. Does hydrocele affect later fertility? (1990) Fertil Steril 53(4): 700-703.
- 56. Fitzgibbons, R.J. Jr., Forse, R.A. Clinical practice. Groin hernias in adults. (2015) The N Engl J Med 372(8): 756–763.
- 57. Van den Berg, J.C., De Valois, J.C., Go, P.M., et al. Detection of groin hernia with physical examination, ultrasound, and MRI compared with laparoscopic findings. (1999) Invest Radiol 34(12): 739-743.
- 58. Shahid, A, Khan. M.R.C.S., Jonathan, L, Richenberg., et al. FRCS Scrotal swelling in sarcoidosis. (2004) J R Soc Med 97(10): 487–488.
- 59. Sallum, A.M., Silva, M.F., Michelin, C.M., et al. Penile and scrotum swelling in juvenile dermatomyositis. (2011) Acta Reumatol Port 36(2): 176-179.