Stercoral Perforation of the Sigmoid Colon: A Case Report
Affiliation
St Mary’s Hospital, Loudong, Yilan, Taiwan
Corresponding Author
Swei H. Tsung, 160 S, Chungchong Rd, Loudong, Yilan, Taiwan, Tel: 886-3-954106/ext 7372; E-mail: tsung.sweihsiung@gmail.com
Citation
Tsung, S.H. Stercoral Perforation of the Sigmoid Colon: A case report. (2016) J Gastro Dis Liver Func 2(1): 56- 58.
Copy rights
© 2016 Tsung, S.H. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Stercoral perforation; Peritonitis; Sigmoid colon; Fecaloma; Constipation
Abstract
Stercoral perforation is a very dangerous, life-threatening situation that has a high mortality rate, and usually is diagnosed only during exploratory laparotomy. Stercoral perforation, in more than 90% of cases involves the sigmoid colon, resulting from ischemic pressure necrosis of the bowel wall, caused by fecalomas. The exact mechanism that causes fecalomas to form has yet to be defined clearly, but many factors such as a history of constipation, are thought to contribute. I report a rare case of stercoral perforation of sigmoid colon on a 86-year-old man who had been bed ridden because he was paraplegic due to CVA.
Introduction
The first case of stercoral perforation (SP) of colon was reported by Berry in 1894[1]. Fewer than 150 cases were reported in the English literature through 2011[2]. Today, SP is still unknown to many surgeons, gastroenterologists, and pathologists. SP is associated with high morbility and mortality rate. Awareness of this entity is important, because correct preoperative diagnosis can facilitate early surgical intervention, and prevent or mitigate serious complications. I report a rare case of stercoral perforation of sigmoid colon on an 86-year-old man who had been bed ridden because he was paraplegic due to CVA.
Case report
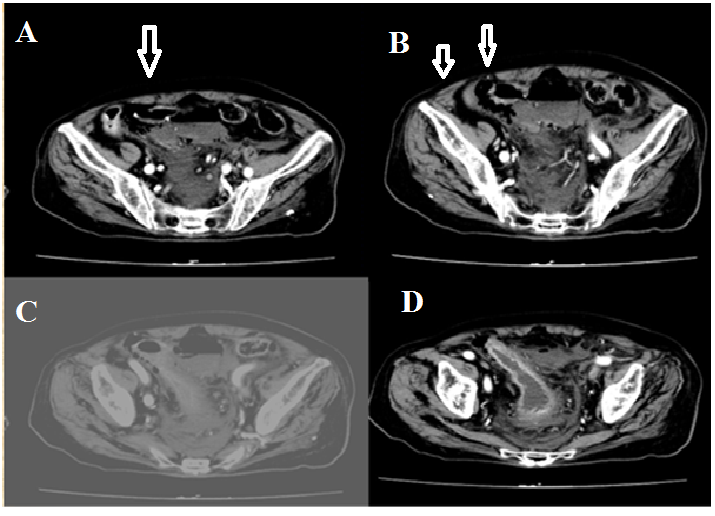
An 86-year-old male was admitted to the department of surgery through the emergency room with a chief complaint of fever, vomiting, production of thick sputum and bloody stool. On physical examination in the emergency room, his body temperature was 37.6°C, heart rate was 126 per minute, blood pressure was 79/52 mmHg, and respiratory rate was 27 per minute. His abdomen was distended with hypoactive bowel sound. He passed bloody stool in the emergency room. Laboratory examination showed that white blood cell count was 10,470 cells /mm³. Hemoglobin was 11.7 g/dl. Blood gas analyses revealed that pH was 7.43, PCO2 56, PO2 32. Abdominal CT revealed free air around the sigmoid colon and in the lower abdominal cavity (Figure 1). Perforation of hollow organ was suspected. He underwent an emergency exploratory laparotomy. Intraoperatively, there was an obvious perforation, approximately 3 x 2.0 cm at the sigmoid colon .A segmental resection and proximal colostomy was performed. Approximately 150 ml of turbid fluid was aspirated from the abdominal cavity. He had copious intraperitoneal lavage. His postoperative course was uneventful.
Figure 1: Image findings of computer tomography.
A. Perforation site (arrow).
B. Free air (arrow).
C. Peritoneal fluid level (arrow).
D. Thickening of bowel wall (arrow).
Past history reveal that the patient had been under nursing care for years, and had been bed ridden because he was paraplegic due to CVA. He had above knee amputaion of his right leg, and had a long time history of constipation.
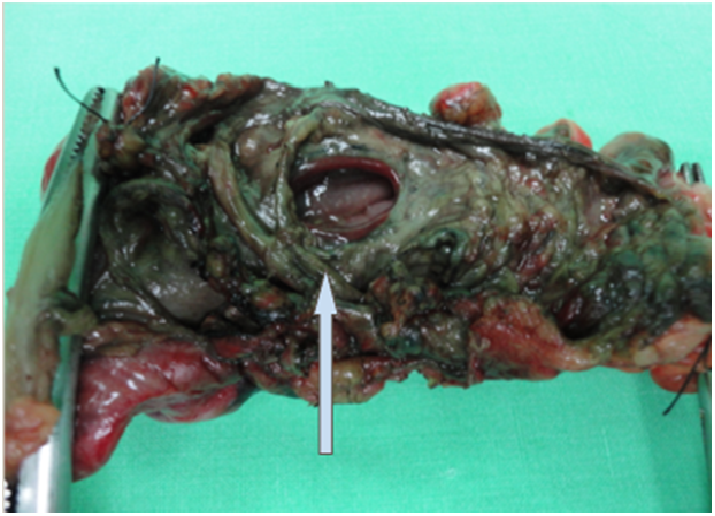
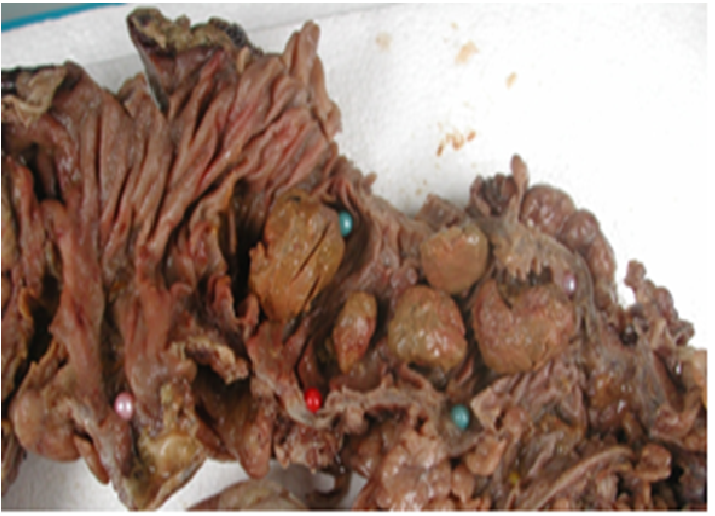
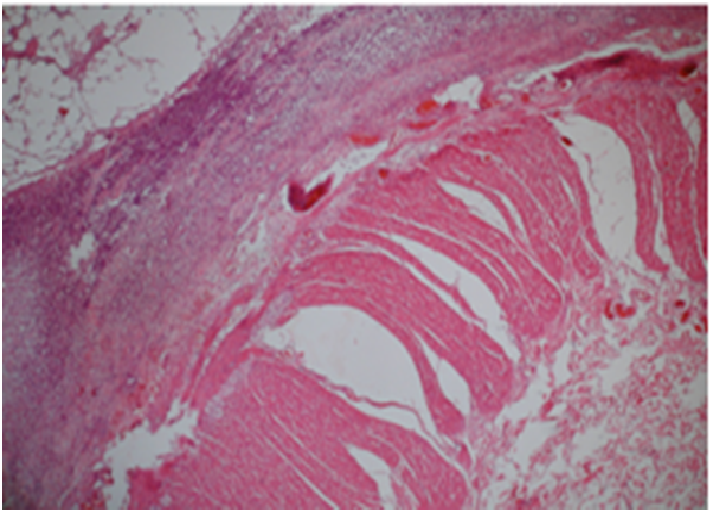
Pathology The specimen consisted of a segment of colon, 12 cm in length, with an oval perforation , 3 cm in its greatest dimension, on the antimesenteric site (Figure 2). The specimen was opened after fixed in formalin overnight. There were five fecalomas found[3](Figure 3). Histologic sections showed mucosal erosion, and transmural necrosis and fibropurulent exudates of the subserosa and on the serosal surface (Figure 4).
Figure 2: Oval perforation site at the antimesenteric border
Figure 3: Fecalomas in the lumen
Figure 4: Histology taken from the close proximity of the perforation site displaying fibropurulent exudates on the serosal surface
Discussion
SP is defined as “perforation of the bowel due to pressure necrosis from hard fecal masses”. SP of the colon has been reported to be 3.2% of all colonic perforation[3], and mortality rate of SP was maximal at 35% in the literature[4]. Possible reasons for the poor prognosis include an older patient age group and well-established fecal peritonitis at the time of surgery. SP usually occur in delibitated, bed-ridden, mentally ill or narcotic dependent patients[4]. The most influential factor in development of SP is chronic constipation. A review by Serpell and Nichols[4] noted only 61% of the reported cases had a significant history of constipation. Some reports suggested a link between the use of opioids, nonsteroidal anti-inflammatory drugs, antidepressents and SP[5,6]. It is well known that these drugs have constipation as a side effect.
The pathophysiology of stercoral perforation is considered to be formation of fecaloma causing pressure necrosis of the colon wall leading to ulceration, and ultimately perforation, usually located in the anti-mesenteric border of the descending colon, where the bowel wall has the lowest blood supply and narrowest diameter[7].
The diagnosis has been reported to pose a challenge to surgeons; although patients with SP always present acute abdomen with free gas below the diaphragm. The condition is rarely suspected, and patients are scheduled for emergency laparotomy for a hollow organ perforation.
The most useful tool for diagnosis of SP is abdominopelvic computed tomography (CT). On CT scan, findings of fecal impaction is obvious, with visualization of a dilated colon containing dense, lamellated fecal masses (fecalomas) , with focal colonic wall thickening[3,8]. If perforation occurs, free air below the diaphragm or in the pelvis adjacent to the sigmoid colon can be found. Sometimes, intra-luminal or extra-luminal air loculi are present[9].
For treatment of SP, resection of the involved colon and proximal colostomy was known as the treatment of choice. Evacuation of impacted fecaloma and identification of additional stercoral ulcers may result in avoidance of re-perforation and further complication. For this purpose, Huang et al.[7] suggested to perform intraoperative colonoscopy.
Conclusion
Fecal impaction is not an uncommon condition. Rarely, this can lead to formation of fecaloma resulting in stercoral colitis. If not treated promptly, perforation can occur, leading to peritonitis and death. The exact mechanism that causes fecaloma to develop in patients with or without a history of constipation has yet to be clearly defined. Further studies are needed to uncover what causes fecaloma to develop, so that their formation can be prevented, and SP can be voided.
References
- 1. Berry, J. Dilatation and rupture of sigmoid flexure short report. (1894) Br Med J 1:301.
- 2. Kumar, P., Pearce, O., Higginson, A. Imaging manifestation of faecal impaction and stercoral perforation. (2011) Clin Radiol 66(1): 83-88.
- 3. Maurer, C.A., Renzulli, P., Mazzucchelli, L., et al. Use of accurate diagnostic criteria may increase incidence of stercoral perforation of the colon. (2000) Dis Colon Rectum 43(7): 991-998.
- 4. Serpell, J.W., Nicholls, R.J. (1990) Stercoral perforation of the colon. Br J Surg 77(12): 1325-1329.
- 5. Patel, V.G., Kalakuntla, V., Fortson, J.K., et al. Stercoral perforation of the sigmoid colon: report of a rare case and its possible association with nonsteroidal anti-inflammatory drugs. (2002) Am Surg 68(1): 62-64.
- 6. Hollingworth, J., Alexander-Williams, J. Non-steroidal antiinflammatory drugs and stercoral perforation of the colon. (1991) Ann R Coll Surg Engl 73(6): 337-340.
- 7. Huang, W.S., Wang, C.S., Hsieh, C.C., et al. Management of patients with strcoral perforation of the sigmoid colon: report of five cases. (2006) World J Gastroenterol 12(3): 500-503.
- 8. Heffeman, C., Pachter, H.L., Megibow, A.J., et al. Stercoral colitis leading to fatal peritonitis:CT findings. (2005) AJR Am J Roentgenol 184(5): 1189-1193.
- 9. Sharma, M., Agrawal, A. Case report: Stercoral sigmoid colon perforation with fecal peritonitis. (2010) Indian J Radiol Imaging 20(2): 126-128.