Targeting oncogenic receptor, currently the standard of care
Fabio Musumeci , Peter Byrne , Deepti Gupta , Ekta Gupta
Affiliation
- 1The Institute of Oncology, Tehran University of Medical Sciences, Tehran
- 2Sacoor Medical Group, London, United Kingdom
- 3International Centre for genetic Engineering and biotechnology, Aruna Asaf Ali Marg, New Delhi, India
- 4Institute of liver and biliary sciences, sector D1 vasant kunj, New Delhi, India
Corresponding Author
Prof. George Zhu, The Institute of Oncology, Tehran University of Medical Sciences, Tehran; E-mail: sansan4240732@163.com
Citation
Zhu, G., et al. Targeting Oncogenic Receptor, Currently the Standard of Care. (2017) Clin Trials Pathol Case Stud 2(2): 75- 90.
Copy rights
© 2017 Zhu, G. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Receptor; Oncogenic receptor; Gene activating mutation; Aberrant rearrangement; Tumours; Cancers
Abstract
In 1989 - 91, George Zhu[1] first postulate oncogenic receptor (Voice of America, 1992, 12:31; Curr Pharm Biotechnol, 2013, 14:859 - 863), as a result of his experiments in which steroid PML-RARa fusion receptor gene rearrangement within t (15;17) translocation in acute promyelocytic leukemia (APL), and androgen cognating its (AR/ERa signaling or FGFR-1) receptor induced tumours of the breast glands in two aplastic anemia during the course of testosterone treatment (hormonal tumorigenesis). In the past 2 - 3 decades, there are at least 30 receptor genes involving in several of oncogenic process. These normal physiologic receptors linked to gene amplification, rearrangement, deletion and activating mutations, which converted receptor to oncogenic (also oncogenic receptor) in development, progressive and pathogenesis of benign and malignant diseases. Receptors included nuclear receptor family members (oncogenic estrogen/estrogen receptor alpha signaling, oncogenic androgen receptor, oncogenic pml/RARa, and GRβ); Oncogenic growth factor receptors (EGF/ oncogenic receptor EGFR, Neu oncogenic receptor, insulin receptor substrate 4 IRS4/insulin receptor/c-ros proto-oncogenic receptor, insulin and IGF-1 and -II/oncogenic IGF-1R, oncogenic PDGFAR, oncogenic TEL/PDGFRB, thrombopoietin (TPO)/TPO receptor, oncogenic MPL receptor, HGF/HGFR, met oncogenic receptor), Cytokine receptor rc family members (IL-2-BCM fusion, IL-3/oncogenic IL-3Ra, IL-7/oncogenic IL-7R and IL-21R-BCL6 fusion); Cytokine receptors including the βc family (G-CSF/oncogenic CSF3R, oncogenic EPOR), and oncogenic autocrine growth hormone/nuclear GHR and other VEGFR2. Upon ligand binding or external antigen stimuli, mutated growth factor receptors and mutant cytokine receptors including type I cytokine receptor may be activated via ligand binding receptor complex, receptor dimerizes especially receptor homodimerization, and induces transphosphorylation of tyrosine residues in the cytoplasmic domains which serves as docking sites for several adaptor molecular harboring SH2 domain or phosphotyrosine binding domain. These adaptor molecules recruit and activate downstream signaling molecules such as Ras/MAPK, phospholipase C-r, JAK-STAT molecules, NF-KB pathways through tyrosine- or serine/threnonine-phosphorylation. Among them, Ras /MAPK/ERK, PI3-K/akt and STAT pathways act as the major oncogenic signaling pathway. Overall, these receptors coupled with their ligands are key importance in human subtle balance in physiologically regulating multiple cellular processes, for example, in cellular proliferation and differentiation. Oncogenic receptors mutational activation and/or aberrant gene rearrangement are promiscuously interference with normal cell survival, anti-apoptosis and proliferation, and malignant initiation and progression. Others, in a special APL case, oncogenic pml/RARa fusion behave as a potent (constitutive) transcriptional repressor of RAR and retinoic acid signaling, inducing a differentiation blockage at promyelocytic stage which can be overcome with therapeutic doses of 9-cis retinoic acid or ATRA ligand (see in detail model, George Zhu, January 1991. Curr Pharm Biotechnol, 2013, 14: 849-858)[2,6,8]. This is the classical model of retinoic acid action. This encourages receptor normal agonist, and oncogenic receptor antagonists (or inhibitors) target therapy.
Introduction
Since introduction of oncogenic receptor concept by George Zhu from oncogenic pml/RARa fusion in etiology of a specific APL and androgen/androgen receptor oncogenic signaling in role of hormonal tumorigenesis in early 1989s[1-13], de The H and Chomienne C[14,15], at the same peroid, found that in t (15;17) APL the translocated retinoic acid receptor alpha (an RAR mutant) contribute to leukemogenesis. Neil JC[14-16] is in detail receptor-mediated leukaemogenesis from the oncogenic function of T cell antigen receptor (TCR oncogenic signal) on lymphoid cells not only bind external ligand but are crucial in cellular proliferation. In transgenic mice expressing a mutated TCRbeta lacking the variable chain (Detta V-TCRbeta) developed CD4+, CD8+, IL-2Ra positive T-cell lymphoma[17,18]. Patients with ataxia-telanglectasia are particularly prone to development of T-cell chronic lymphocytic leukemia with chromosomal abnormalities. The breakpoint is composed of a TCR J alpha chain region (from 14q11) fused to sequences derived from 14q32 but on the centromeric side of the IgCmu (IgH), indicating that a 14:14 translocation [t (14; 14) (q11; q32); inv (14) (q11; q32)] in the development of T-cell tumors[19,20]. Like mutated oncogenic growth factor receptors[21,22], antigen- independent B cell receptor (BCR) signaling drives the oncogenic process (Farinha, 2005). The genetic defects in heavy-chain disease (HCD) result in the production of abnormal membrane-associated heavy chain lacking an antigen-binding domain, these aberrant B-cell antigen receptors might engage in ligand-independent signaling, indicating a role in the genesis of HCD neoplasia[21-23]. Thus, BCR associated kinase inhibitors, such as ibrutinib, have revolutioned the treatment of chronic lymphocytic leukemia (CLL).
Yarden Y (1991)[24] propose neu oncogenic receptor from neu oncogene-related receptor tyrosine kinase (RTK), and this might be useful in neu oncogenic receptor[24-29] antagonists lapatinib and trastuzumab target therapy in metastatic breast cancer with HER2V659E mutation[30]. In a large trials of 48 HER2-positive early breast cancer patients, the adjuvant trastuzumab treatment demonstrates highly favorable outcome. Five-year overall survival rates and disease free survival rates were 95.8% and 93.8% respectively (Kato, 2015). Al-Nedawi[31] explore the area that microvesicles containing oncogenic receptor EGFRVIII released to cellular surroundings and blood of tumour-bearing mice,and can merge with the plasma membranes of cancer cells lacking EGFRVIII. This intercellular transfer of membrane-derived microvesicles (‘oncosomes’ -small plasma membrane buds, Robinson, 2008[32]) leads to the transfer of oncogenic activity including activation of MAPK and Akt and autocrine activation of its key signaling receptor (VEGF receptor-2), and increases in anchorage-independent growth capacity. Santos[33] studies oncogenic GRPR (gastrin-releasing peptide receptor) in neoplastic multiple signaling pathway. Somatic mutations in cholecystokinin 2 receptor (CCK2R) alter receptor activity that promote oncogenic phenotype, and the importance of evaluating CCK2R inhibitors to block mutant forms of this receptor[34]. Intriguing, epithelial cell adhesion molecule (EpCAM), as a homophilic adhesion protein,is a novel oncogenic receptor which frequently overexpressed in epithelia, progenitors, embryonic stem cells, carcinoma and cancer-initiating cells, and target its antibodies[35]. The present will in brief focus on recent innovative diagnostic and therapeutic strategies forthcoming in this area.
Steroid hormone receptors oncogenic signaling
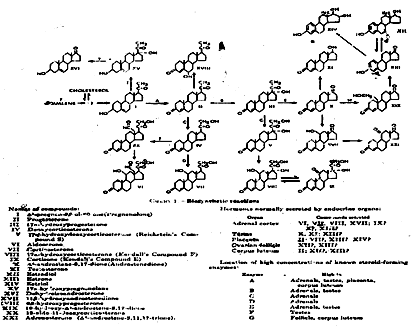
Steroid hormones are a biologically related hormones secreted into blood stream by the adrenal cortex and glands (ovaries and testes) (Singh and Kumar, 2005). After releasing into the blood, steroid hormones enter target cells by crossing the cytoplasmic membrane and exert their action by binding to high affinity receptors, also known as steroid hormone receptors. Steroid hormones control a wide variety of cellular function. Sex hormone (androgen and estrogen) play an important role in gonadal (sex determination) development, the formation of the menstrual cycle. At puberty, estradiol induces mammary duct formation. As the hypothalamic-pituitary-ovarian axis matures, there is a brief phase of anovulatory cycles during which the mammary gland is influenced principally by estrogens. Once ovulation is established, corpus luteum produces progesterone, which stimulate growth of the lobular velour structures. During the reproductive years, progesterone promotes differentiation of alveolar cells into secretory cells, and dilation of the duct system. In conjunction with prolactin and other metabolic hormones, progesterone stimulates lipid droplet formation, and secretory activity. While prolactin and growth hormone are the most important pituitary hormones affecting growth of the mammary gland during pregnancy. It is estradiol and progesterone that prevents the full expression of these secretory effects on the mammary epithelium. At parturition, the sudden withdrawal of these two hormones permits the breast to respond to the lactogenic hormones. Progesterone can acts in synergy with estradiol to prime the mammary gland to respond to mitogens like prolactin, glucocorticoids and growth hormone, which is essential for human alveolar gland development and growth (Horwitz, 1985). The following figure 1 represents hormone biosynthetic reaction.
Figure 1: Hormones normally biosynthetic reaction.
The estrogen receptor (ER) is found in a wide variety of species and is involved in the programming and regulation of gene expression in vertebrate female sex-accessory tissue[36]. Estrogen E2/ERa signaling plays an important role in the regulation of mammary gland development and function, and also contributes to the onset and progression of breast cancer. More than 70% of human breast cancers express ERa, and elevated levels of ERa in benign breast epithelium correlate with increased risk of breast cancer[37]. Green S & Chambon P(1986)[38] described oncogenic hormone receptor from human oestrogen receptor cDNA sequence. This carcinogenicity of estrogen is attribute to receptor-mediated stimulation of cellular proliferation. Increased proliferation could result in turn in accumulation of genetic damage and stimulation of the synthesis of growth factors that act on the mammary epithelial cells via an autocrine or paracrine loop[39]. There were evidence that estrogen-dependent cell line(MCF-7) cells under estradiol(E2) stimulation release some known polypeptide growth factor activities (EGF-like, IGF-1-like)[40]. Dickson RB and Stancel GM (2000)[41] discuss estrogen receptor-mediated processes in normal and cancer cells. ER-mediated regulation of gene expression plays many significant roles in normal and cancer cells and this will improve the understanding of hormonal carcinogenesis.
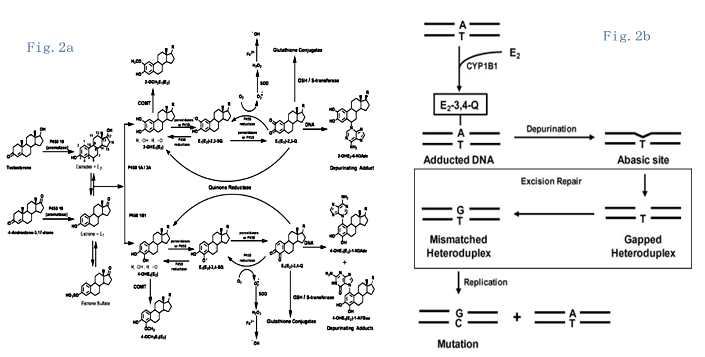
Furthermore, Russo (2009)[42], Santen, Cavalieri, Rogan (2009)[43] and Yager, Yue (2013)[44-46] discussed estrogen receptor-dependent and independent mechanisms of breast carcinogenesis. ERa mediated stimulation of breast cell proliferation with a concomitant enhanced rate of mutations, and estradiol metabolites (see figure 2a) to genotoxic DNA mutation cause DNA damage (figure 2b). Thus, ERa function as estrogen activated transcription factor and involved in the stimulation of estrogen target genes in the regulation of cell cycle progression and growth of breast epithelium[47]. As Clarke described[48], some ERa/PR-positive epithelial cells are quiescent breast stem cells that acts as ‘steroid hormone sensors’. Such hormone sensor cells are likely to secrete positive or negative paracrine/ juxtacrine factors dependent on the prevailing estrogen or progesterone concentration to influence the proliferative activity of adjacent ERa/PR-epithelial cells. This might represent one step toward the development of neoplasia and malignancy-invasive tumors.
Figure 2: a. Estradiol metabolites reaction. b). Schematic description of DNA damage mutation following formation of depurinating adduct. (Data adapted from Yue & Yager, etal, Steroid, 2013,78:161-70[35]).
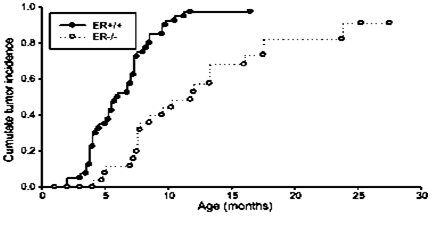
Utilizing ERKO/wnt-1 oncogene mice[49]. (figure 3) and aromatase/ERKO transgene mice[50], they demonstrated the role of ERa-dependent in mammary development and carcinogenesis. Lack of ERa mice results in impaired mammary development and much delayed tumor incidence even in the presence of tissue estrogen (50% of mammary tumors at 5 months in ER-positive animals versus 11 months in those without ERa). Whereas introduction ERa into the tTA/TAg mice[51] and DES-treated MT-mER transgene mice[52,53] developed mammary adenocarcinoma (at 8 months) and preneoplastic lesion atypical hyperplasia (at 4 months), which implicate that ERa contributes to carcinogenic through ER-mediated signal transduction, increasing estrogen-responsive cell proliferation, and ERa signaling in mammary cancer initiation and progression.
Figure 3: The effect of estrogen receptor alpha (ERa) on the development of mammary tumors in Wint-1 transgenic mice.(Data adapted from Bocchinfuso, J Mamm Gland Biol Neoplasia, 1997, 2:323-34[49]).
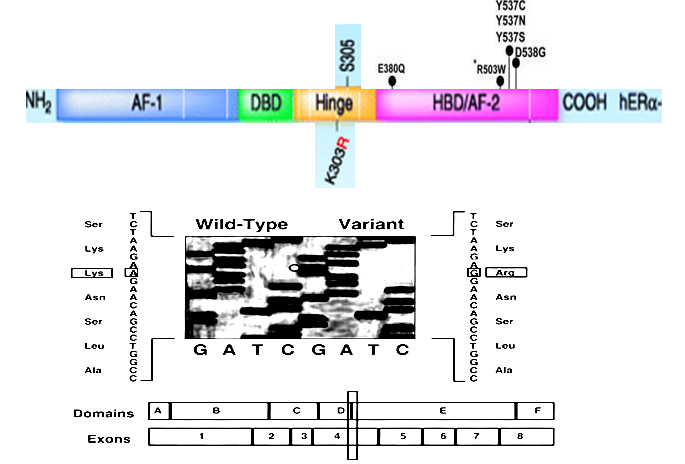
Moreover, mutations in estrogen receptor converted estrogen receptor-dependent breast tumor into estrogen-independent growth[54]. Fuqua (2000)[55] found a K303R estrogen receptor alpha (ERa) mutation in human premalignant breast lesions (see figure 4). The K303R mutation formed tumors in nude mice faster than cells expressing wild-type ERa in the presence of low levels of estrogen (at 10 - 12 M estradiol), and those K303R ERa-expressing tumors are estrogen-independent growth[56]. From screeing of those ER+ breast cancer, Veeraraghavaa and colleagues[57,58] detected oncogenic ESR1- CCDC170 fusion positive tumors. This neoplastic ESR1-CCDC170 fusion leads to anchorage- independent growth, reduced endocrine sensitivity and enhanced xenograft tumor formation, suggesting a new concept of this oncogenic receptor ESR1 fusion in path biology in a more aggressive subtype of breast cancer.
Figure 4: Sequence analysis of ER Var and WT cDNAs isolated from frozen breast hyperplastic tissue. A portion of the sequencing products is shown for WT and Var clones, demarcating the location of the G transition and Arg substitution. ER domains A–E and the exons across these domains are shown on the bottom, with the location of the Lys-to-Arg change demarcated with a box across exon 4 at the end of domain D (Data adapted from Fuqua, etal, Cancer Res, 2000, 60:4026-9[55]).
Thus far, in addition to tamoxifen and fulvestrant, AZD9496, a non-steroid small molecule inhibitor of oncogenic (or neoplastic, due to not targeting a normal ERa) ERa[2-6,38,51,52,59], bound and down- regulated clinically relevant ESR1 mutants in vitro and inhibited tumor growth in an ESR1 mutant patient-derived xenograft model that included a Y537 and D538G mutation[60,61]. AZD9496 is currently being evaluated in a phase I clinical trial[62].
Using heterotypic tissue recombination,Cunha (1981- 2008)[63] established a stromal androgen receptor for mesenchymal-epithelial transition(EMT) in normal androgen-dependent prostate development and in the etiology of benign prostatic hyperplasia[64]. By different methods including immortalized human prostate cells expressing androgen receptor[64] and androgen receptor transgene[65], they demonstrated that androgen receptor is oncogenic, and this oncogenic receptor induces prostate intraepithelial neoplasia (PIN) and plays a cruical role in transforming process in prostate cells. The AR-expressing PrECs are dependent on circulating testosterone for tumor growth, and immortalized PrECs lacking AR failed to form tumors. But this androgen receptor is difficult to characterize as an oncogene[64]. Mononen (2000)[66] and Koivisto (2004)[67] detected the R726L mutation of androgen receptor (AR) in Finnish patients with sporadic or familial prostate cancer, which may confer an up to 6-fold increased risk of a small fraction of prostate cancer in Finlan. T877A mutation of AR was idenitified in LNCaP cell line and metastatic cells of androgen -independent prostate cancer[68-74], whereas V739M was identified in early stage PCa[75]. Nyquist (2013)[76] discovered intragenic AR gene rearrangements in CRPC tissues, rendering expression of truncated AR variants proteins lacking the AR ligand-binding domain, constitutive activity of AR, and intragenic ARv567es cDNA formed tumor faster rate and a CRPC growth independent of full-length AR or androgens. Therefore, targeting oncogenic AR variants[7,64,77-82] (here, please note that it is no need to target a normal AR) includes AR antagonists bicalutamide and enzalutamide, which might provide an approach to suppress prostatic intraepithelial neoplasia (PIN) development. In phase II trials, the CBR (clinical benefit rate) of 19% was observed with bicalutamide 150 mg daily dose in selected patients with androgen receptor-positive, estrogen receptor-negative metastatic breast cancer[83].
In another area,increased thyroid diseases and thyroid papillary carcinoma(PTC) associated with a high dietary iodine intake[7,84-93].
GRβ/STAT-5 pathway was found to be involved in erythrocytosis[94], and GR/SGK1(including GR-SGK1-FOXO3a signaling pathway and GR-SGK1-MKP1/DUSP1 pathway) network linked to higher tumor grade and antiapoptotic and increased cancer recurrence[95-97]. Moreover,the aberrant glucocorticoid receptor signaling in breast cancer[98-101], prostate hyperproliferation[97,102,103], Cushing’s disease[104] and Nelson’s syndrome[105]. Thus, GR activation is sufficient to provide a potent signal for cell survival in mammary epithelial cells. Induction of serum and glucocorticoid-regulated kinase-1 (SGK-1) expression is required for GR-mediated epithelial cell survival signaling. SGK-1 is a direct GR target and encodes a serine-threonine kinase with significant homology to Akt-1. In immunohistochemical analysis, nucleus GR-immunostaining and glucocorticoid receptor(GR)- immunopositive cells were abundantly present in subclinical Cushing’s disease due to pituitary adenomas (2 macroadenomas and 8 microadenomas), suggesting impaired glucocorticoid action, at least in part, in tumorigenesis of this disease[104]. RU486 (mifepristone), a glucocorticoid receptor antagonist, has been successful treatment of the Cushingoid phenotype with markedly elevated lymphocyte glucocorticoid receptor numbers in a transient Cushing’s syndrome[106]. Mifepristone may also be a useful strategy for increasing tumor cell apoptosis in chemotherapy-resistant GR+ triple- negative breast cancer (TNBC)[108]. In addition, the cortisol/cortisone-responsive AR(AR (ccr)) has two mutations (L701H and T877A) that were detected in the MDA PCa human prostate cancer cell lines estabolished from a castrated patient whose metastatic tumor exhibited androgen-independent growth. GR antagonist RU38486 showed inhibitory activity[102], but its therapeutic application to treat prostate cancer may be limited. Thus, the combination of ARccr receptor antagonists bicalutamide (casodex) together with a ligand suppressor (triamcinolone) represents a new therapeutic strategy for the treatment of the subset of androgen-independent prostate cancers harboring the L701H or ARccr type.
So fathered is a conflict among hormone FSH/FSH receptor in etiology of epithelial ovarian cancer[109,110]. Actions of FSH (follicle-stimulating hormone) in reproductive physiology are essential for folliculogenesis and steroidogenesis[111], FSH receptor (FSHR), a transmembrane receptor with a G protein-coupled signaling, is expressed by granulosa cells in developing ovarian follicles. Over expression of FSHR activates oncogenic pathways through FSHR-induced EGFR amplification, and HER-2/ neu and activated ERK1/2 in preneoplastic immortalized ovarian surface epithelial (IOSE) cells[112]. The data by epidemiological studies that an increased occurrence of ovarian cancer has been suggested with exposure to high levels of gonadotropins during post menopause or infertility therapy[113-115].
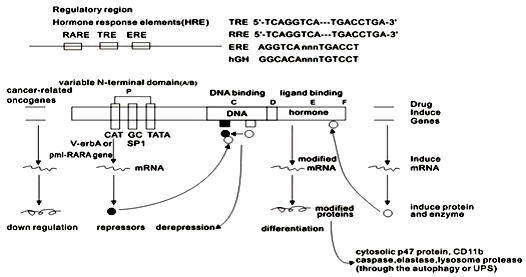
Retinoid can regulate proliferation and differentiation of normal myeloid cells, and that supraphysiological levels of retinoic acid (9-cis RA or all-trans RA) can induce abnormal promyelocytes toward maturation. These leukemic cells harboring steroid PML-RARA translocation play a central role in etiology of APL[8,12,13,116]. The PML-RARa chimera can function as a strong transcriptional repressor of retinoic acid (RA) signaling and RAR function by perturbing normal retinoid signaling, leading to a block in differentiation and in an accumulation of leukemic cells at promyelocytic stage[8,10,116-129] (see model, figure 5, George Zhu, 1991, 2013 - 2014). This oncogenic receptor is locked in its “off” regulated mode thereby constitutively repressing transcription of genes or key enzymes that are critical for differentiation of hematopoietic cells[8,130]. Moreover, the PML-RARa apparently involved in part the defects in ability to release corepressor under physiological hormone concentration, the wild-type RARa readily form heterodimer with the retinoid X receptors (RXRs). In contrast, chimeric pml/RARa oncoprotein exhibited an enhanced ability to bind to DNA as homodimer. This enhanced homodimerization by RAR chimeras implicates in aberrant co repressor interaction properties of these oncogenic receptor derivatives, influences their DNA recognization, and appears to prevail in neoplastic cells of these oncoproteins[130]. These differences in target gene recognition by the normal and oncogenic RARa protein may contribute to the leukemogenic phenotype[130].
Figure 5: Hypothetical model of the regulation of retinoic acid (RA) action (George Zhu, January 1991, revised in 2012). Schematic alignament of the receptor protein. The two highly conserved regions, identified as the putative DNA- binding (C) and hormone -binding (E), ahinge region (D) and the non- conserved variable NH2-terminus (A/B) as described above. (Data adapted from George Zhu, January 1991. Curr Pharm Biotechnol, 2013, 14:849-858[4,5]).
Targeting oncogenic growth factor receptors
The EGF receptor (EGFR)[130] has a key role in normal embryonic development, adult tissue hemeostasis and many pathological processes, particular tumor formation. Aberrant EGFR activation becomes oncogenic due to over expression and/or amplification of the EGFR gene or by autocrine / paracrine growth factor loops, whereas activating dimerized mutations promote EGFR signaling, which lead to ligand-independent[130-133]. Phosphorylation of this oncogenic receptor at residues Tyr845, Tyr1045 and Tyr1173 leads to receptor activation and downstream signaling[135,136]. Oncogenic receptor EGFR[2-6,9,11,134,137-139] was found to involved in A431 human carcinoma cells[140-143], squamous cell carcinoma (SSC)[144], epithelial cell lines from mammary carcinoma[145], glioblastoma stem cells[9,146,147], EGFR+++ positive in one glioma, George Zhu, 2013], and colorectal carcinoma tissue[148]. Oncogenic EGFR mutations are found in 10% to 35% of lung adenocarcinomas, with predominant in a subset of patients with non-small cell lung cancer (NSCLC)[149-151]. These mutations, which commonly occur as either small in-frame deletions in exon19 or point mutations T790M and L858R in exon21 within the EGFR tyrosine kinase domain, confer constitutive activity and sensitivity to EGFR tyrosine kinase inhibitors(TKI)[152,153]. Recent, Gallant[152] identified a novel EGFR alterations in lung cancer: EGFR exon 18-25 kinase domain duplication (EGFR-KDD). EGFR-KDD is oncogenic and oncogenic EGFR-KDD-transformed cells are sensitive to the EGFR TKI afatinib. Konduri and colleagues[153] reported five patients with metastatic lung cancer whose tumors harbored EGFR fusion, most commonly RAD51, are recurrent in lung cancer. Four of whom were treated with EGFR TKI erlotinib with documented antitumor response for 5, 6, 8, and 20 months respectively. These patients whose tumors harbored EGFR fusions are oncogenic in preclinical studies. In mouse model, transgenic mice expressing EGFR L858R in type II pneumocytes developed atypical adenomatous hyperplasia and multifocal adenocarcinoma, and gefitinib inhibited tumorigenesis completely[154]. Blesa[155] present a durable complete remission of a relapsed glioblastoma with a complete radiologic response and the combination of cetuximab and bevacizumab in a third-line setting, that has offered a progression-free survival of 20 months. In Cuba, CimaVax-EGF, promising, an active vaccine targeting EGF as the major ligand of EGFR, it is in use as a cancer therapy against non-small-cell lung cancer (NSCLC)[156,157].
PDGFRa mutations are oncogenic (tumorigenic) and developed 100% of mice with brain tumors whereas only one of 19 mice implanted with cells over expressing wild-type PDGFRa developed into brain tumor in vivo[158,159]. This D842V mutant was effectively inhibited by crenolanib, a specific inhibitor of PDGFRa and PDGFRß. Golub (1994)[160] identified that PDGF receptor β is oncogenic in pathogenesis of chronic myelomonocytic leukemia with t (5;12) chromosomal translocation, targetable oncogenic receptor tyrosine kinases PDGFRa/PDGFRβ, and FGFR fusions[145-147] in diverse cancers have made some major progress. For example, these hypereosinophilia (HES) patients with FIP1L1/PDGFRA have excellent responses to imatinib treatment[167-172]. At present, Imatinib, a selective inhibitor of ABL, KIT,and PDGFRA/B, is the first line target therapy for gastrointestinal stromal tumor (GIST)[173].
Hepatocyte growth factor (HGF), like other growth factors, has different effect in different cells. HGF regulates cell growth, cell mortality and morphogenesis by acting a tyrosine signaling cascade after binding to the proto-oncogenic receptor for HGF (HGFR, also proto-oncogenic receptor c-met, met receptor)[174-177]. HGF enhances hepatocyte growth, potently suppresses apoptic death of hepatocytes and decreases serum bilirubin and serum ALT (alanine aminotransferase), which provide therapeutic action of HGF, including severe hepatitis, falminant hepatic failure[178] and liver cirrhosis[179].
HGF-HGF receptor (met oncogenic receptor) signaling stimulate growth of mouse C127 cells transformed phenotype[ 180], Caki-1 (a human kidney clear cell carcinoma cell line), U87-MG (a glioblastoma cell line)[181], canine osteosarcoma cells[176], and human hepatoblastoma cells[181], and AML[182].
In vitro HGF can transform immortalized mouse liver epithelial cells[183]. Serum HGF levels are elevated in patients suffering from chronic hepatitis and liver cirrhosis (Tomiya, 1992). Moreover, hepatocytes from transgenic mice expressing HGF grew more rapidly than did those from normal siblings. In vivo, Fao HGF cells produced tumors when transplanted into nude mice[184]. These conditions cause persistent hepatocellular damage and regeneration; consequently, there are associated with the subsequent of hepatocellular carcinoma (HCC). Thus, HGFHGF receptor signaling might play an important role in carcinogenesis[182,185]. PRS-110 (starting at 0.8 mg/kg and going up to 30 mg/kg) specifically binds to Met receptor with high affinity and blocks HGF interaction on ligand-dependent (U87-MG) and ligand-independent (Caki-1) xenograft model[181]. Animals were randomized for the treatment with a novel met inhibitor EMD1214063 (50 mg/kg/d), which resulted in a complete regression of the sensitive H1112L met variant-derived tumors[186]. Foretinib, the first multi-target c-met TKI to under clinical investigation, produced a promising benifit in HCC patients[163]. Recently, the chemically-modified monovalent antibody DN30 was found to inhibit ligand- independent activation of the met oncogenic receptor, providing an another target therapy[187-189].
Cytokine receptors had oncogenic mutant variants in cancer
Growth hormone (GH)/oncogenic GH receptor (GHR)[190-193] was associated with growth hormone receptor deficiency[194]; gigantism, acromegaly and cancer risk[195-199]; GHR determines ‘cancer- like’ features[193]. And GH-releasing hormone GHRH/GHRH receptor oncogenic signaling[201,202]. Insulin/insulin receptor/Ros proto-oncogenic receptor homologue, and IGF-I, IGF-II/ oncogenic receptor PTK IGF-IR linked to physiology and diseases (short status, oncogenic transformation process)[202-209]; and IGF-I (Mecasermin) replacement therapy[212-214]. Interesting, the oncogenic mechanism in Ewing sarcoma harboring oncogenic EWS/NR4A3 fusion involves a novel pro- oncogenic IGF/IGF-1 receptor signaling pathway including post-transcriptional derepression of IGF signaling by the EWS/Fli1 fusion oncoprotein via miRs[215], and this provide therapeutic targeting anti-IGF-1 receptor antibody in Ewing Sarcoma[216-218]. G-CSF (filgrastim) has been used in clinic for more than 2 decades to treat congenital and acquired neutropenias[219-224]. It is highlight the clinical application of G-CSF to children with severe congenital neutropenia (SCN) and especially in patients with neutropenia harboring in the G-CSF receptor (CSF3R) gene, which is correlated to an increased risk for development of MDS and acute myeloid leukemia(AML)[225]. There are two classes of CSF3R mutant variants:truncations of the cytoplasmic domain[226,227] and membrane proximal point mutations including T618I[228]. Truncated CSF3R mutations are the mutant type nearly almost observed in SCN and abnormal signaling of this oncogenic receptor variants in malignant transformation, whereas membrane proximal mutations (particularly T618I) are the predominant mutation type observed in chronic neutrophilic leukemia (CNL) and atypical (BCR-ABL negative) chronic myeloid leukemia (aCML), and confer ligand-independent growth[228]. Maxson and colleagues[229] identified activating mutations for CSF3R in 59% (16/27) of patients with CNL or atypical CML. In vivo, the activating mutation in the CSF3R gene induces hereditary chronic neutrophilia[230]. Mice transplanted with CSF3R T618I-expressing hematopoietic cells developed a myeloproliferative disorder[228]. Treatment with the JAK inhibitor ruxolitinib lowered the white blood cells and reduced spleen weight. These results indicate that activating mutant CSF3R is oncogenic[229] and sufficient to drive a myeloproliferative disorder resembling CML and CNL that is sensitive to pharmacologic JAK inhibition[228].
Another more example is that a translocation t (14; 19) (q32; P13) was involved IGH@ and the cytokine receptor EPOR at 19P13 in two patients with B-cell precursor acute lymphoblastic leukemia (BCP-ALL)[231-233]. An over 230- and 241-fold increase in the expression of EPOR were observed in 2 patients at diagnostic and relapse samples respectively. The EPOR-IGH/IGK chain fusions result in truncation of the cytoplasmic tail of EPOR at residues similar to the mutant EPOR in PFCP, with preservation of the proximal tyrosine essential for receptor activation and loss of distal regulatory residues. Expression of truncated EPOR in mouse B cell progenitors induced ALL in vivo. The data implicate oncogenic erythropoietin receptor in role of both benign erythrocytosis and malignancy[234,235]. Moreover, mutation of erythropoietin receptor(EPOR) gene was associated with primary familial and congenital polycythemia (PFCP). Truncated mutations of 59 to 84 amino acids of EPOR at c-terminus lead to loss of the intracellular cytoplasm tail of the receptor, and prolonged proliferative signal resulting in hypersensitivity (5-10 fold increased sensitivity) to erythropoietin, and prolonged activity of JAK2 kinase and STAT5 activity[236-239]. The leukemic cells with oncogenic EPOR fusions were sensitive to JAK-STAT inhibition, suggesting a therapeutic option in high-risk ALL.
Accumulated studies, constitutive activation of cytokine interleukin-2 (IL-2) gene can induce autocrine growth of IL-2-producing leukemic cells in adult T-cell leukemia[240], in vitro transformation and tumorigenicy of T cells[241-244], and tumour cells bearing IL-2-BCM fusion in a T cell lymphoma with t(4;16)(q26;p13) translocation[245]. IL-2 binds to IL-2 receptor a (IL-2Ra) and rc subunit of the IL-2 receptor (IL-2RG) sharing with other cytokine receptor super family (including IL-7 receptor, IL-21 receptor) that receptor complex transduces growth and differentiation signals[246]. Under physiological condition, IL-2 appears to act on antigen-specific proliferation of T lymphocytes, immune thymocytes, B-lymphocytes, natural killer cells (NK cells) and lymphokine-activated killer cells (LAK cells), which linked to adoptive immune therapy[247].
In vitro nude mice, fibroblasts transfected with a chimera molecule containing the extracellular IL-2 binding domain of the IL-2R cDNA and the transmembrane and intracellular kinase domain of the EGF receptor cDNA, were morphologically transfomed and produced rapidly growing tumor[248]. Moreover, retroviral expression of IL-2RG restore signaling by IL-7 receptor to X-SCID precursor cells in T-cell progression to the pro-leukemic effects of ectopic LMO2[249]. Recently, the chromosomal translocation t (5;9) (q13; q22) in peripheral T cell lymphoma generating the interleukin 2 inducible T cell kinase (ITK)-spleen tyrosine kinase (SYK) fusion kinase mimics a T-cell receptor signal and drives oncogenesis in mouse models (Pechloff, 2010).
Activation of the interleukin-3 (IL-3) gene by the enhancer of the IgH fusion leads to the overexpression of IL-3 gene product in 2 cases of acute lymphocytic leukemia with t (5; 14) (q31; q21) translocation[250]. Serum IL-3 correlated with the clinical course.When the patient’s leukemic cell burden was highes t (WBC 116,500/ul, lymphoblasts 33,785/ul), the serum IL-3 level was highest (799,5 pg/ml); whereas complete remission (WBC 123,00/ul, lymphoblasts 0/ul), serum IL-3 levels decreased to 105,1 pg/ml. Therefore, overexpression of IL-3 gene coupled with the presence of aberrant IL-3 receptor in these cells could account for oncogenic effects of proliferatative advantage and may play a central role in the pathogenesis of leukemia[250,251]. Aberrant presence of cystiene residues was shown to induce homodimerization of mutant interleukin-7 receptor (IL-7R), which drive constitutive signaling via JAK1 and independently of IL-7, rc or JAK3[252], promoting cell transformation. This abnormality is involved in -10% human pediatric T-cell leukemogenesis, paving the way for therapeutic targeting oncogenic IL-7R-mediated signaling in T-ALL[253-255]. Interleukin-21 receptor (IL-21R) is capable of signal transduction through homodimerization or potentially heterodimerization with IL-2R gamma. IL-21 and IL-21R not only regulates proliferation of mature B cells and T cells in response to activating stimuli but also mediate expansion of NK population from bone marrow. The gene for IL-21R is found the partner of BCL6 in t (3; 16) (q27; p11), which is recurrently observed in diffuse large B-cell lymphoma and a lymphoma cell line YM[256]. This IL-21R/BCL6 fusion gene is clearly associated with lymphoid cell origin.
Conclusion
To date, antibodies that target oncogenic receptors are often targeted toward lysosome[257] or blockade of translocation from the endoplasmatic reticulum to the cell surface of specific antigens such as vascular endothelial growth factor receptors (VEGFR2) or Tie2[258]. For instance, targeting cells with biotinylated ligands and addition of streptavidin efficiently targets trastuzumab to lysosome and this crosslinking of trastuzumab increased lysosomal degradation of its cognate oncogenic receptor Her2 in breast cancer cell lines[257]. Another burgeoning class of targeted chemotherapies called antibody-drug conjugates (ADCs). This ADCs that have demonstrated sufficient efficacy to gain and retain clinical approved are ado-trastuzumab emtansine (brand name Kadcyla) and brentuximab vedotin (brand name Adcetris)[259]. The auristatin-based antibody-drug conjugate BAY1187982 is for the treatment of FGFR2-positive solid tumors[195]. Another, the nicotinic acetylcholine receptor a7-nAchR (toxicology) is the oncogenic receptor, which mediated nicotine (NNK and NNN) oncogenic signaling in an important role in the initiation and progression of cancer including lung cancer and this oncogenic response was in parallel with the mutagenic and cytotoxic effects of tobacco smoke to promote the growth and angiogenesis of the tobacco related cancers[260]. Thus nAchRs yiel- new targets for the prevention and treatment of tobacco related cancers. Thus, down regulating oncogenic receptors may be useful paradigm and perspective in currently the third-line setting of clinical target therapy and cancer biology (Woodman, 2016; George Zhu, 2014)[261].
Acknowledge:
We wish to thank Prof. T.Taniguchi in University of Tokyo in Japan, Nobel Laureates Prof. Ferid Murad in University of Texas Health Center in USA and UNESCO Science Laureates Prof. Atta-ur-rahman in international centre for chemical and biological sciences, university of karachi in Pakistan for their valuable help. I especially want to thank my friend Mr Xu for his precious time and patience in long preparing the article.
Conflict of interest:
The author(s) declare(s) that there is no conflict of interest regarding the publication of this paper.
References
- 1. Zhu, G. Oncogenic receptor hypothesis(1989-91). (1992) VOA(Voice of America) 12: 31.
Pubmed || Crossref || Others - 2. Zhu, G. A retrospective study of the combination of chemotherapy with phytohemagglutinin (PHA, inducing the generation of interleukin 2) in advanced cancer. (1997) (unpublished data).
Pubmed || Crossref || Others - 3. Long follow up of patients with advanced cancers after chemotherapy with traditional medicine (2000).
Pubmed || Crossref || Others - 4. A further study of patients with advanced cancer after chemotherapy with traditional chinese medicine. (2007) JCCM 2(11): 618-623.
Pubmed || Crossref || Others - 5. Five to ten years survivors of patients with advanced cancers after chemotherapy with traditional chinese medicine. (2009) JCCM 4(9): 512-519.
Pubmed || Crossref || Others - 6. Use of chemotherapy and traditional medicine for advanced cancers: A retrospective study of 68 patients (1993-2010). (2010) JCCM 5(6): 343-350.
Pubmed || Crossref || Others - 7. Zhu, G., Musumeci, F., Byrne, P. Induction of thyroid neoplasm following plant medicine marine algae (sargassum): A rare case and literature. (2013) Curr Pharm Biotechnol 14(9): 859-863.
Pubmed || Crossref || Others - 8. Zhu, G., Mische, S.E., Seigneres, B. Novel treatment of acute promyelocytic leukemia: As2O3, retinoic acid and retinoid pharmacology. (2013) Curr Pharm Biotechnol 14(9): 849-858.
Pubmed || Crossref || Others - 9. Zhu, G., Dong, J.X., Dharmadhikari, D. In, Natural products from traditional medicine antitumor compound in advanced cancers. (2013) Proceeding of BIT's11th Annual Congress of International Drug Discovery Science and Technology: pp477.
Pubmed || Crossref || Others - 10. Zhu, G. Discovery of the molecular basis of retinoic acid action (retinoid signaling)-A genetic regulation of eukaryotes in transcription. (2014) Proceedings of 3rd biotechnology world congress, Duibai, UAE pp97-98.
Pubmed || Crossref || Others - 11. Zhu, G., Ali-Akbar, S.Y. In oncogenic receptor: from molecular physiology to diseases. (2015) Abstract in BIT's 8th Annual World Cancer Congress-2015: pp 494.
Pubmed || Crossref || Others - 12. Chomienne, C., Ballerioi, P., Balitrand, N., et al. The retinoic acid receptor alpha gene is rearranged in retinoic acid-sensitive promyelocuytic leukemias. (1990) Leukemia 4(12): 802-807.
Pubmed || Crossref || Others - 13. de The H, Lavau, C., Marchio, A., et al. The PML-RARA fusion mRNA generated by the t(15;17) translocation in acute promyelocytic leukemia encodes a functionally altered RAR. (1991) Cell 66(4): 675-684.
Pubmed || Crossref || Others - 14. Neil, J.C., Fulton, R., McFarlane, R., et al. Receptor-mediated leukemogenesis: hypothesis revisited. (1988) Br J Cancer Suppl 9: 76–79.
Pubmed || Crossref || Others - 15. Strzadala, L., Miazek, A., Matuszyk, J., et al. Role of thymic selection in the development of thymic lymphomas in TCR transgenic mice. (1996) Int Immunol 9: 127-138.
Pubmed || Crossref || Others - 16. Mehlen, P., Bredesen, D.E. The dependence receptor hypothesis. (2004) Apoptosis 9(1): 37-49.
Pubmed || Crossref || Others - 17. Jacobs, H., Ossendorp, F., de Vries, E., et al. Oncogenic potential of a pre-T cell receptor lacking the TCR beta variable domain. (1996) Oncogene 12(10): 2089-2099.
Pubmed || Crossref || Others - 18. Cui, Y.Z., Onozawa, M., Garber, H.R., et al. Thymic expression of a T-cell receptor targeting a tumor-associated antigen coexpressed in thymus induces T-ALL. (2015) Blood 125(19): 2958-2967.
Pubmed || Crossref || Others - 19. Denny, C.T., et al. A chromosomal 14 inversion in a T-cell lymphoma is caused by site-specific recombination between Ig and T-cell receptor loci. (1986) Nature 320(6062): 549-551.
Pubmed || Crossref || Others - 20. Davey, M.P. Juxtaposition of the T-cell receptor alpha-chain locus (14q11) and a region (14q32) of potential importance in leukemogenesis by a 14:14 translocation in a patient with T-cell chronic lymphocytic leukemia and ataxia-telangiectasia. (1988) Proc Natl Acad Sci USA 85(23): 9287-9291.
Pubmed || Crossref || Others - 21. Corcos, D. Oncogenic potential of the B-cell antigen receptor and its relevance to heavy chain disease and other B-cell neoplasias: a new model. (1990) Res Immunol 141(6): 543-553.
Pubmed || Crossref || Others - 22. Corcos, D., Osborn, M.J., Matheson, L.S. B-cell receptors and heavy chain diseases: guilt by association? (2011) Blood 117(26): 6991-6998.
Pubmed || Crossref || Others - 23. Friedman, D.R., Weinberg, J.B. Inhibition of B-cell receptor signaling as a therapeutic strategy for treatment of CLL. (2013) The Haematologist 10(3)
Pubmed || Crossref || Others - 24. Yarden, Y., Peles, E. Biochemical analyses of the ligand for the neu oncogenic receptor. (1991) Biochemistry 30(14): 3543-3550.
Pubmed || Crossref || Others - 25. Levea, C.M., Myers, J.N., Dougall, W.C. A structural and kinetic comparison of proto-oncogenic and oncogenic neu receptors expressed in insect cells. (1993) Receptor 3(4): 293-309.
Pubmed || Crossref || Others - 26. Tzahar, E., Yarden, Y. The ErbB-2/HER2 oncogenic receptor of adenocarcinomas:from orphanhood to multiple stromal ligands. (1998) Biochim Biophys Acta 1377(1): M25-37.
Pubmed || Crossref || Others - 27. Houliston, R.S., Hodges, R.S., Sharom, F.J., et al. Characterization of the proto-oncogenic and muant form of the transmembrane region of Neu in micelles. (2004) J Biol Chem 279(23): 24073-24080.
Pubmed || Crossref || Others - 28. Jonckhere, N., Skrypek, N., Merlin, J., et al. The Mucin MUC4 and its membrane partner ErbB2 regulate biological properties of human CAPAN-2 pancreatic cancer cells via different signaling pathways. (2012) PLos One 7(2): e32232.
Pubmed || Crossref || Others - 29. Nicolas, S., Vasseur, R., Vincent, A., et al. The oncogenic receptor ErbB2 modulates gemcitabine and irinotecin/SN-38 chemoresistance of human pancreatic cancer cells via hCNT1 transporter and multidrug resistance associated protein MRP-2. (2015) Oncotarget 6(13): 10853-10861.
Pubmed || Crossref || Others - 30. Serra, V., Vivancos, A., Puente, X.S., et al. Clinical response to a lapatinib-based therapy for a Li-Fraumeni syndrome patient with a novel HER2V659E mutation. (2013) Cancer Discov 3(11): 1238-1244.
Pubmed || Crossref || Others - 31. Al-Nedawi, K., Meehan, B., Micallef, J., et al. Intracellular transfer of the oncogenic receptor EGFRvIII by microvesicles derived from tumor cells. (2008) Nat Cell Biol 10(5): 619-624.
Pubmed || Crossref || Others - 32. Robinson, R. Tumor cells share oncogenic receptors. (2008) J Cell Biol 181(4): 570.
Pubmed || Crossref || Others - 33. Santos, J., Mesquita, D., Barros-Silva, J.D., et al. Uncovering potential downstream targets of oncogenic GRPR overexpression in prostate carcinomas harboring ETS rearrangements. (2015) Oncoscience 2(5): 497-507.
Pubmed || Crossref || Others - 34. Willard, M.D., Lajiness, M.E., Wulur, I.H., et al. Somatic mutations in CCK2R alter receptor activity that promotes oncogenic phenotypes. (2012) Mol Cancer Res 10(6): 739-749.
Pubmed || Crossref || Others - 35. Maetzel, D., Denzel, S., Mack, B., et al. Initial activation of EpCAM cleavage via cell-to-cell contact. (2009) BMC Cancer 9: 402.
Pubmed || Crossref || Others - 36. Green, S., Chambon, P. Carcinogenesis, A superfamily of potentially oncogenic hormone receptors. (1986) Nature 324(6098): 615-617.
Pubmed || Crossref || Others - 37. Elangovan, S., Ramachandran, S., Venkatesan, N., et al. SIRT1 is essential for oncogenic signaling by estrogen/estrogen receptor a in breast cancer. (2011) Cancer Res 71(21): 6654-6664.
Pubmed || Crossref || Others - 38. Russo, I.H., Russo, J. Role of hormones in mammary cancer initiation and progression. (1998) J Mammary Gland Biol Neoplasia 3(1): 49-61.
Pubmed || Crossref || Others - 39. Dickson, R.B., McManaway, M.E., Lipman, M.E. Estrogen-induced factors of breast cancer cells partially replace estrogen to promote tumor growth. (1986) Science 232(4757): 1540-1543.
Pubmed || Crossref || Others - 40. Dickson, R.B., Stancel, G.M. Estrogen receptor-mediated processes in normal and cancer cells. (2000) J Natl Cancer Inst Monogr (27): 135-145.
Pubmed || Crossref || Others - 41. Russo, J., Lareef, M.H., Tahin, Q., et al. 17-Beta-estradiol is carcinogenic in human breast epithelial cells. (2002) J Steroid Biochem Mol Biol 80(2): 149-162.
Pubmed || Crossref || Others - 42. Russo, J., Fernandez, S.V., Russo, P.A., et al.17-Beta-estradiol induces transformation and tumorigenesis in human breast epithelial cells. (2006) FASEBS 20(10): 1622-1634.
Pubmed || Crossref || Others - 43. Abramson, W., Warshawsky, H. Cancer of the breast in the male secondary to estrogenic administration- Report of a case. (1948) J Urol 59(1): 76-79.
Pubmed || Crossref || Others - 44. Santen, R., Cavalieri, E., Rogan, E., et al. Estrogen mediation of breast tumor formation involves estrogen receptor-dependent, as well as independent, genotoxic effects. (2009) Ann NY Acad Sci 1155: 132-140.
Pubmed || Crossref || Others - 45. Yue, W., Yager, J.D., Wang, J.P., et al. Estrogen receptor-dependent and independent mechanisms of breast cancer carcinogenesis. (2013) Steroids 78(2): 161-170.
Pubmed || Crossref || Others - 46. Cavalieri, E.L., Rogan, E.G., Chakravarti, D. Initiation of cancer and other diseases by catechol ortho-quinones: a unifying mechanism. (2002) Cell Med Life Sci 59(4): 665-681.
Pubmed || Crossref || Others - 47. Singh, R.R., Kumar, R. Steroid hormone receptor signaling in tumorigenesis. (2005) J Cell Biochem 96(3): 490-505.
Pubmed || Crossref || Others - 48. Clarke, R.B. Human breast cell proliferation and its relationship to steroid receptor expression. (2004) Climateric 7(2): 129-137.
Pubmed || Crossref || Others - 49. Bocchinofuso, W.P., Korach, K.S. Mammary gland development and tumorigenesis in estrogen receptor knockout mice. (1997) J Mamm Gland Biol Neoplasia 2(4): 323-334.
Pubmed || Crossref || Others - 50. Tekmal, R.R., Liu, Y.G., Nair, H.B., et al. Estrogen receptor alpha is required for mammary development and the induction of mammary hyperplaia and epigenetic alterations in the aromatase transgenic mice. (2005) J Steroid Biochem Mol Biol 95(1-5): 9-15.
Pubmed || Crossref || Others - 51. Tilli, M.T., Frech, M.S., Steed, M.E., et al. Introduction of ER aplha into the tTA/TAg conditional mouse model precipitates the development of estrogen-responsive mammary adenocarcinoma. (2003) Am J Pathol 163(5): 1713-1719.
Pubmed || Crossref || Others - 52. Couse, J.F., Davis, V.L., Hanson, R.B., et al. Accelerated onset of uterine tumors in transgenic mice with aberrant expression of the estrogen receptor after neonatal exposure to DES. (1997) Mol Carcinog 19(4): 236-242.
Pubmed || Crossref || Others - 53. Davis, V.L., Newbold, R.R., Couse, J.F., et al. Expression of a dominant negative estrogen receptor alpha variant in transgenic mice accelerates uterine cancer induced by the potent estrogen diethylstilbestrol. (2012) Reprod Toxicol 34(4): 512-521.
Pubmed || Crossref || Others - 54. Sledge, W.G., McGuire, W.L. Steroid Hormone Receptors in Human Breast Cancer. (1983) Adv Cancer Res 38: 61-75.
Pubmed || Crossref || Others - 55. Fuqua, S.A., Wiltschke, C., Zhang, Q.X., et al. A hypersensitive estrogen receptor-alpha mutation in premalignant breast lesions. (2000) Cancer Res 60(15): 4026-4029.
Pubmed || Crossref || Others - 56. Herynk, M.H., Hopp, T., Cui, Y., et al. A hypersensitive estrogen receptor alpha mutation that alters dynamic protein interactions. (2010) Breast Cancer Res Treat 122(2): 381-393.
Pubmed || Crossref || Others - 57. Veeraraghavan, J., Tan, Y., Cao, X.X., et al. Recurrent ESR-CCDC170 rearrangements in an aggressive subset of oestrogen receptor-positive breast cancers. (2014) Nat Commun 5: 4577.
Pubmed || Crossref || Others - 58. Giltnane, J.M., Balko, J.M., Stricker, T.L., et al. Recurrent ESR1 fusion transcripts are associated with endocrine resistance in estrogen receptor positive,HER2 negative breast cancer. Abstract PD6-3 in Thirty-seventh Annual CTRC-AACR San Antonio Breast Cancer Symposium, December 9-13, 2014, San Antonio, TX. (2015) Cancer Res 75(9S):
Pubmed || Crossref || Others - 59. Frech, M.S., Halama, E.D., Tilli, M.T., et al. Deregulated estrogen receptor alpha expression in mammary epithelial cells of transvenic mice results in the development of ductal carcinoma in situ. (2005) Cancer Res 65(3): 681-685.
Pubmed || Crossref || Others - 60. Takeshita, T., Yamamoto, Y., Yamamoto-Ibusuki, M., et al. Droplet digital polymerase chain reaction assay for screening of ESR1 mutations in 325 breast cancer specimens. (2015) Transl Res 166(6): 540-553.
Pubmed || Crossref || Others - 61. Weir, H.M., Bradbury, R.H., Lawson, M., et al. AZD9496: An oral estrogen receptor inhibitor that blocks the growth of ER-positive and ESR1 mutant breast tumors in preclinical models. (2016) Cancer Res 76(11): 3307-3318.
Pubmed || Crossref || Others - 62. Cunha, G.R., Chung, L.W.K. Stromal-epithelial interactions-I. Induction of prostatic phenotype in urothelium of testicular feminized (Tfm/y) mice. (1981) J Steroid Bio Chem 14(12): 1317 – 1324.
Pubmed || Crossref || Others - 63. Izumi, K., kami, A., Lin, W.J., et al. Androgen receptor roles in the development of benign prostate hyperplasia. (2013) Am J Pathol 182(6): 1942-1949.
Pubmed || Crossref || Others - 64. Berger, R., Febbo, P.G., Majumder, P.K, et al. Androgen-induced differentiation and tumorgenicity of human prostate epithelial cells. (2004) Cancer Res 64(24): 8867-8875.
Pubmed || Crossref || Others - 65. Stanbrough, M., Leav, I., Kwan, P.W., et al. Prostatic intraepithelial neoplasia in mice expressing an androgen receptor transgene in prostate epithelium. (2001) Proc Naal Acad Sci USA 98(19): 10823-10828.
Pubmed || Crossref || Others - 66. Mononen, N., Syrjäkoski, K., Matikainen, M., et al. Two percent of Finnish prostate cancer patients have a germline mutation in the hormone-binding domain of the androgen receptor gene. (2000) Cancer Res 60(22): 6479-6481.
Pubmed || Crossref || Others - 67. Koivisto, P.A., Hyytinen, E.R., Matikainen, M., et al. Germline mutation analysis of the androgen receptor gene in Finnish patients with prostate cancer. (2004) J Urol 171(1): 431-433.
Pubmed || Crossref || Others - 68. Harris, S.E., Rong, Z., Harris, M.A., et al. Androgen receptor in human prostate carcinoma LNCaP/Adep cells contains a mutation which alters the specificity of the steroid-dependent transcriptional activation region. In:Bell L, editor. (1990) Proceedings of the 72nd Annual Meeting of the Endocrine Society: Atlanta (GA). Bethesda (MD): The Endocrine Society.
Pubmed || Crossref || Others - 69. Veldscholte, J., Ris-Stalpers, C., Kuiper, G.G., et al. A mutation in the ligand and binding domain of the androgen receptor of human LNCap cells affects steroid binding characteristics and response to anti-androgens. (1990) Biochem Biophys Res Commun 173(2): 534-540.
Pubmed || Crossref || Others - 70. Culig, Z., Hobisch, A., Cronauer, M.V., et al. Mutant androgen receptor detected in an advanced-stage prostatic carcinoma is activated by adenal androgens and progesterone. (1993) Mol Endocrinol 7(12): 1541-1550.
Pubmed || Crossref || Others - 71. Gaddipati, J.P., McLeod, D.G., Heidenberg, H.B., et al. Frequent detection of codon 877 mutation in the androgen receptor gene in advanced prostate cancer. (1994) Cancer Res 54(11): 2861-2864.
Pubmed || Crossref || Others - 72. Taplin, M.E., Bubley, G.J., Shuster, T.D., et al. Mutation of the androgen receptor gene in metastatic androgen-independent prostate cancer. (1995) N Engl J Med 332(21): 1393-1398.
Pubmed || Crossref || Others - 73. Suzuki, H., Akakura, K., Komiya, A., et al. Codon 877 mutations in the androgen receptor gene in advanced prostate cancer: relation to antiandrogen withdrawal syndrome. (1996) Prostate 29(3): 153-158.
Pubmed || Crossref || Others - 74. Southwell, J., Chowdhury, S.F, Gottlieb, B., et al. An investigation into CAG repeat length variation and N/C terminal interactions in the T877A mutant androgen receptor found in prostate cancer. (2008) J Steroid Biochem Mol Biol 111(1-2): 138-146.
Pubmed || Crossref || Others - 75. Newmark, J.R., Hardy, D.O., Tonb, D.C., et al. Androgen receptor gene mutations in human prostate cancer. (1992) Proc Natl Acad Sci USA 89(14): 6319-623.
Pubmed || Crossref || Others - 76. Nyquist, M.D., Li, Y., Hwang, T.H., et al. TALEN-engineered AR gene rearrangements reveal endocrine uncoupling of androgen receptor in prostate cancer. (2013) PNAS 110(43): 17492-17497.
Pubmed || Crossref || Others - 77. Tepper, C.G., Boucher, D.L., Ryan, P.E., et al. Characterization of a novel androgen receptor mutation in a relapsed CWR22 prostate cancer xenograft and cell line. (2002) Cancer Res 62(22): 660-6614.
Pubmed || Crossref || Others - 78. Shi, X.B., Xue, L.,Tepper, C.G., et al. The oncogenic potential of a prostate cancer-derived androgen receptor mutant. (2007) Prostate 67(6): 591-602.
Pubmed || Crossref || Others - 79. Kung, H.S., Evans, C.P. Oncogenic activation of androgen receptor. (2009) Urol Oncol 27(1): 48-52.
Pubmed || Crossref || Others - 80. Sun, S.H., Sprenger, C.C., Vessella, R.L., et al. Castration resistance in human prostate cancer is conferred by a frequently occurring androgen receptor splice variant. (2010) J Clin Invest 120(8): 2715-2730.
Pubmed || Crossref || Others - 81. Young, L., Creevey, L., Ali, A., et al. Abstract p3-05-21 in Thirty- Seventh Annual CTRC-AACR San Antonio Breast Cancer. (2015) Cancer Research 75(9).
Pubmed || Crossref || Others - 82. Liang, M., Adisetiyo, H., Liu, X., et al. Identification of androgen receptor splice variants in the pten deficient murine prostate cancer model. (2015) PLoS One 10(7): e0131232.
Pubmed || Crossref || Others - 83. Gucalp, A., Tolaney, S., Isakoff, S.J., et al. Phase II trial of bicalutamide in patients with androgen receptor-positive, estrogen receptor-negative metastatic breast cancer. (2013) Clin Cancer Res 19(19): 5505-5512.
Pubmed || Crossref || Others - 84. Coindet, J. New researches on the effects of iodine, and on sureties, surge in the treatment of goitre by this new urge. (1821) Ann Chimie Phys 16: 252-266.
Pubmed || Crossref || Others - 85. Goldberg, R.C., Chaikoff, I.L. Induction of thyroid cancer in the rats by radioactive iodine. (1952) Arch Pathol 53(1): 22-28.
Pubmed || Crossref || Others - 86. Suzuki, H., Higuchi, T., Hashimoto, H., et al. A case of endemic goiter along the seashores of Hidaka District, Hokkaido. (1962) Jpn J Med Sci Biol 51: 781-786.
Pubmed || Crossref || Others - 87. Mussig, K., Thamer, C., Bares, R., et al. Iodine-induced thyrotoxicosis after ingestion of kelp-containing tea. (2006) J Gen Intern Med 21(6): C11-C14.
Pubmed || Crossref || Others - 88. Horn-Ross, P.L., Morris, J.S., Lee, M., et al. Iodine and thyroid cancer risk among women in a multiethnic population:the Bay Zrea Thyroid Cancer Study. (2001) Cancer Epidemiol Biomarkers Prev 10(9): 979-985.
Pubmed || Crossref || Others - 89. Giusti, F., Falchetti, A., Franceschelli, F., et al. Thyroid cancer: current molecular perspective. (2010) J Oncol 2010: 17.
Pubmed || Crossref || Others - 90. Michikawa,T., Inoue, M., Shimazu,T., et al. Seaweed consumption and the risk of thyroid cancer in women: the Japan Public Health Center-based prospective study. (2012) Eur J Cancer Prev 21(3): 254-260.
Pubmed || Crossref || Others - 91. Schneider, D.F., Chen, H. New developments in the diagnosis and treatment of thyroid cancer. (2013) CA Cancer J Clin 63(6): 373-394.
Pubmed || Crossref || Others - 92. Chandrasekaren, M., Ramadevi, K. Thyromegaly and iodine nutritional status in a tertiary care hospital in South India. (2013) Indian J Endocrinol Metab 17(2): 260-264.
Pubmed || Crossref || Others - 93. Choi, W.J., Kim, J. Dietary factors and risk of thyroid cancer: A review. (2014) Clin Nutr Res 3(2): 75-88.
Pubmed || Crossref || Others - 94. Varricchio, L., Masselli, E., Alfani, E., et al. The dominant negative beta isoform of the glucocorticoid receptor is uniquely expressed in erythroid cells expanded from polycythemia vera patients. (2011) Blood 118: 425-423.
Pubmed || Crossref || Others - 95. Mikose, C.A., Brickley, D.R., Sharkey, M.S., et al. Glucocorticoid receptor-mediated protection from apoptosis is associated with induction of the serine/threonine survival kinase gene,sgk-1. (2001) J Biol Chem 276(20): 16649-16654.
Pubmed || Crossref || Others - 96. Melhem, A., Yamada, S.D., Fleming, G.F., et al. Administration of glucocorticoids to ovarian cancer patients is associated with expression of the anti-apoptotic gene SGK1 and MKP1/DUSP1 in ovarian tissues. (2009) Clin Cancer Res 15(9): 3196-3204.
Pubmed || Crossref || Others - 97. Isikbay, M., Otto, K., Kregel, S., et al. Glucocorticoid receptor activity contributes to resistance to androgen-targeted therapy in prostate cancer. (2014) Horm Cancer 5(2): 72-89.
Pubmed || Crossref || Others - 98. Mirand, E.A., Reiniiard, M.C.,Goltz, H.L., et al. Development of sarcomas in Marsh-Albino mice following injection of desoxycorticosterone acetate(DCA) in sesame oil. (1953) Proc Soc Exp Biol Med 83(1): 14-17.
Pubmed || Crossref || Others - 99. Lien, H.C., Lu, Y.S., Cheng, A.L., et al. Differential expression of glucocorticoid receptor in human breast tissue and related neoplasms. (2006) J Pathol 209(3): 317-327.
Pubmed || Crossref || Others - 100. Moutsatsou, P., Papavassiliou, A.G. The glucocorticoid receptor signaling in breast cancer. (2007) J Cell Mol Med 12(1): 145-163.
Pubmed || Crossref || Others - 101. Vilasco, M., Communal, L., Mourra, N., et al. Glucocorticoid receptor and breast cancer. (2011) Breast Cancer Res Treat 130(1): 1-10.
Pubmed || Crossref || Others - 102. Krishnan, A.V., Zhao, X.Y., Swami, S., et al. A glucocorticoid-responsive mutant androgen receptor exhibits unique ligand specificity: therapeutic implications for androgen- independent prostate cancer. (2002) Endocrinology 143(5): 1889-1900.
Pubmed || Crossref || Others - 103. Simanainen, U., Lampinen, A., Henneicke, H., et al. Long-term corticosterone treatment induced lobe- specific pathology in mouse prostate. (2011) Prostate 71(3): 289-297.
Pubmed || Crossref || Others - 104. Ebisawa, T., Tojo, K., Tajima, N., et al. Immunohistochemical analysis of 11-beta -hydroxysteroid dehydrogenase type 2 and glucocorticoid receptor in subclinical Cushing's disease due to pituitary macroadenoma. (2008) Endocr Pathol 19(4): 252-260.
Pubmed || Crossref || Others - 105. Karl, M., Von, Wichert, G., Kempter, E., et al. Nelson's syndrome associated with somatic frame shift mutation in the glucocorticoid receptor gene. (1996) J Clin Endocrinol Metab 81(1):124-129.
Pubmed || Crossref || Others - 106. Newfield, R.S., Kalaitzoglou, G., Licholai, T., et al. Normocorticolemic Cushing's syndrome initially presenting with increased glucocorticoid receptor number. (2000) J Clin Endocrinol Metab 85(1): 14-21.
Pubmed || Crossref || Others - 107. Johanssen, S., Allolio, B. Mifepristone (RU486) in Cushing's syndrome. (2007) Eur J Endocrinol 157(5): 561-569.
Pubmed || Crossref || Others - 108. Skor, M.N., Wonder, E.L., Kocherginsky, M., et al. Glucocorticoid receptor antagonism as a novel therapy for triple-negative breast cancer. (2013) Clin Cancer Res 19(22): 6163-6172.
Pubmed || Crossref || Others - 109. Risch, H. Hormonal etiology of epithelial ovarian cancer, with a hypothesis concerning the role of androgens and progesterone. (1998) J Natl Cancer Inst 90(23): 1774-1786.
Pubmed || Crossref || Others - 110. Althuis, M.D., Fergenbaum, J.H., Garcia-Closas, M., et al. Etiology of hormone receptor-defined breast cancer: A systematic review of the literature. (2004) Cancer Epidemiol Biomarkers Prev 13(10): 1558-1568.
Pubmed || Crossref || Others - 111. Richards, J.S., Farookhi, R. Gonadotrophins and ovarian-follicular growth. (1978) Clin Obstet Gynaecol 5(2): 363-373.
Pubmed || Crossref || Others - 112. Choi, J.H., Choi, K.C., Auersperg, N., et al. Overexpression of follicle-stimulating hormone receptor activates oncogenic pathways in preneoplastic ovarian surface epithelial cells. (2004) J Clin Endocrinol Metab 89(11): 5508-16.
Pubmed || Crossref || Others - 113. Hull, M.E., Kriner, M., Schneider, E., et al. Ovarian cancer after successful ovulation induction: a case report. (1996) J Reprod Med 41(1): 52-4.
Pubmed || Crossref || Others - 114. Shushan, A., Paltiel, O., Iscovich, J., et al. Human menopausal gonadotropin and the risk of epithelial ovarian cancer. (1996) Fertil Steril 65(1): 13-18.
Pubmed || Crossref || Others - 115. Brinton, L.A., Lamb, E.J., Moghissi, K.S., et al. Ovarian cancer risk after the use of ovulation-stimulating drugs. (2004) Obstet Gynecol 103(6): 1194-1203.
Pubmed || Crossref || Others - 116. Hauksdotti, H., Privalsky, M.L. DNA recognition by the aberrant retinoic acid receptor implicated in human acute promyelocytic leukemia. (2001) Cell Growth Differ 12(2): 85-98.
Pubmed || Crossref || Others - 117. Grignani, F., Ferrucci, P., Testa, U., et al. The acute promyelocytic leukemia-specific PML-RARa fusion protein inhibits differentiation and promotes survival of myeloid precursor cells. (1993) Cell 74(3): 423-431.
Pubmed || Crossref || Others - 118. Rousselot, P., Hardas, H., Patel, A., et al. The PML-RARa gene product of the t(15;17) translocation inhibits retinoic acid-induced granulocytic differentiation and mediated transactivation in human myeloid cells. (1994) Oncogene 9(2): 545-551.
Pubmed || Crossref || Others - 119. Yoshida, H., Kitamura, K., Tanaka, K., et al. Accelerated degradation of PML-retinoic acid receptor alpha(PML-RARa) oncoprotein by all-trans-retinoic acid in acute promyelocytic leukemia, possible role of the proteasome pathway. (1996) Cancer Res 56(13): 2945-2948.
Pubmed || Crossref || Others - 120. Kitareewan, S., Pitha-Rowe, I., Sekula, D., et al. UBE1L is a retinoid target that triggers PML/RAR alpha degradation and apoptosis in acute promyelocytic leukemia. (2002) PNAS 99(6): 3806-3811.
Pubmed || Crossref || Others - 121. Segalla, S., Rinaldi, L., Kilstrup-Nielsen, C., et al. Retinoic acid receptor a fusion to PML effects its transcriptional and chromatin-remodeling properties. (2003) Molecular and Cellular Biology 23(23): 8795-8808.
Pubmed || Crossref || Others - 122. Carbone, R., Botrugno, O.A., Ronzoni, S., et al. Recruitment of the histone methyltransferase SUV39H1 and its role in the oncogenic properties of the leukemia-associated PML-retinoic acid receptor fusion protein. (2006) Mol Cell Bio 26(4): 1288-1296.
Pubmed || Crossref || Others - 123. Nasr, R., Guillemin, M.C., Ferhi, O., et al. Eradication of acute promyelocytic leukemia-initiating cells through PML-RARA degradation. (2008) Nat Med 14(12): 1333-1342.
Pubmed || Crossref || Others - 124. Marstrand, T.T., Borup, R., Willer, A., et al. A conceptual framework for the identification of candidate drugs and drug targets in acute promyelocytic leukemia. (2010) Leukemia 24(7): 1265-1275.
Pubmed || Crossref || Others - 125. Lallemand-Breitenbach, V., de, The, H. A new oncoprotein catabolism pathway. (2010)Blood 116(13): 2200-2201.
Pubmed || Crossref || Others - 126. Podhorecka, M., Macheta, A. Acute promyelocytic leukemia--modern approach to disease pathogenesis and differentiation treatment. (2013) Postepy Hig Med Dosw 67: 1083-1089.
Pubmed || Crossref || Others - 127. Dos Santos, G.A., Kats, L., Pandolfi, P.P. Synergy against pml-RARa: targeting, transcription, proteolysis, differentiation, and self-renawal in acute promyelocytic leukemia. (2013) J Exp Med 210(13): 2793-2802.
Pubmed || Crossref || Others - 128. Humbert, M., Federzoni, E.A., Britschgi, A., et al. The tumor suppressor gene DAPK2 is induced by myeloid transcription factors pu.1 and c.EBPa dueing granulocytic differentiation but repressed by PML-RARa in APL. (2014) J Leuk Biol 95(1): 83-93.
Pubmed || Crossref || Others - 129. De Braekeleer, E., Douet-Guilbert, N., De Braekeleer, M. RARA fusion genes in acute promyelocytic leukemia:a review. (2014) Expert Rev Hematol 7(3): 347-357.
Pubmed || Crossref || Others - 130. Rietveld, L.E., Caldenhoven, E., Stunnenberg, H.G. Avian erythroleukemia: a model for corepressor function in cancer. (2001) Oncogene 20(24): 3000-3009.
Pubmed || Crossref || Others - 131. Cohen, S., Ushiro, B., Stoscheck, C., et al. A native 170,000 epidermal growth factor receptor kinase complex from shed membrane vesicles. (1982) J Biol Chem 257(3): 1523-1531.
Pubmed || Crossref || Others - 132. Brown, G.L., Nanney, L.B., Griffen, J., et al. Enhancment of wound healing by topical treatment with epidermal growth factor. (1989) N Engl J Med 321(2):76-79.
Pubmed || Crossref || Others - 133. Zandi, R., Larsen, A.B., Andersen, P., et al. Mechanisms for oncogenic activation of the epidermal growth factor receptor. (2007) Cell Signal 19(10): 2013-2023.
Pubmed || Crossref || Others - 134. Laisney, J.A., Mueller, T.D., Schartl, M., et al. Hyperactivation of constitutively dimerized oncogenic EGF receptors by autocrine loop. Oncogene (2013) 32(19): 2403-2411.
Pubmed || Crossref || Others - 135. Glynn, S.A., Boerima, B.J., Dorsey, T.H., et al. Increased NOS2 predicts poor survival in estrogen receptor-negative breast cancer patients. (2010) J Clin Invest 120(11): 3843-3854.
Pubmed || Crossref || Others - 136. Kim, Y.J., Apetri, M., et al. Differential effects of tyrosine kinase inhibitors on normal and oncogenic EGFR signaling and downstream effectors. (2015) Mol Cancer Res 13(4): 765-774.
Pubmed || Crossref || Others - 137. Ullrich, A. Growth factor receptors in oncogenesis. (1992) The American Association for Cancer Research Annual Meeting 33: 589-590.
Pubmed || Crossref || Others - 138. O'Connor, R. Concealed cargo within the tumor microenvironment: microvescles disseminate oncogenic receptors among cancer cells. Cancer Biol Ther (2008) 7(): 1350-1351.
Pubmed || Crossref || Others - 139. Gabitova, L., Gorin, A., Astsaturov, I. Molecular pathways: sterols and receptor signaling on cancer. Clini Cancer Res (2014) 20(1): 28-34.
Pubmed || Crossref || Others - 140. Shimizu, N., Kondo, I. Hyperproduction of EGF receptor in human A431 cell is regulated by a translocation chromosome, t (7; 11) (p22; q23). (1982) Cytogenetics Cell Gen 32: 316-317.
Pubmed || Crossref || Others - 141. Merline, G.T., Xu, Y.H., Ishii, S., et al. Amplification and enhanced expression of the epidermal growth factor receptor gene in A431 human carcinoma cells. (1984) Science 224(4647): 417-419.
Pubmed || Crossref || Others - 142. Ullrich, A., Coussens, J., Hayflick, J.S., et al. Human epidermal growth factor receptor cDNA sequence and aberrant expression of the amplified gene in A431epidermoid carcinoma cells. (1984) Nature 309(5967): 418-425.
Pubmed || Crossref || Others - 143. Santon, J.B., Cronin, M.T., Macleod, C.L., et al. Effects of epidermal growth factor receptor concentration on tumorigenicity of A431 cells in nude mice. (1986) Cancer Res 46(9): 4701-4705.
Pubmed || Crossref || Others - 144. Kamata, N., Chida, K., Rikimaru, K., et al. Growth-inhibitory effects of epidermal growth factor and overexpression of its receptors on human squamous cell carcinomas in culture. (1986) Cancer Res 46(4): 1648-1653.
Pubmed || Crossref || Others - 145. Minke, J.M.H.M., Schuuring, E.D., Van den Berghe, R., et al. Isolation of two distinct epithelial cell lines from a single feline mammary carcinoma with different tumorigenic potential in nude mice and expressing different levels of epidermal growth factor receptor. (1991) Cancer Res 51(15): 4028-4031.
Pubmed || Crossref || Others - 146. Lee, J.C., Vivanco, I., Beroukhim, R., et al. Epidermal growth factor receptor activation in glioblastoma through novel misdense mutations in extracellular domain. (2006) PLoS medicine 3(12): e485.
Pubmed || Crossref || Others - 147. Miltra, S., Han, S., Soderstram, K., et al. Preferential expression of an oncogenic receptor in brain tumor stem cells: Identification and targeting using an engineered antibody. (2009) Proc Am Assoc Cancer Res 69(9).
Pubmed || Crossref || Others - 148. Hembrough, T., Thyparambil, S., Liao, W.L., et al. Quantitative multiplexed SRM analysis of oncogenic receptors in FFPE colorectal carcinoma tissue. (2012) Cancer Res 72(8): 5537.
Pubmed || Crossref || Others - 149. Godin-Heymann, N., Bryant, I., Rivera, M.N., et al. Oncogenic activity of epidermal growth factor receptor kinase mutant alleles is enhanced by the T790M drug resistance mutation. (2007) Cancer Res 67(15): 7319-7326.
Pubmed || Crossref || Others - 150. Rosell, R., Molina, M.A., Costa, C., et al. Pretreatment EGFR T790M mutation and BRCA1 mRNA expression in erlotinib-treated advanced non-small-cell lung cancer patients with EGFR mutations. (2011) Clin Cancer Res 17(5): 1160-1168.
Pubmed || Crossref || Others - 151. Karachaliou, N., Gimenez-Capitan, A., Drozdowskyj, A., et al. ROR1 as a novel therapeutic target for EGFR-mutant non-small-cell lung cancer patients with the EGFR T790M mutation. (2014) Transl Lung Cancer Res 3(3): 122-190.
Pubmed || Crossref || Others - 152. Gallant, J.N., Sheehan, J.H., Shaver, T.M., et al. EGFR kinase domain duplication (EGFR-KDD) is a novel oncogenic driver in lung cancer that is clinically responsive to afatinib. (2015) Cancer Discov 5(11): 1155-1163.
Pubmed || Crossref || Others - 153. Konduri, K., Gallant, J.N., Chae, Y.K., EGFR fusions as Novel Therapeutic Targets in lung cancer. (2016) Cancer Discov 6(6): 601-611.
Pubmed || Crossref || Others - 154. Ichihara, E., Takeda, H., Kubo, T., et al. Chemopreventive effect of gefitinib on nonsmoking-related lung tumorigenesis in activating epidermal growth factor receptor transgenic mice. (2009) Cancer Res 69(17) :7088-7095.
Pubmed || Crossref || Others - 155. Blesa, G.J.M., Mollá, S.B., Esparcia, M.F., et al. Durable complete remission of a brainstem glioma treated with a combination of bevacizumab and cetuximab. (2012) Case Rep Oncol 5(3): 676-681.
Pubmed || Crossref || Others - 156. Rodriguez, P.C., Rodriguez, G., Gonzalez, G., et al. Clinical development and perspectives of CIMAvax EGF, Cuban vaccine for non-small-cell lung cancer therapy. (2010) MEDICC Rev 12(1): 17-23.
Pubmed || Crossref || Others - 157. Gonzalez, G., Crombet, T., Lage, A. Chronic vaccination with a therapeutic EGF-based cancer vaccine: a review of patients receiving long lasting treatment. (2011) Curr Cancer Drug Target 11(1): 103-104.
Pubmed || Crossref || Others - 158. Paugh, B.S., Zhu, X., Qu, C., et al. Novel oncogenic PDGFRA mutations in pediatric high-grade gliomas. (2013) Cancer Res 73(20): 6219-6229.
Pubmed || Crossref || Others - 159. Yamada, Y., Rothenberg, M.E., Lee, A.W., et al. The FIPIL1-PDGFRA fusion gene cooperates with IL-5 to induce murine hyper-eosinophilic syndrome (HES)/chronic eosinophilic leukemia (CEL)-like disease. (2006) Blood 107(10): 4071-4079.
Pubmed || Crossref || Others - 160. Golub, T.R., Barker, G.F., Louett, M., et al. Fusion of PDGF receptor beta to a novel ets-like gene,tel,in chronic myelomonocytic leukemia with t(5;12) chromosomal translocation. (1994) Cell 77(2): 307-316.
Pubmed || Crossref || Others - 161. Mizuki, M., Ueda, I., Matsumura, I., et al. Oncogenic receptor tyrosine kinase in leukemia. Cell Mol Biol (2003) 49(6): 907-922.
Pubmed || Crossref || Others - 162. Matsumura, I., Mizuki, M., Kanakura, Y., Roles for deregulated receptor tyrosine kinase and their downstream signaling molecules in hematologic malignancies. (2008) Cancer Sci 99(): 479-485.
Pubmed || Crossref || Others - 163. Lierman, E., Lahortiga, I., Miegroet, H.V., et al. The ability of sorafenib to inhibit oncogenic PDGFRbeta and FLT3 mutants and overcome resistance to other small molecular inhibitors. (2007) Haematologica 92(1): 27-34.
Pubmed || Crossref || Others - 164. Holzmann, K., Grunt, T., Heinzle, C., et al. Alternative splicing of fibroblast growth factor receptor IgIII loops in cancer. (2012) J Nucleic Acids : 950508.
Pubmed || Crossref || Others - 165. Mcgee, G.S., Davidson, J.M., Buckley, A., et al. Recombinant basic fibroblast growth factor acclerate wound healing. (1988) J Surg Res 45(): 145.
Pubmed || Crossref || Others - 166. Oda, Y., Kagami, H., Ueda, M. Acclerating effects of basic growth factor on wound healing of rat palatal mucosa. (2004) J Oral Maxillofac Surg 62(1): 73-80.
Pubmed || Crossref || Others - 167. Apperley, J.F., Gardenbas, M., Melo, J.V., et al. Response to imatinib mesylate in patients with chronic myeloproliferative disorders with rearrangements of platelet-derived growth factor receptor beta. (2002) N Engl J Med 347(): 481-487.
Pubmed || Crossref || Others - 168. Cools, J., De Angelo, D.J., Gotlib, J., et al. A tyrosine kinase created by fusion of the PDGFRA and FIPIL1 gene as a therapeutic target of imatinib in idiopathic hypereosinophilic syndrome. (2003) N Engl J Med 348(13):1201-1214.
Pubmed || Crossref || Others - 169. Klion, A.D., et al. Relapse following discontinuation of imatinib mesylate therapy for FIPIL1/ PDGFRA-positive chronic eosinophilic leukemia: implications for optimal dosing. (2007) Blood 110(10): 3552-3556.
Pubmed || Crossref || Others - 170. Jovanovic, J.V., Score, J., Waghorn, K., et al. Low-dose imatinib mesylate leads to rapid molecular responses and achievement of complete molecular remission in FIPIL1-PDGFRA-positive chronic eosinophilic leukemia. (2007) Blood 109(11): 4635-4640.
Pubmed || Crossref || Others - 171. Helbig, G., A single weekly dose of imatinib is sufficient to induce and maintain remission of chronic eosinophilic leukemia in FIPIL1-PDGFRA-expressing patients.(2008) Br J Haematol 141(2): 200- 204.
Pubmed || Crossref || Others - 172. Arefi, M., et al. Response to imatinib mesylate in patients with hypereosinophilic syndrome. (2012) Int J Hematol 96(): 320-326.
Pubmed || Crossref || Others - 173. Kuroiwa, M., Hiwatari, M., Hirato, J., et al. Advanced-stage gastrointestinal tumor treated with imatinib in a 12-year-old girl with a unique mutation of PDGFRA. (2005) J Pediatr Surg 40(11): 1798-1801.
Pubmed || Crossref || Others - 174. MacDougall, C.A., Vargas, M., Soares, C.R., et al. Involvement of HGF/SF-Met signaling in prostate adenocarcinoma cells: evidence for alternative mechanisms leading to a metastatic phenotype in pr-14C. (2005) Prostate 64(2): 139-148.
Pubmed || Crossref || Others - 175. Spee, B., Arends, B., Van den Ingh, T., et al. Major HGF-mediated regenerative pathways are similarly affected in human and canine cirhosis. Comp Hepatol (2007) 6: 8.
Pubmed || Crossref || Others - 176. Fieten, H., Spee, B., Ijzer, J., et al. Expression of hepatocyte growth factor and the proto-oncogenic receptor c-Met in canine osteosarcoma. (2009) Vet Pathol 46(5): 869-877.
Pubmed || Crossref || Others - 177. Nakamura, T., Sakai, K., Nakamura, T., et al. Hepatocyte growth factor twenty years on: Much more than a growth factor. (2011) J Gastroenterol Hepatol. 26 Suppl (1): 188-202.
Pubmed || Crossref || Others - 178. Ishiki, Y., Ohnishi, H., Muto, Y., et al. Direct evidence that hepatocyte growth factor is a hepatotrophic factor for liver regeneration and for potent anti-hepatitis action in vivo. (1992) Hepatology 16(5): 1227–1235.
Pubmed || Crossref || Others - 179. Matsuda, Y., Matsumoto, K., Ichida, T., et al. Hepatocyte growth factor suppresses the onset of liver cirrhosis and abrogates lethal hepatic dysfunction in rats. (1995) J. Biochem 118(3): 643–649.
Pubmed || Crossref || Others - 180. Jeffers, M., Rong, S., Anver, M., et al. Autocrine hepatocyte growth factor/scatter factor-Met signaling induces transformation and the invasive/metastatic phenotype in C127 cells. (1996) Oncogene 13(): 853-856.
Pubmed || Crossref || Others - 181. Olwill, S.A., Joffroy, C., Gille, H., et al. A highly potent and specific MET therapeutic protein antagonist with both ligand-dependent and ligand-independent activity. (2003) Mol Cancer Ther 12(11): 2459-2471.
Pubmed || Crossref || Others - 182. Kentis, A., Reed, C., Rice, K.L., et al. Autocrine activation of the Met receptor tyrosine kinase in acute myeloid leukemia. (2012) Nat Med 18(7): 1118-1122.
Pubmed || Crossref || Others - 183. Kanda, H., Tajima, H., Lee, G.H., et al. Hepatocyte growth factor transforms immortalized mouse liver epithelial cells. (1993) Oncogene 8(11): 3047-3053.
Pubmed || Crossref || Others - 184. Shiota, G., Rhoads, D.B., Wang, T.C., et al. Hepatocyte growth factor inhibits growth of hepatocellular carcinoma cells. (1992) Proc Natl Acad Sci USA 89(1): 373-377.
Pubmed || Crossref || Others - 185. Gentile, A., Trusolino, L., Comoglio, P.M. The Met tyrosine kinase receptor in development and cancer. (2008) Cancer Metastasis Rev 27(1): 85-94.
Pubmed || Crossref || Others - 186. Medová, M., Pochon, B., Streit, B. The novel ATP-competitive inhibitor of the MET hepatocyte growth factor receptor EMD1214063 displays inhibitory activity against selected MET-mutated variants. (2013) Mol Cancer Ther 12(11): 2415-2424.
Pubmed || Crossref || Others - 187. Gual, P., Giordano, S., Anguissola, S., et al. Gab l phosphorylation: a novel mechanism for negative regulation of HGF receptor signaling. (2001) Oncogene 20(2): 156-166.
Pubmed || Crossref || Others - 188. Vigna, E., Pacchiana, G., Chiria, C., et al. Targeted therapy by gene transfer of monovalent antibody fragment the Met oncogenic receptor. (2014) J Mol Med (Berl) 92(1): 65-76.
Pubmed || Crossref || Others - 189. Vigna, E., Chiriaco, C., Cignetto S., et al. Inhibition of ligand-independent constitutive activation of the Met oncogenic receptor by the engineered chemically -modified antibody DN30. (2015) Mol Oncol 9(9): 1760-1772.
Pubmed || Crossref || Others - 190. Zhu, T., Starling-Emerald, B., Zhang, X., et al. Oncogenic transformation of human mammary epithelial cells by autocrine human growth hormone. (2005) Cancer Res 65(1): 317-324.
Pubmed || Crossref || Others - 191. Conway-Campbell, B.L., Wooh, J.W., Brooks, A.J., et al. Nuclear targeting of the growth hormone receptor results in dysregulation of cell proliferation and tumorigenesis. (2007) Proc Natl Acad Sci USA 104(33): 13331-13336.
Pubmed || Crossref || Others - 192. Lincoln, D.T., Kaiser, H.E., Raju, G.P., et al. Growth hormone and colorectal carcinoma: localization of receptors. (2000) In Vivo 14(1): 41-49.
Pubmed || Crossref || Others - 193. Yash, C., Waters, M.J., Brooks, A., et al. The growth hormone receptor mediated oncogenesis. (2014)
Pubmed || Crossref || Others - 194. Rosenbloom, A.L., Guevara-Aguirre, j., Rosenfeld, R.G., et al. Growth hormone receptor deficiency in Ecuador. (1999) J Clin Endocrinol Metab 84(12): 4436-4443.
Pubmed || Crossref || Others - 195. Palmiter, R.D., Brinster, R.L., Hammer, R.E., et al. Dramatic growth of mice that develop from eggs microinjected with metallothionein-growth hormone fusion genes. (1982) Nature 300(5893): 611-615.
Pubmed || Crossref || Others - 196. Orian, J.M., Tamakoshi, K., Mackay, I.R., et al. New murine model for hepatocellular carcinoma; transgenic mice expressing metallothionein-ovine growth hormone fusion gene. (1990) J Natl Cancer Inst 82(5): 393-398.
Pubmed || Crossref || Others - 197. Orme, S.M., McNally, R.J., Cartwright, R.A., et al. Mortality and cancer incidence in acromegaly:a retrospective cohort study. United Kingdom Acromegaly Study Group. (1998) J Clin Endocrinol Metab 83(8): 2730-2734.
Pubmed || Crossref || Others - 198. Beuschlein, F., Strasburger, C. J., Siegerstetter, V., et al. Acromegaly caused by secretion of growth hormone by a non-Hodgkin's lymphoma. (2000) N Engl J Med 342(25): 1871-1876.
Pubmed || Crossref || Others - 199. Tornell, J., Rymo, L., Isaksson, O.G. Induction of mammary adenocarcinomas in metallothione in promoter-human growth hormone transgenic mice. (1991) Int J Cancer 49(1): 114-117.
Pubmed || Crossref || Others - 200. Jenkins, P.J. Cancer associated with acromegaly. (2006) Neuroendocrinology 83(3-4): 218-23.
Pubmed || Crossref || Others - 201. Mayo KE, etal. Dramatic pituitary hyperplasia in transgenic mice expressing a human growth hormone-releasing factor gene. (1988) Mol Endocrinol 2(7): 606-612.
Pubmed || Crossref || Others - 202. Asa, S.L., Kovacs, K., Stefaneanu, L., et al. Pituitary adenomas in mice transgenic for growth hormone- releasing hormone. (1992) Endocrinology 131(5): 2083-2089.
Pubmed || Crossref || Others - 203. Wang, L.H., Lin, B., Jong, S.M., et al. Activation of transforming potential of the human insulin receptor gene.(1987) Proc Natl Acad Sci U S A 84(16): 5725-5729.
Pubmed || Crossref || Others - 204. Zong, C.S., Zeng, L., Jiang, Y., et al. Stat3 plays an important role in oncogenic ROS- and insulin-like growth factor I receptor-induced anchorage-independent growth. (1998) J Bio Chem 273(43): 28065-28072.
Pubmed || Crossref || Others - 205. Kaleko, M., Rutter, W.J., and Miller, A.D. Over expression of the human insulin like growth factor-1 receptor promotes ligand-dependent neoplastic transformation. (1990) Mol Cell Biol 10(2): 464-473.
Pubmed || Crossref || Others - 206. Giorgino, F., Belfiore, A., Milazzo, G., et al. Over expression of insulin receptors in fibroblast and ovary cells induces a ligand-mediated transformed phenotype. (1991) Mol Endocrinol 5(3): 452-459.
Pubmed || Crossref || Others - 207. Karrman, K., Kjeldsen, E., Lassen, C., et al. The t(X; 7) (q22;q34) in paediatric T-cell acute lymphoblastic leukemia results in overexpression of the insulin receptor substrate 4 gene through illegitimate recombination with the T-cell receptor beta locus. (2009) Br J Haematol 144(4): 546-551.
Pubmed || Crossref || Others - 208. Hankinson, S.E., Willett, W.C., Colditz, G.A., et al. Circulating concentrations of IGF-1 and risk of breast cancer.(1998) Lancet 351(9113): 1391-1396.
Pubmed || Crossref || Others - 209. Jones, R.A., Campbell, C.I., Gunther, E.J., et al. Transgenic overexpression of IGF-1R disrupts mammary ductal morphogenesis and induces tumor formation. (2007) Oncogene26(11): 1636-1644.
Pubmed || Crossref || Others - 210. Carboni J.M., Lee, A.V., Hadsell, D.L., et al. Tumor development by transgenic expression of a constitutively active insulin-like growth factor I receptor. (2005) Cancer Res 65(9): 3781-3787.
Pubmed || Crossref || Others - 211. Pisani, P. Hyper-insulinaema and cancer, meta-analyses of epidemiological studies. (2008) Arch Physiol Biochem 114(10: 63-70.
Pubmed || Crossref || Others - 212. Klinger, B., Laron, Z. Three year IGF-1 treatment of children with Laron syndrome. (1995) J Pediatr Endocrinol Metab 8(3): 149-158.
Pubmed || Crossref || Others - 213. Rosenbloom, A.L. Mecasermin (recombinant human insulin-like growth factor 1). (2009) Adv Ther 26(1): 40-54
Pubmed || Crossref || Others - 214. Ranke, M.B., Savage, M.O., Chatelain, P.G. et al. Long-term treatment of GH insensitivity syndrome with IGF-I.Results of the European multicenter study. (1999) Horm Res 51:128-34.
Pubmed || Crossref || Others - 215. McKinsey, E.L., Parrish, J.K., Irwin, A.E., et al. A novel oncogenic mechanism in Ewing sarcoma involving IGF pathways targeting by EWS/Fil1-regulated microRNAs. (2011) Oncogene 30(49): 4910-4920.
Pubmed || Crossref || Others - 216. Naing, A., LoRusso, P., Fu. S., et al. Insulin growth factor-receptor (IGF-1R) antibody cixutumumab combined with the mTOR inhibitor temsirolimus in patients with refractory Ewing's sarcoma family tumors. (2012) Clin Cancer Res 18(9): 2625-2631.
Pubmed || Crossref || Others - 217. Tap, W.D., Demetri, G., Barnette, P., et al. Phase II study of ganitumab,a fully human anti-type-1 IGF-1 receptor antibody,in patients with metastatic Ewing family tumors or desmoplasiic small round cell tumors. (2012) J Clin Oncol 30: 1849-1856.
Pubmed || Crossref || Others - 218. Sommer, A., Kopitz, C., Schatz, C.A., et al. Preclinical efficacy of the auristatin-based antibody-drug conjugate BAY1187982 for the treatment of FGFR2-positive solid tumors. (2016) Cancer Res 76(21): 6331-6339.
Pubmed || Crossref || Others - 219. Kostmann, R. Infantile genetic agranulocytosis: A review with presentation of 10 cases. (1975) Acta Pediatri Scand 64(2): 362-368.
Pubmed || Crossref || Others - 220. Dale, D.C., Bonilla, M.A., Davis, M.W., et al. A randomized controlled phase III trial of recombinant human granulocyte colony stimulating factor (filgrastim) for treatment of severe chronic neutropenia. (1993) Blood 81(10): 2496-2502.
Pubmed || Crossref || Others - 221. Hubel, K., Dale, D.C., and Liles, W.C. Therapeutic use of cytokines to modulate phagocyte function for the treatment of infectious diseases: current status of granulocyte colony-stimulating factor, granulocyte-macrophage colony-stimulating factor, macrophage colony-stimulating factor, and interferon-gamma. (2002) J Infect Dis 185(10): 1490-1501.
Pubmed || Crossref || Others - 222. Zeidler, C., Boxer, L., Dale, D.C., et al. Management of Kostmann syndrome in the G-CSF era. (2000) Br J Haematol 109(3): 490-495.
Pubmed || Crossref || Others - 223. Donini, M., Fontana, S., Savoldi, G., et al. G-CSF treatment of severe congenital neutropenia reverses neutropenia but does not correct the underlying functional deficiency of the neutrophil in defending against microorganisms. (2007) Blood 109(11): 4716-4723.
Pubmed || Crossref || Others - 224. Rosenberg, P.S., Zeidler, C., Bolyard, A.A., et al. Stable long-term risk of leukemia in patients with severe congenital neutropenia maintained on G-CSF therapy. (2010) Br J Haematol 150(2): 196-199.
Pubmed || Crossref || Others - 225. Beekman, R., and Touw, I.P. G-CSF and its receptor in myeloid malignancy. (2010) Blood 115(25): 5131-5136.
Pubmed || Crossref || Others - 226. Hunter, MG., Avalos, BR. Granulocyte colony-stimulating factor receptor mutations in severe congenital neutropenia transforming to acute myelogenous leukemia confer resistance to apoptosis and enhance cell survival. (2000) Blood 95(6): 2132-2137.
Pubmed || Crossref || Others - 227. Germeshausen, M., Ballmaier, M., Walter, K. Incidence of CSF3R mutations in SCN and relevance for leukemogenesis: results of a long-term survey. (2007) Blood 109(1): 93-99.
Pubmed || Crossref || Others - 228. Beel, K., Vandenberghe, P. G-CSF receptor (CSF3R) mutations in X-linked neutropenia evolving to acute leukemia or myelodysplasia. (2009) Haematologica 94(10): 1449-1452.
Pubmed || Crossref || Others - 229. Fleischman, A.G., Maxson, J.E., Luty, S.B., et al. The CSF3R T618I mutation cause a lethal neutrophilic neoplasia in mice that is responsive to therapeutic JAK inhibition. (2013) Blood 122(22): 3628-3631.
Pubmed || Crossref || Others - 230. Maxson, J.E., Gollib, J., Pollyea, D.A., et al. Oncogenic CSF3R mutations in chronic neutrophilic leukemia and atypical CML. (2013) N Engl J Med 368(19): 1781-1790.
Pubmed || Crossref || Others - 231. Plo, I., Zhang, Y., Le, Couedic, J.P., et al. An activating mutation in the CSF3R gene induces a hereditary chronic neutrophilia. (2009) JEM 206(8): 1701-1707.
Pubmed || Crossref || Others - 232. Russell, L.J., De, Cadtro, D.G., Griffiths, M., et al. A novel translocation, t(14;19)(q32;p13), involving IGH@ and the cytokine receptor for erythropoietin. (2009) Leukemia 23(3): 614-617.
Pubmed || Crossref || Others - 233. Iacobucci, I., Roberts, K.G., Li, Y., et al. Cryptic truncating rearrangement of the erythropoietin receptor in ph-like acute lymphoblastic leukemia. (2014) Blood 124(21): 128.
Pubmed || Crossref || Others - 234. Iacobucci, I., Li, Y., Roberts, K.G., et al. Truncating erythropoietin receptor rearrangements in acute lymphoblastic leukemia. (2016) Cancer Cell 29(2): 186-200.
Pubmed || Crossref || Others - 235. Longmore, G.D., Pharr, P., Neumann, D., et al. Both megakaryocytopoiesis and erythropoiesis are induced in mice infected with a retrovirus expressing an oncogenic erythropoietin receptor. (1993) Blood 82(8): 2386-2395.
Pubmed || Crossref || Others - 236. de, la, Chapelle, A., Träskelin, A.L., and Juvonen, E. Truncated erythropoietin receptor cause dominantly inherited benign human erythrocytosis. (1993) PNAS 90(10): 4495–4499.
Pubmed || Crossref || Others - 237. Arcasoy, M.O., Karayal, A.F., Segal, H.M., et al. A novel mutation in the erythropoietin receptor gene is associated with familial erythrocytosis. (2002) Blood 99(8): 3066-3069.
Pubmed || Crossref || Others - 238. Forget, B.G., Degan, B.A., Arcasoy, M.D. Familial polycythemia due to truncations of the erythropoietin receptor. (2000) Trans Am Clin Climatol Assoc 111: 38-44.
Pubmed || Crossref || Others - 239. Perrotta, S., Cucciolla, V., Ferraro, M., et al. EPO receptor gain-of-fumction causes hereditary polycythemia, alters CD34 cell differentiation and increases circulating endothelial precursors. (2010) PLos One 5(8): e12015.
Pubmed || Crossref || Others - 240. Bento, C., Almeida, H., Maia, T.M., et al. Molecular study of congenital erythrocytosis in 70 unrelated patients revealed a potential causal mutation in less than half of the cases. (2013) Eur J Hematol 91(4): 361-368.
Pubmed || Crossref || Others - 241. Maruyama, M., Shibuya, H., Harada, H., et al. Evidence for aberrant activation of the interleukin-2 autocrine loop by HTLV-1-encoded p40x and T3/Ti complex triggering. (1987) Cell 48(2): 343-350.
Pubmed || Crossref || Others - 242. Yamada, G., Kitamura, Y., Taniguchi, T., et.al. Retroviral expression of the human IL-2 gene in a murine T cell line results in cell growth autonomy and tumorigenicity. (1987) The EMBO J 6(9): 2705-2709.
Pubmed || Crossref || Others - 243. Karasuyama, H., Tohyama, N., and Tada, T. Autocrine growth and tumorigenicity of interleukin-2- dependent helper T cells transfected with IL-2 gene. (1989) JEM 169(1): 13-25.
Pubmed || Crossref || Others - 244. Nagarkatt, M., Hassuneh, M., Seth, A., etal. Constitutive activation of the interleukin 2 gene in the induction of spontaneous in vitro transformation and tumorigenicity of T cells. (1994) PNAS 91(16): 7638-7642.
Pubmed || Crossref || Others - 245. Hassuneh, MR., Nagarkatti, P.S., and Nagarkatti, M. Evidence for the participation of interleukin-2 (IL-2) and IL-4 in the regulation of autonomous growth and tumorigenesis of transformed cells of lymphoid origin. (1997) Blood 89(2): 610-620.
Pubmed || Crossref || Others - 246. Laabi, Y., Gras, M.P., Carbonnei, F., et al. A new gene, BCM, on chromosome 16 is fused to the interleukin 2 gene by a t (4;16) (q26;p13) translocation in a malignant T cell lymphoma. (1992) EMBO J 11(11): 3897-3904.
Pubmed || Crossref || Others - 247. Goldsmith, M.A., Lai, S.Y., Xu, W., et al. Growth signal transduction by the human interleukin-2 receptor requires cytoplasmic tyrosines of the beta chain and non-tyrosine residues of the gamma c chain. (1995) J Biol Chem 270(37): 21729-37.
Pubmed || Crossref || Others - 248. Rosenberg, S.A., Lotze, M.T., Muul, L.M., et al. Observation on the systemic administration of autologous lymphokine- activated killer cells and recombinant interleukin-2 to patients with metastatic cancer. (1985) N Engl J Med 313(23): 1485-1492.
Pubmed || Crossref || Others - 249. Bernard, O., Ullrich, A., Green, W., et al. High-affinity interleukin 2 binding by an oncogenic hybrid interleukin 2-epidermal growth factor receptor molecule. (1987) PNAS 84(8): 2125-2129.
Pubmed || Crossref || Others - 250. Pike-Overzet, K., de, Ridder, D., Weerkamp, F., et al. Gene therapy:Is IL-2RG oncogenic in T-cell development?. (2006) Nature 443(7109): 1123.
Pubmed || Crossref || Others - 251. Grimaldi, J.C., Meeker, T.C. The t(5;14) chromosomal translocation in a case of acute lymphocytic leukemia joins the interleukin-3 gene to the immunoglobulin heavy chain gene. (1989) Blood 73(8): 2081 – 2085.
Pubmed || Crossref || Others - 252. Steelman, L.S., Algate, P.A., Balock, W.L., et al. Oncogenic effect of overexpression of the interleukin-3 receptor on hematopoietic cells. (1996) Leukemia 10(3): 528-542.
Pubmed || Crossref || Others - 253. Durum, S.K. IL-7 and TSLP receptors:twisted sisters. (2014) Blood 124(1): 106-110.
Pubmed || Crossref || Others - 254. Sasson, S.C., Zaunders, J.J., Kelleher, A.D. The IL-7/IL-7 receptor axis:understanding its central role in T-cell homeostasis and the challenge facing its utilization as a novel therapy. (2006) Curr Drug Targets 7(12): 1571-1582.
Pubmed || Crossref || Others - 255. Shochat, C., Tal, N., Gryshkova, V., et al. Novel activating mutations lacking cysteine in type I cytokine receptors in acute lymphoblastic leukemia. (2014) Blood 124(1): 106-110.
Pubmed || Crossref || Others - 256. Mansour, M.M., Reed, C., Eisenberg, A., et al. Targeting oncogenic interleukin-7 receptor signaling with N-acetylcysteine in T-cell acute lymphoblastic leukemia. (2013) Blood 122(21): 2535.
Pubmed || Crossref || Others - 257. Ueda, C., Akasaka, T., Kurata, M., et al. The gene for interleukin-21 receptor is the partner of BCL6 in t (3;16)(q27;p11),which is recurrently observed in diffuse large B-cell lymphoma. (2002) Oncogene 21(3); 368-376.
Pubmed || Crossref || Others - 258. Moody, P.R., Sayers, E.J., Magnusson, J.P., et al. Receptor crosslinking:A general method to trigger internalization and lysosomal targeting of therapeutic receptor:ligand complexes. (2015) Molecular Therapy 23(12): 1888-1898.
Pubmed || Crossref || Others - 259. Kirschning, C.J., Dreher, S., Maa, B., et al. Generation of anti-TLR2 intrabody mediating inhibition of macrophage surface TLR2 expression and TLR2-deriven cell activation. (2010) BMC Biotechnology 10: 31.
Pubmed || Crossref || Others - 260. Ornes, S. Antibody-drug conjugates. (2013) Proc Natl Acad Sci USA 110(34):13695.
Pubmed || Crossref || Others - 261. Zhao, Y. The oncogenic functions of nicotinic acetylcholine receptors. (2016) Journal of Oncology 2016(3): 1-9.
Pubmed || Crossref || Others