Tick Paralysis
Affiliation
Department of Dermatology and Post graduated from University of Carabobo, Venezuela
Corresponding Author
Jose lapenta, Department of Dermatology and Post graduated from Carabobo University, Researcher, Venezuela; Website: www.dermagicexpress.blogspot.com
Citation
Lapenta, J. Tick Paralysis. (2017) Invest Dermatol Venereol Res 3(2): 117- 119.
Copy rights
© 2017 Lapenta, J. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Introduction
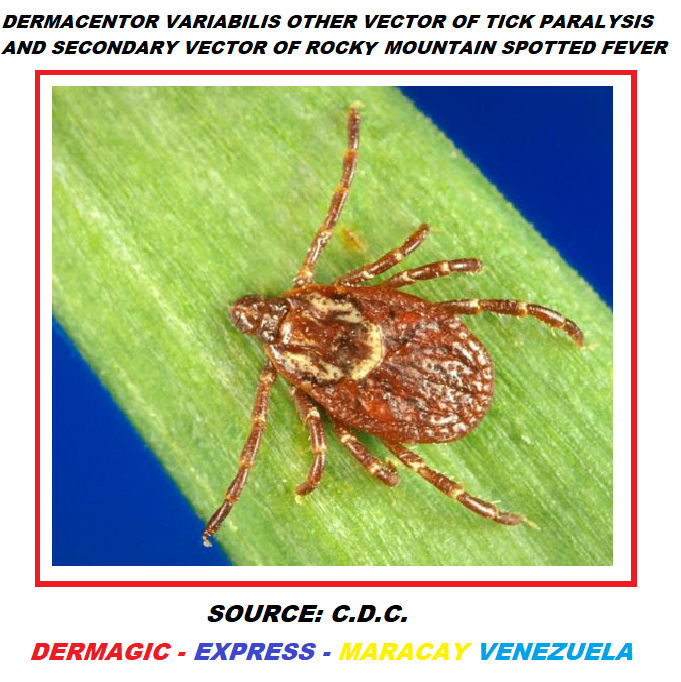
The Tick Paralysis is now considered an Envenoming Neurotoxic which is similar to polio, affects both children and adults (majority children) especially in regions considered Hyperendemic as the West of the United States and the regions of Eastern Australia. Historically, the Australians Hamilton Hume and William Hove described the first bites of Ticks To Humans in 1824, but it was Bancroft in 1.884 the first to report two cases (2) of toxicosis by Ticks To Humans describing 2 cases with weakness and blurred vision. The first death was reported by Cleland in 1912. Since that time the disease has been reported almost everywhere in the world. [Dermacentor Variables, other vector of Tick Paralysis and secondary vector of the Rocky Mountain spotted fever]
This disease is considered a rare condition, but very well studied by our scientists, and begins with the transmission of a Neurotoxin that is in the salivary glands of the Female ticks that when feed with blood enter to the bloodstream causing the symptoms which are characterized by a Ascending Flaccid Paralysis of the muscles that begins 2 to 7 days after the bite, in the lower limbs, and then goes up to the trunk, arms, head and death can occur due to respiratory failure. Other symptoms include numbness, decreased tendon reflexes, ophthalmoplegia, and bulbar palsy.
The Tick Paralysis (TP) can be misdiagnosed, and confuse medical science with entities such as: Acute Ataxia, Transverse Myelitis, Epidural Abscess, Botulism And Gullain Barre Syndrome (GBS), the latter being the one that lends itself most to confusion.
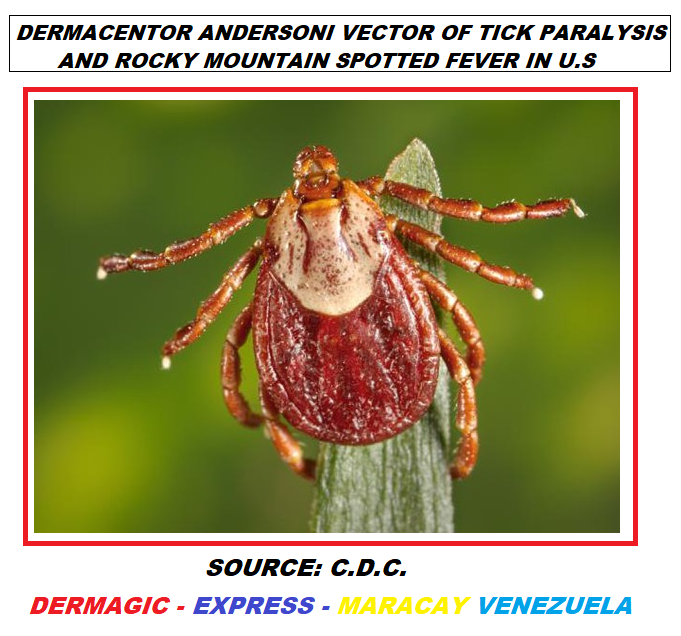
The causative agents of this condition are fully identified: In the United States of America, the vector is the Tick Dermacentor Andersoni, which also transmits the Disease the Rocky Mountains Spotted Fever. Another causative agent of this disease is the Tick Dermacentor Variables, considered the second most frequent vector in the transmission of The Rocky Mountains Spotted Fever.
Figure 1:
Figure 2:
But this does not stop here; Approximately 69 species of Ticks from all over the world are able to induce Paralysis by Bitting. In other countries, such as the southeast of Australia, this disease (TP) is also endemic and the causative agents are other Ticks, among which the Tick of the Ixodes genus, Ixodes Holocyclus, and Ixodes Cornuatus, also Dermacentor Andesoni and Variables stand out. [Tick Ixodes Holocyclus, Vector of Tick Parslysis in Australia.]
In South Africa the most important vector is the Tick Ixodes Rubicundus, in Ethiopia, the Ticks Rhipicephalus Evertsi Evertis and Argas Walkerae and Tick Argas Radiatus in the Neartic region of North America.
The disease considered as a global extension “Supposedly” has not been described in the Hemisphere Sur, but in the year 1994, two (2) cases were described in Argentina in the province of Jujuy. A case (1) was also described on the Pacific coast of Mexico, produced by the Tick Amblyoma Maculatum.
It has also been reported in The British Columbia, the third most populated province of Canada, 57 cases between 1993 and 2016 being the most common vector the Tick Dermacentor Andersoni, the cases were found in both humans and animals.
Ticks Paralysis has also been described in animals such as: cats, dogs, cattle horses, sheep, and birds, being the Tick Ixodes Holocyclus the most involved. In fact, today this disease in Australia is considered a veterinary problem because of the large number of infected animals, and the main host of this is the mammal Long-Nosed-Bandicoot. [Long-noses-bandicoot mammal, most common host from Ixodes Holocyclus, Vector of Tick Parslysis in Australia.]
Figure 3:
Figure 4:
Unlike other diseases such as Lyme, Powassan and Heartland Disease, where the Tick involved Transmits a bacterium (Lyme) or virus (Powassan and Heartland) that infects the organism, in the case of Tick Paralysis (TP) it is a Neurotoxin that only remains in the organism While The Tick Is Adhered to the Skin Feeding With Blood, when taking it off the symptoms gradually disappear recovering the patient, even though the Lethality is of 10 - 12%.
Conclusion
So that I describe another disease Transmitted By Ticks, and I leave you the same reflection of my other reviews, the best way to Avoid Them, is not only to fight for human rights to receive adequate treatment Like The Case Of Lyme Disease, which have been Violated in many countries, especially in the US, we also have to fight against Vectors and Hosts.
References
1) Morshed, M., Li, L., Lee, M.K., et al. A Retrospective Cohort Study of Tick Paralysis in British Columbia. (2017) Vector Borne Zoonotic Dis 17(12): 821-824.
2) Diaz, J.H. A comparative meta-Analysis of tick paralysis in the United States and Australia. (2015) Clin Toxicol (Phila) 53(9): 874-883.
3) Diaz, J.H. A 60-year meta-analysis of tick paralysis in the United States: a predictable, preventable, and often misdiagnosed poisoning. (2010) J Med Toxicol 6(1): 15-21.
4) Edlow, J.A., McGillicuddy, D.C. Tick paralysis. (2008) Infect Dis Clin North Am 22(3): 397-413.
5) Remondegui, C. Tick paralysis cases in Argentina. (2012) Rev Soc Bras Med Trop 45(4): 533-534.
6) Taraschenko, O.D., Powers, K.M. Neurotoxin-induced paralysis: a case of tick paralysis in a 2-year-old. (2014) Pediatr Neurol 50(6): 605-607.
7) Gordon, B.M., Giza, C.C. Tick paralysis presenting in an urban environment. (2004) Pediatr Neurol 30(2): 122-124.
8) Dworkin, M.S., Shoemaker, P.C., Anderson, D.E. Tick paralysis: 33 human cases in Washington State. (1999) Clin Infect Dis 29(6): 1435-1439.
9) Cluster of tick paralysis cases--Colorado, 2006. (2006) MMWR Morb Mortal Wkly Rep 55(34): 933-935.
Pubmed || Crossref || Others
10) Brazier, I., Kelman, M., Ward, M.P. The association between landscape and climate and reported tick paralysis cases in dogs and cats in Australia. (2014) Vet Parasitol 204(3-4): 339-345.
11) Whitfield, Z., Kelman, M., Ward, M.P. Delineation of an endemic tick paralysis zone in southeastern Australia. (2017) Vet Parasitol 247: 42-48.
12) Barker, S.C., Walker, A.R., Campelo, D. A list of the 70 species of Australian ticks; diagnostic guides to and species accounts of Ixodes holocyclus (paralysis tick), Ixodes cornuatus (southern paralysis tick) and Rhipicephalus australis (Australian cattle tick); and consideration of the place of Australia in the evolution of ticks with comments on four controversial ideas. (2014) Int J Parasitol 44(12): 941-953.
13) Espinoza-Gomez, F., Newton-Sanchez, O., Flores-Cazares, G. Tick paralysis caused by Amblyomma maculatum on the Mexican Pacific Coast. (2011) Vector Borne Zoonotic Dis 11(7): 945-946.
14) Tick Paralysis — Washington, 1995. (1996) MMWR Morb Mortal Wkly Rep 45(16): 325-326.
15) Pek, C.H., Cheong, C.S., Yap, Y.L., et al. Rare Cause of Facial Palsy: Case Report of Tick Paralysis by Ixodes Holocyclus Imported by aPatient travelling into Singapore from Australia. (2016) J Emerg Med 51(5): e109-e114.
16) Hall-Mendelin, S., Craig, S.B., Hall, R.A., et al. Tick paralysis in Australia caused by Ixodes holocyclus Neumann. (2011) Ann Trop Med Parasitol 105(2): 95-106.