Hypereosinophilia-and-Intraoperative-Complications-under-General-Anesthesia-in-Surgical-Patients-Aged-12-Years-or-More-an-Observation
Affiliation
Assistant Professor, Department of Anaesthesiology, Andaman and Nicobar Islands Institute of Medical Sciences & GB Pant, Hospital, Port Blair, India
Corresponding Author
Habib Md Reazaul Karim, Department of Anaesthesiology, ANIIMS and GB Pant Hospital, Port Blair, India,744104, Tel: +919612372585; E-mail: drhabibkarim@gmail.com
Citation
Karim, H.M.R., et al. Hypereosinophilia and Intraoperative Complications under General Anesthesia in Surgical Patients Aged 12 Years or More: an Observation. (2017) J Anesth Surg 4(2): 82- 85.
Copy rights
© 2017 Karim, H.M.R. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Eosinophils; Eosinophilia; Anesthesia; Adult; Hypereosinophilic syndrome
Abstract
Background: Hypereosinophilia (HE) is a relatively commoner and previously has been shown to be associated with several adverse effects in intraoperative and immediate postoperative period in anesthetic practice. However, recent scientific literature in this aspect is very scarce.
Aim: The present study was aimed to assess the frequency of HE and incidences of notable intraoperative adverse events in such patients.
Methods: The present study was conducted in a tertiary care teaching hospital during December 2016 to June 2017. Files of all patients aged 12 years and more attending preanesthetic evaluation clinic was screened for the presence of HE. Anesthetic management of these patients was then observed and adverse events like respiratory spasms, urticaria, drug reactions etc noted. Data were presented in absolute numbers and percentage scale. INSTAT software was used for statistical analysis purpose.
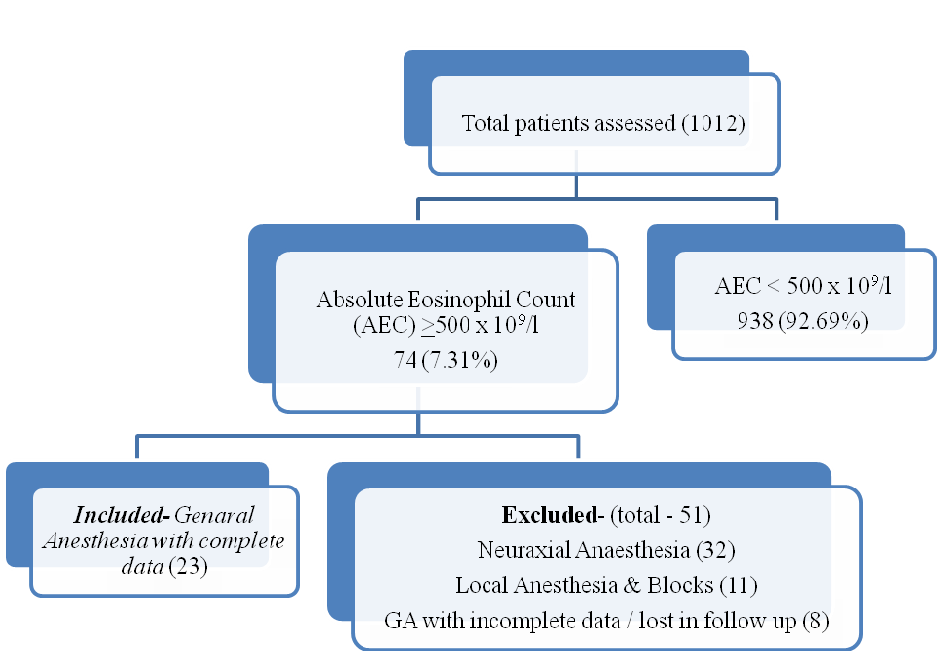
Results: A total of 1012 patients were included; 74 (7.31%) were having absolute Eosinophil counts (AEC) > 500 x 109/l. Eosinophilia was more among male (58.11%) and significantly more frequent in children than adults (17.39% versus 6.83%; p 0.015). The AEC of hypereosinophilic patients ranged from 502 to 4030 × 109/l. Medicine consultation was taken in two cases while six cases were prescribed antihelminthic and antihistaminic drug by anesthesiologist in preoperative period. The treatment was effective in reducing AEC by an average of 1191.5 × 109/l. Twenty three out of 27 patients who were managed with general anesthesia were observed for HE related complication. No notable complication attributable to HE was found.
Conclusion: HE is very common even in adult surgical patients, mostly asymptomatic and idiopathic; HES is however rare. Deworming and antihistaminic treatment was effective in reducing AEC in patients with marked HE. GA with currently used agents appear to be safe and without much adverse effects (if any) in hypereosinophilic patients.
Introduction
Eosinophil mediates parasite defense reactions, allergic response, tissue inflammation, and immune modulation in our body[1]. They ingest antigen-antibody complexes and releases vasoactive mediators like leukotrienes, histamines etc. these vasoactive materials are well known for provoking hypersensitive reactions which clinically manifests as spasms of respiratory systems, desaturation, urticaria and may even show profound fall of blood pressure and cardiovascular effects. Therefore hypereosinophilic patients are an important concerning group for anesthesiologists. Studies showed that hypereosinophilic patient experienced more bronchospasm, urticaria, rigors at the time of induction and reversal of anaesthesia[2]. Many of the anaesthetic drugs used in general anaesthesia is also known to induce histamine release / hypersensitivity[3]. Drug rash with eosinophilia and systemic symptoms (DRESS) has been described in anesthetic practice in recent period too[4]. However there is relative lack of data to show the extent of the problem. With the routine use of safer drugs in anesthetic practice, adverse reactions or events with anaesthetic drugs in hypereosinophilic patient may have been reduced to a great extent. The present study was therefore aimed to assess the frequency of hypereosinophilia and incidences of notable intraoperative adverse events in older childrens and adult patients. The preoperative impact of hypereosinophlia in anaesthesiologists’ decision making was also observed.
Methods
The present study was conducted by analyzing the data bank which was collected by the author for assessing the ‘impacts of abnormal routine preoperative test results in perioperative anesthetic management’ after obtaining the approvals from the institute. These data were collected prospectively during December 2016 to June 15, 2017. All patients aged 12 years and above, of either sex attending preanaesthesia evaluation clinic (PAEC) for planned elective surgeries were screened for data collection. Legally protected tribal population as per local law, pregnant women, bedridden or immobile patients whose body weight could not be assessed were excluded. Patients’ demographic parameters, grade of surgery as per adapted NICE classification, ASA physical status, etc were noted. Presence of hypereosiniphilia (HE) was noted both as per local reference and definition. Eosinophil differential count of 1 - 6% was normal and number of patients with Eosinophil differential count > 7 % was also calculated. In the study, HE was however calculated as per Absolute Eosinophil Counts (AEC) criteria (definition) in which AEC > 500 x 109/l was considered for analysis[5]. No intervention was done by the data collector to modify the PAEC process. History of allergy, atopy, asthma, drug reactions, elephantiasis (if any) were also noted. The responses of anaesthesiologists to the eosinophilia were noted. The cases were further followed up for noting any presence of intraoperative bronchospasm, skin reactions or any adverse events attributable to hypereosinophilia. The drug management for general anaesthesia was also noted. Qualitative data are presented in absolute numbers and percentage scale. Metric data were analyzed for measuring central tendencies and dispersions using INSTAT software (GraphPad Prism Software, La Zolla, CA, USA).
Results
A total of 1012 patients {470 (46.44 %) male and 542 (53.56 %) female} file were screened. Eighty (7.91 %) patients were having Eosinophil differential counts > 7 % but 74 (7.31 %) patients AEC was > 500 × 109/l. Out of 1012, 17 (1.68 %) patients were having AEC > 1500 × 109/l. The median age of eosinophilic patients (AEC > 500 × 109/l) was 46 (range 12 – 75) year. The demographic data, ASA and NICE surgical grade data are presented in Table 1.
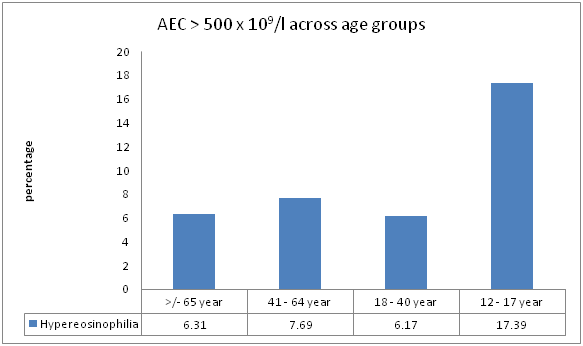
The AEC of eosinophilic patients ranged from 502 to 4030 × 109/l with mean ± standard deviation AEC count of 1209.55 ± 679.5 × 109/l. Among the patients with incidental eosinophilia, 57 (77.03%) patients were having mild eosinophilia (AEC up to 1500 × 109/l) while 17 (22.97%) were having marked eosinophilia (AEC > 1500 × 109/l). The frequency of eosinophilia were higher among older children (i.e 12 – 17 years) as compared to adults (i.e 18 years and more) {17.39 % versus 6.83 %; relative risk (95 % confidence): 2.545 (1.30 – 4.98); p 0.015}. The distributions of eosinophilia across the different age groups are presented in figure 1.
Table 1: Demographic, physical status and surgical category wise distribution of the patients with Absolute Eosinophil Count > 500 x 109/l. (n – number, SD – standard deviation, ASA – American Society of Anesthesiologists, NICE – National Institute for Health and Care Excellence, IQR – inter quartile range, BMI – body mass index).
| Parameters | n (%) |
|---|---|
| Male | 43 (58.11) |
| Female | 31 (41.89) |
| Age (year) mean ± SD | 43.12 ± 17.47 |
| Weight (kg) mean ± SD | 55.83 ± 11.36 |
| ASA physical status in median (IQR) | 2 (2 – 2) |
| I | 17 (22.97) |
| II | 44 (59.46) |
| III | 12 (16.22) |
| IV | 1 (1.35) |
| V | 0 |
| NICE surgical grade in median (IQR) | 2 (1 – 3) |
| 1 | 34 (45.96) |
| 2 | 20 (27.02) |
| 3 | 20 (27.02) |
| 4 | 0 |
| BMI > 30 Kg/m² | 1 (1.35) |
Figure 1: Frequency of eosinophilia among different age groups in studied cohort. (AEC – absolute Eosinophil counts).
Medicine (physician) consultation for evaluation was taken in 2 (2.70 %) case. Six (8.11 %) cases was prescribed antihelminthic drug along with antihistaminic by anesthesiologist with an advice to repeat AEC after the course. The treatment reduced the AEC ranging between 482 – 1995 × 109/l (average 1191.5 × 109/l). History and laboratory findings suggestive of systemic involvements were nearly none and presented in Table Out of the 74 patients, 27 were managed with general anesthesia for their elective surgeries; 23 were included for observational analysis. The sampling tree is presented in flow diagram below.
Table 2: Clinical and laboratory parameter abnormalities in patients with Absolute Eosinophil Count > 500 x 109/l). (n – Number, ECG -electrocardiogram)
| Parameters [N – total number assessed] | n (%) |
|---|---|
| Allergy, Atopy, Asthma (history) [74] | 2 (2.70) |
| Known case of Filariasis | 0 |
| Feature of heart failure (clinical) [74] | 0 |
| Low platelets (< 1 lac x 109/l) [74] | 0 |
| Abnormal coagulation tests [14] | 0 |
| Deranged liver function test [52] | 7 (13.46) |
| Unexplained arrhythmia in ECG [65] | 0 |
| Pneumonitis in chest x-ray [64] | 0 |
| Anemia [74] | 16 (21.62) |
| Leucocytosis [74] | 1 (1.35) |
The mean ± SD age of the patient who were managed with GA was 36.86 ± 18.84 (range 13 – 70) years. They had mean ± SD AEC of 1442.4 ⊕ 906.4 x 109/l (range 548 – 4030 x 109/l). None of the patient had notable bronchospasm, laryngospasm, skin manifestions during intubation, maintenance and extubation which were attributable to HE.
Discussion
The normal eosinophil count in the peripheral blood ranges from 50 to 500 × 109/l. Blood eosinophilia can be divided into mild eosinophilia (up to 1500 × 109/l) and marked eosinophilia (>1500 × 109/l)[5]. HE may be present in variety of conditions like infections (especially helminthic parasites), allergic responses, neoplasms, connective tissue disorders, medications, endocrinopathies etc[5]. HE may present as DRESS, chronic dry cough, and even manifest with cardiovascular signs and symptoms[4,6,7]. However, most of the time HE is asymptomatic and incidental finding in routine complete blood counts. Although exact history of parasitic infestation could not assessed in present study; only 2 (2.70 %) of patients were having history of allergy, atopy and asthma. Even if we exclude these two cases, rest (97.30 %) patients could be regarded as asymptomatic / accidental finding.
Eosinophilia is very common abnormality and is found more in children. A retrospective study from India found that 29 % of patients who underwent cleft lip and palate repair under smile train project had eosinophilia[8]. The present study also showed that eosinophilia was higher among children aged between 12 – 17 years as compared to adults. The lower frequency of eosiniphilia in the present cohort is probably because the present cohort did not have children below 12 years. The incidence of eosinophilia and HE however is variable from place to place and the finding of the present study may not well represent global data. A Korean study found 12.2 % patient to have eosinophilia but only 0.9 % was found to have HE[9]. Although the frequency of eosinophilia in the present study was lower than the Korean study, the frequency of HE was nearly double (i.e. 1.68 %) in the present study. On the other hand, a study done in Copenhagen found only 4% eosinophilia which is lower than the present study[10]. Another multicentre retrospective analysis from United States found eosinophilia in 6 % patients as incidental finding[11].
Anesthesiologists are concerned with marked HE because of the fact that Eosinophil degranulation releases vasoactive mediators which can affect respiratory, cardiovascular as well as hematologic system. Long term HE can do tissue damage. Moreover marked HE may be a part of hypereosinophilic syndrome (HES) which has diverse clinical manifestations due to associated end organ damages[12]. Complications like life-threatening acute respiratory distress syndrome following GA in HES patient have also been reported[13]. Many syndromes are also associated with HE[12]. Recognition of such cases is important for proper evolution, risk stratification and anaesthetic plan and management. Patients with HES must have basal neurologic examination done. Evaluation of cardiac dysfunction and arrhythmia by electrocardiography and echocardiography, review baseline CXR, complete blood cell blood count, and liver function should also be done preoperatively[12]. In the present cohort 17 patients had marked HE; 7 had AEC > 2000 x 109/l and none had symptoms and signs suggestive of end organ damage. It was observed that 6 out of 7 patients who had AEC > 2000 x 109/l were prescribed medication for deworming (tablet albendazole) for one day and antihistaminic (tablet levocetrizine) for 5 days as per institutional protocol and it was found to be effective in reducing AEC although most of them still remained in marked HE range. Helminthic infections / infestations are the most common cause of marked eosinophilia worldwide[14]. These infections / infestations are more prevalent in developing and poor socioeconomic countries. Moreover, allergy is a well cause of eosinophilia[5]. Considering these a dose of antihelminthic and antihistaminic were prescribed in patients with marked eosinophilia. Only two cases were thought that AEC may not be idiopathic and medicine evaluation was requested; one was associated with leucocytosis. However, both the case turned out to be idiopathic HE. Although 7 patients had slight deranged alkaline phospahatase and mild elevation of bilirubin, two of them were regular alcohol user and none of them actually indicated any significant liver damage / failure. Thus not a single patient was suspected to have HES. This is probably because HES is extremely rare disease with the crude incidence of HES 0.035 per 100,000[15].
The major anaesthetic drug used for GA were injection Propofol (all 23 cases), Fentanyl (in 21 cases), Morphine (in 3 cases), Vecuronium (in 22 cases), succinyl choline (in 2 cases), atracurium in one case. Sevoflrane was used in 19 out of 23 while rest cases were maintained with Isoflurane. None of the patient had any clinically evident intraoperative drug reaction and bronchospasm.
The present study was however limited with the fact that it was observational in nature and the number of patient who underwent GA was less. Yet, absence of any adverse events attributable to HE in 23 cases indicate that, it is rare in older children and especially in adult patients with idiopathic HE.
Conclusion
Eosinophilia and HE are very common even in adult surgical patients of our set up, mostly asymptomatic and idiopathic; HES is however rare. Deworming and antihistaminic treatment was effective in reducing AEC in patients with marked HE. Anesthesiologist should be however alert to find HES among marked HE patients; history and clinical examination can help. GA appears to be safe and without much adverse effects (if any) in older children and adult surgical patients with HE.
Conflict of interest:
The authors declare no conflict of interest.
References
- 1. Gotlib, J. Molecular classification and pathogenesis of eosinophilic disorders: 2005 update. (2005) Acta Haematol 114: 7-25.
Pubmed || Crossref || Others - 2. Gurnani, A., Jain, A., Bhattacharya, A. Anaesthetic problems in eosinophilia: preliminary report. (1991) J Anaesthesiol Clin Pharmacol 7: 205-208.
Pubmed || Crossref || Others - 3. Walkins, J. Investigation of Allergic and Hypersensitivity reactions to anaesthetic agents. (1987) Br J Anaesth 59(1): 104-111.
Pubmed || Crossref || Others - 4. Bansal, S., Bassi, R., Tripathi, N. Eosinophilia in Preanaesthetic Assesment: A guide to diagnose DRESS syndrome. (2013) J Anaesth Clin Pharmacol 29(2): 270-271.
Pubmed || Crossref || Others - 5. Valent, P., Gleich, G.J., Reiter, A., et al. Pathogenesis and classification of eosinophil disorders: a review of recent developments in the field. (2012) Expert Rev hematol 5(2): 157-176.
Pubmed || Crossref || Others - 6. Kobayashi, M., Kubota, T., Uemura, Y., et al. A case of hypereosinophilic syndrome presenting with chronic cough successfully treated with imatinib. (2009) Respirology 14(2): 302-304.
Pubmed || Crossref || Others - 7. Ogbogu, P., Rosing, D.R., Horne, M.K. Cardiovascular Manifestations of Hypereosinophilic Syndromes. (2007) Immunol Allergy Clin North Am 27: 457-475.
Pubmed || Crossref || Others - 8. Jindal, P., Khurana, G., Gupta, D., et al. A retrospective analysis of anesthetic experience in 2917 patients posted for cleft lip and palate repair. (2013) Anesth Essays Res 7: 350-354.
Pubmed || Crossref || Others - 9. Kim, D.W., Shin, M.G., Yun, H.K., et al. [Incidence and causes of hypereosinophilia (corrected) in the patients of a university hospital]. (2009) Korean J Lab Med 29(3): 185-193.
Pubmed || Crossref || Others - 10. Andersen, C.L., Siersma, V.D., Hasselbalch, H.C., et al. Association of the blood eosinophil count with hematological malignancies and mortality. (2015) Am J Hematol 90: 225-229.
Pubmed || Crossref || Others - 11. Ogbogu, P.U., Bochner, B.S., Butterfield, J.H., et al. Hypereosinophilic syndromes: A multicenter, retrospective analysis of clinical characteristics and response to therapy. (2009) J Allergy Clin Immunol 124: 1319–1325.
Pubmed || Crossref || Others - 12. Bissonnette, B., Luginbuehl, I., Merciniakm, B., et al. Hypereosinophilic syndrome. In: Syndromes- Rapid Recognition and Perioperative Implications. (2006) 1st edition New York McGraw Hill 395.
Pubmed || Crossref || Others - 13. Cho, H.R., Han, S.J., Kwon, Y.E., et al. Anesthetic Management of a Patient with Idiopathic Hypereosinophilic Syndrome - A case report. (2007) Korean J Anesthesiol 52: 728-732.
Pubmed || Crossref || Others - 14. Nutman, T.B. Evaluation and differential diagnosis of marked, persistent eosinophilia. (2007) Immunol Allergy Clin North Am 27: 529-549.
Pubmed || Crossref || Others - 15. Crane, M.M., Chang, C.M., Kobayashi, M.G., et al. Incidence of myeloproliferative hypereosinophilic syndrome in the United States and an estimate of all hypereosinophilic syndrome incidence. (2010) J Allergy Clin Immunol 126(1): 179-181.
Pubmed || Crossref || Others