Relationship between initial high-sensitivity cardiac troponin-T morbidity and mortality in patients after ST-elevation Myocardial Infarction in Erbil City, Iraq
Hewa M.H. Ameen1, Mohammed H. Alwan1, Nicola King2*
Affiliation
1Hawler Medical University, Medical College, Department of Medicine, Erbil City, Iraq
2School of Biomedical Sciences, Faculty of Health: Medicine, Dentistry and Human Sciences, University of Plymouth, Plymouth, PL4 8AA. UK
Corresponding Author
Nicola King, School of Biomedical Sciences, Faculty of Health: Medicine, Dentistry and Human Sciences, University of Plymouth, Plymouth, PL4 8AA, UK, Fax: +44 (0)1752 586788, Telephone: +44 (0)1752 584969; Email: Nicola.king@plymouth.ac.uk
Citation
Ameen H.M.H., et al. Relationship between Initial High-Sensitivity Cardiac Troponin-T Morbidity and Mortality in Patients after ST-Elevation Myocardial Infarction in Erbil City, Iraq. (2019) J Heart Cardiol 4(2): 28-33.
Copy rights
© 2019 King, N. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
hs-cTnT; STEMI; PPCI; Mortality; Morbidity
Abstract
Background: ST-segment elevation myocardial infarction (STEMI) patients treated with primary percutaneous intervention (PPCI) are at a high risk of death and MACE (Major Adverse Cardiovascular Events). One method to stratify these patients’ risk could be high-sensitivity cardiac troponin-T (hs-cTnT). Unfortunately; data using this approach is limited. The aim of this study was to investigate whether there is a correlation between initial levels of cTnT in STEMI patients with MACE.
Methods: Initial hs-cTnT levels were measured in 167 patients with STEMI undergoing PPCI. Patients were divided into 2 groups: group A hs-cTnT below the median (83 patients); group B hs-cTnT above the median (84 patients). Patients were followed up for 2 years investigating mortality and MACE.
Results: The median value of initial hs-cTnT was 100 ng / L. The mean hs-cTnT was 52 ± 26 ng / L in group A and 548 ± 458 ng / L in group B. 18 (10.8%) patients died during follow-up:13 (15.5%) in group B compared to only 5 (6%) ingroup A (P < 0.05). Further analysis showed that non-surviving patients were older, more likely to be female, had more diabetes mellitus, more hypertension, and more diffuse coronary artery disease. They also had worse outcomes such as heart failure, increased rates of recurrent chest pain, readmissions and other infrequent complications such as complete heart block, renal impairment, reinfarction, stent thrombosis, and upper gastrointestinal tract bleeding.
Conclusions: Increased initial hs-cTnT levels are associated with a higher risk of mortality and morbidity at 2-year follow up in patients from Erbil with STEMI undergoing PPCI.
Introduction
It is estimated that ischemic heart disease will be the number one cause of disability and death worldwide by the year 2020[1]. Almost all cases result from coronary thrombosis following the erosion or rupture of an atherosclerotic lesion[2]. With the occlusion of the coronary blood flow ST segment elevation occurs on the electro cardiogram (ECG) and impaired myocardial perfusion causes ischemia that may result in myocardial cell death or injury, cardiac arrhythmias, and ventricular dysfunction. Within 15 minutes of occlusion myocardial cell death begins and rapidly proceeds from the endocardium to the epicardium in a wave front. Partial Salvage of the myocardium can be achieved by restoration of the blood flow within 3 to 6 hours, with the degree of salvage and the duration of ischemia being inversely proportional[3].
The increasing sensitivity of cardiac biomarkers means that clinicians can detect lower levels of injury, but this does not provide information on the cause of the damage[4]. The cardiac biomarker of choice to detect myocardial injury is cardiac troponin. Following cardiomyocyte injury, the initial release of cTnT is from the cytosolic pool, (6 – 8% of cTnT dissolved in the cytosol). This is later followed by the release of myofilament bound protein[5]. The cornerstone of the diagnostic criteria for myocardial infarction (MI) is detection of a rise and fall in cTnT or cTnI[6], which occurs approximately 3 hours after the onset of chest pain by conventional assays (non–high-sensitivity)[7]. cTnT continues to be released from necrotic cardiomyocytes as the contractile apparatus degenerates. This causes persistent elevations of up to 10-14 days in cTnT after MI[8], which can be helpful for late diagnosis of MI. Successful recanalization of the infarct-related artery also induces a rapid release of cardiac troponins, which may indicate reperfusion. With high-sensitivity assays (hs-cTn) there is more precise measurement of very low concentrations of cardiac troponin leading to assays which are capable of detecting cTnT in more than 50% of the healthy population[5,6, 9]. Ndrepepa et al.,[10] divided circulating hs-cTnT into 4 fractions according to the time of measurement in patients with ST segment elevation myocardial infarction (STEMI) who were undergoing primary percutaneous coronary intervention (PPCI). The first fraction is caused by physiological cardiomyocyte turnover[11]. The second fraction is due to enhanced cardiomyocyte stress by many abnormal stimuli which cause leakage of troponin through multiple mechanisms[12]. The third fraction is from acute myocardial ischemia/necrosis in patients presenting with an acute coronary syndrome (ACS). For example in the early phase of STEMI where detection of troponin I correlates closely with infarct size[13] and mortality[14]. The fourth fraction relates to PPCI complications and correlates with a poor outcome[15]. The aim of this study was to determine if hs-cTnT measurements performed during initial admission to hospital of patients with STEMI about to undergo PPCI can predict long-term mortality and major adverse cardiovascular events (MACE).
Methods
Ethical approval
The study was approved by the local ethical committee of the Kurdistan Board of Medical Specialties. All patients involved in the study gave written informed consent.
Patients
This study was a prospective review of patients with STEMI who were admitted to the surgical specialty hospital / cardiac center in Erbil city (Iraq) from January 2017 to June 2017 and who later underwent successful PPCI. This included cases referred from other hospitals. Patients were admitted to the coronary care unit (CCU), where they immediately had a standard 12 lead ECG taken. The criteria used for ST elevation was based on criteria from The European Society of Cardiology, American College of Cardiology, American Heart Association, and the World Heart Federation. Thus, new ST elevation at the J point in two contiguous leads with the following cut off points: ≥ 0.1 mV in all leads (except V2-V3), in leads V2-V3 the following cut points apply: ≥ 0.2 mV in men ≥ 40 years, ≥ 0.25 mV in men < 40 years, And ≥ 0.15 mV in women[16]. Using this criteria 225 patients were enrolled in this study to be followed up for 2 years. Unfortunately contact was lost with 58 patients during follow up. Patients were excluded if they had been diagnosed with chronic renal failure, presented with cardiogenic shock or pulmonary odema, or underwent emergency coronary artery bypass graft. Patients were also excluded if they had a severe comorbidity such as chronic obstructive pulmonary disease, liver or neurological diseases.
Procedures
After obtaining informed consent from patients or their relatives, a detailed history and clinical examination were collected for every patient within the first 24 hours of their admission to the CCU. This mainly concentrated on clinical presentation and the arrival time of the patient to the CCU from the start of the symptoms. In addition, risk factors such as hypertension, diabetes mellitus, smoking, hyperlipidemia, previous ischemic heart disease, and a positive family history were noted. ECG changes were used to locate the site of the MI depending on the presence of ST elevation and / or hyperacute T waves and development of Q waves in certain leads. All medications administered to the patient were recorded including antiplatelet, anticoagulation and thrombolytic therapy. A peripheral venous blood sample was taken at initial admission for hs-cTnT, creatine kinase-muscle-brain band, complete blood picture, erythrocyte sedimentation rate, blood sugar, blood urea, serum creatinine and lipid profile. The plasma concentration of cTnT was measured using the high sensitivity assay by a Cobas e411 immunoanalyzer based on electrochemiliuminescence technology (Roche Diagnostics) with the assay performed according to the manufacturer’s instructions (detection limit of 5 ng / L, 99th percentile in the general population of 14 ng / L and 10% coefficient of variation level of 13 ng /L).
Interventions were performed according to global and local guidelines (STEMI within first 24 hours, or persistent chest pain or heart failure within 48 hours), and the decision for PPCI was made by the interventional cardiologist on duty. All patients underwent PPCI with an oral loading dose of 180 mg of ticagrelor plus aspirin 300mg at time of admission. During the procedure, intravenous heparin was administered; the use of glycoprotein IIb / IIIa inhibitors was at the discretion of the operator, drug-eluting stents were used for PPCI. After the intervention, all patients were prescribed 100 mg / day of aspirin indefinitely, ticagrelor 90 mg twice per day for 12 months, and other cardiac medications at the discretion of the patient’s physician. Within 1-2 days of admission a doppler echocardiography was arranged for most patients.
Endpoints
Patients were followed up for up to 20 to 24 months (median 22 months) after STEMI. The primary endpoint of interest in this study was all-cause mortality. The secondary endpoint was other MACE including heart failure, reinfarction, readmission, and the need for further revascularization. Information on deaths was obtained from hospital records or telephone contact with relatives of the patient. Arterial hypertension was diagnosed in the presence of active treatment with antihypertensive agents or otherwise as a systolic blood pressure of ≥ 140 mm Hg and / or diastolic blood pressure of ≥ 90 mm Hg on at least 2 separate occasions[17]. Diabetes mellitus was diagnosed in the presence of active treatment with antidiabetic agents or based on current guidelines[18]. Heart failure was diagnosed according to modified Framingham clinical criteria for the diagnosis of heart failure[19]. The infarct related artery is the coronary artery containing the culprit lesion which presented as an acute occlusion, intraluminal filling defect or thrombus, ulcerated plaque with contrast-filled pocket protruding into the plaque with or without delayed contrast wash-out, dissection, extraluminal contrast, or intraluminal flaps[20,21]. PPCI success was defined as TIMI III flow across the culprit lesion and less than 30% residual stenosis[22].
Data Analysis
According to initial admission hs-cTnT levels patients were divided into two groups: first group less than the median value (group A) and second group more than the median (group B). A further analysis was carried out according to the survival status of the patients. The computer software SPSS v.25 for windows was used to analyze the data. Chi2 test was used for categorical variables to determine the significance of any difference for any observed feature between the two groups. Continuous data is expressed as mean ± SD. A p value < 0.05 was considered significant.
Results
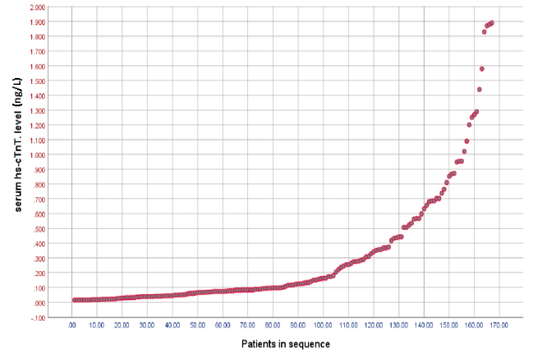
A total of 167 patients were included in this study. The median value of initial hs-cTnT was 100 ng / L. Using this value the patients were divided into 2 groups. Group A (83 patients) patients with hs-cTnT measurements below the median, range 14-98 ng / L, mean 52 ± 26 ng / L. Group B (84 patients) patients had hs-cTnT measurements above the median, range 100-1890 ng / L, mean 548 ± 458 ng / L. The distribution chart of patients according to their levels of serum hs-cTnTis shown in figure 1.
Figure 1: distribution of patients according to hs-cTnT levels. Patients are ranked in order of ascending hs-cTnT levels.
Overall, patient ages ranged from 29-87 years with a mean of 57.5 ± 11.1 years and there were more males than females. These and other baseline characteristics compared between the 2 groups are shown in table 1. There was no significant differences in age categories, gender, incidence of hypertension, smoking status, infarct related artery and number of vessels affected between the 2 groups. However, proportionately more patients in group B had diabetes mellitus.
Table 1: clinical characteristics of patients.Baseline clinical characteristics of the patients grouped according to whether their initial hs-cTnT was above (group A) or below (group B) the median. HTN: hypertension; DM: diabetes mellitus; LAD: left anterior descending; RCA: right coronary artery; LCX: left circumflex.
|
|
|
Group A |
Group B |
Total |
p value |
|
Age categories (in years) |
20-39 |
6(7.2%) |
6(7.1%) |
12(7.2%) |
0.405 |
|
40-59 |
42(50.6%) |
33(39.3%) |
75(44.9%) |
||
|
60-79 |
34(41%) |
42(50%) |
76(45.5%) |
||
|
80-90 |
1(1.2%) |
3(3.6%) |
4(2.4%) |
||
|
Gender |
Female |
17(20.5%) |
21(25%) |
38(22.8%) |
0.486 |
|
Male |
66(79.5%) |
63(75%) |
129(77.2%) |
||
|
DM |
|
16(19.3%) |
37(44%) |
53(31.7%) |
0.001 |
|
HTN |
|
29(34.9%) |
35(41.7%) |
64(38.3%) |
0.371 |
|
Current Smoker |
|
30(36.1%) |
29(34.5%) |
59(35.3%) |
0.827 |
|
Infarct related artery |
LAD |
44(53%) |
48(57.1%) |
92(55.1%) |
0.410 |
|
RCA |
32(38.6%) |
33(39.3%) |
65(38.9%) |
||
|
LCX |
7(8.4%) |
3(3.6%) |
10(6.0%) |
||
|
Number of vessels affected |
Single vessel |
31(37.3%) |
24(28.6%) |
55(32.9%) |
0.475 |
|
Two vessels |
26(31.3%) |
31(36.9%) |
57(34.1%) |
||
|
Three vessels |
26(31.3%) |
29(34.5%) |
55(32.9%) |
Table 2: Survival status in both groups. The number of living and dead patients grouped according to whether their hs-cTnT was above or below the median.
|
|
|
Group A |
Group B |
Total |
|
Survival |
Live |
78(94%) |
71(84.5%) |
149(89.2%) |
|
Dead |
5(6%) |
13(15.5%) |
18(10.8%) |
|
|
Total patients |
83(100%) |
84(100%) |
167(100%) |
|
|
P.value : 0.042 |
||||
A total of 18(10.8%) patients died during follow-up (table 2). Significantly more of these patients came from group B (13, 15.5%) compared to those in group A (5, 6%). With respect to the occurrence of other complications in the 2 groups, there were no significant differences (table 3).
Table 3: follow up outcomes. The incidence of complications grouped according to whether the initial hs-cTnT was above or below the median. PCI: percutaneous coronary intervention.
|
|
Group A |
Group B |
Total |
p value |
|
Heart Failure |
12(14.5%) |
14(16.7%) |
26(15.6%) |
0.429 |
|
Second PCI |
16(19.3%) |
15(17.9%) |
31(18.6%) |
0.485 |
|
Re-admission |
11(13.3%) |
9(10.7%) |
20(12.0%) |
0.395 |
|
Recurrent Chest pain |
12(14.5%) |
15(17.9%) |
27(16.2%) |
0.350 |
|
Other complications |
8(9.6%) |
10(11.9%) |
18(10.8%) |
0.412 |
This included other complications comprising stent thrombosis, renal failure, stroke and upper gastrointestinal tract bleeding.
In order to investigate whether there were any defining characteristics in the patients who died, a further analysis was carried out comparing the survived versus non survived groups. Table 4 shows the baseline clinical characteristics of patients in these 2 groups. Patients in the non survived group were older, more likely to be female, had more diabetes mellitus, more hypertension and a greater number of affected vessels. Smoking and infarct related artery were not significantly different between the two groups.
Table 4: clinical characteristics of patients according to survival status. The baseline clinical characteristics of all patients grouped according to whether they survived or not. Abbreviations as per table 1.
|
|
|
Survived |
Non survived |
Total |
p value |
|
Age categories |
20-39 year |
11(7.4%) |
1(5.6%) |
12(7.2%) |
<0.001 |
|
40-59 year |
74(49.7%) |
1(5.6%) |
75(44.9%) |
|
|
|
60-79 |
63(42.3%) |
13(72.2%) |
76(45.5%) |
|
|
|
80-90 |
1(0.7%) |
3(16.7%) |
4(2.4%) |
|
|
|
Gender |
Female |
30(20.1%) |
8(44.4%) |
38(22.8%) |
0.020 |
|
Male |
119(79.9%) |
10(55.6%) |
129(77.2%) |
|
|
|
DM |
|
40(26.8%) |
13(72.2%) |
53(31.7%) |
<0.001 |
|
HTN |
|
53(35.6%) |
11(61.1%) |
64(38.3%) |
0.035 |
|
Current Smoker |
|
55(36.9%) |
4(22.2%) |
59(35.3%) |
0.218 |
|
Infarct related artery |
LAD |
83(55.7%) |
9(50%) |
92(55.1%) |
0.379 |
|
RCA |
56(37.6%) |
9(50%) |
65(38.9%) |
|
|
|
LCX |
10(6.7%) |
0(0.0%) |
10(6.0%) |
|
|
|
No. of vessels affected |
Single vessel |
55(36.9%) |
0(0.0%) |
55(32.9%) |
0.005 |
|
Two vessels |
49(32.9%) |
8(44.4%) |
57(34.1%) |
|
|
|
Three vessels |
45(30.2%) |
10(55.6%) |
55(32.9%) |
|
At the follow up point the non survived group had more heart failure, more re-admissions, more recurrent chest pain and more of the other complications including complete heart block, renal impairment, reinfarction, stent thrombosis, and upper gastrointestinal tract bleeding compared to the survived group (table 5). There was no difference in the need for revascularization between the 2 groups.
Table 5: follow up outcomes in both groups according to survival status. The incidence of complications in patients grouped according to whether they survived or not. Abbreviation as per table 3.
|
|
Survived |
Non survived |
Total |
p value |
|
Heart Failure |
17(11.4%) |
9(50%) |
26(15.6%) |
< 0.001 |
|
Second PCI |
30(20.1%) |
1(5.6%) |
31(18.6%) |
0.133 |
|
Re-admission |
13(8.7%) |
7(38.9%) |
20(12%) |
<0.001 |
|
Recurrent Chest pain |
19(12.8%) |
8(44.4%) |
27(16.2%) |
<0.001 |
|
Other complications |
9 (6%) |
9(50%) |
18(10.8%) |
<0.001 |
Discussion
There are only a few studies that have assessed the prognostic value of cardiac troponins in patients with STEMI undergoing PPCI. Both admission and peak post-procedural values provide information on prognosis that can be incorporated into risk prediction scores. The advantages of using admission values is that these correlate more with the extent of spontaneous ischemic damage and are not subject to the interferences caused by the PPCI procedure or other treatment applied in the early stages of STEMI. Thus admission values can be preferred for inclusion in risk prediction scores[10].
This study demonstrates that patients with STEMI undergoing PPCI who have higher admission hs-cTnT levels had a higher risk of 2-year all-cause mortality. Although all patients presented early (within the first few hours of starting chest pain), which is reflected in the level of hs-cTnT, the more hs-cTnT the more time lapsed from symptoms, the more necrosis occurs, the more extensive and established the ischemic outcome. This study also observed that the non-survived group have higher levels of hs-cTnT than the survived group and were mostly older in age. This agrees with Ndrepepa et al.[10] who studied 818 patients with STEMI, treated by PPCI,with a 3 year follow up, who also found that the nonsurvivors were older in age and more likely to have type 2 diabetes, higher preprocedural and peak postprocedural hs-cTnT levels, lower estimated glomerular filtration rate and left ventricular function, but less likely to have a history of arterial hypertension or hypercholesterolemia. They concluded that admission or peak post procedural hs-cTnT is independently associated with higher 3 year mortality[10].
In the current study females have a greater risk of developing complications of MI,which is similar to Wijnbergen et al[22]. They found that mortality was higher and there was worse long term outcome after PPCI for STEMI in females. In addition, De Luca[23] studied 1548 patients of which 353 were women (22.8%) and showed that females tended to be more advanced in age, had higher prevalence of hypertension, diabetes, longer ischemia time, higher Killip class, smaller vessel caliber, and significantly higher 1-year mortality rate at univariate but not at multivariate analysis. This is also confirmed by van der Meer et al.,[24] in a systematic review of prognostic studies which showed a worse outcome in women with STEMI leading to the conclusion that mortality is higher in women with STEMI and can be explained by their unfavorable risk profile and longer symptom‐to‐ balloon time.
The current study observed that diabetic patients have higher levels of troponin on admission and higher mortality on follow up. Piccolo et al.,[25] conclude that diabetes in the ACS setting confers a worse prognosis with 1-year mortality >10% in both STEMI and non ST-elevation acute coronary syndrome[26]. also confirms that even with reperfusion, patients with STEMI and DM have greater long term mortality than do patients without DM.
In the baseline patient characteristics of Ndrepepa et al[10]., the number of current smokers was significantly lower in the non-survived group (15.6%) than in the survived group (38%). In this study also a higher mortality rate was observed in non-smoker than current smokers, although this was statistically insignificant, possibly due to a higher mean age in non-smokers (58.08 ± 10.47 years) than in current smokers (56.63 ± 12.22 years), together with the non-smoker group having more risk factors like diabetes mellitus and hypertension. Giannitsis et al[27]. who studied 140 patients with STEMI showed that higher levels of cTnT measured on admission were associated with poorer epicardial and tissue perfusion after PPCI. Velders et al[28]. showed that hs-cTnT, N-terminal probrain natriuretic peptide, extent of angiographic CAD, and growth differentiation factor-15 measured on admission predict the occurrence of subsequent cardiovascular death or MI compared with clinical information alone in STEMI patients reperfused by PPCI. Wang et al.[29] studied 173 STEMI patients undergoing PPCI and reported that the incidence of MACE (death, myocardial infarction and revascularization) at 30 days and 1 year were 10% and 18% respectively. They concluded that hs-cTnT measured on admission in patients with STEMI was strongly associated with 30 day and 1 year rates of major adverse events after PPCI[29].
Other outcomes of myocardial infarction were worse in the non-survived group than survived, such as heart failure, other complications (like reinfarction, stent thrombosis, stroke, renal impairment, and upper gastrointestinal tract bleeding), higher rates of recurrent chest pain, more readmissions, and increased need for further revascularizations. Although few patients developed these complications possibly due to small sample size, these were in agreement with the results of other studies that also showed higher rates of heart failure[30-31], renal failure[29,31], reinfarction and revascularizations[29] that were associated with higher baseline hs-cTnT levels, possibly reflecting an increase in the extent of myocardial necrosis and end-organ damage. According to these data there is a close association between hs-cTnT with baseline cardiovascular risk and the extent of myocardial damage in patients with STEMI and subsequent mortality. In the present study higher hs-cTnT was associated with higher mortality possibly due to higher risk profile like age, DM and multivessel coronary artery lesions.
Limitations
Contact with a lot of patients was lost during follow up. This led to a reduced sample size.
In this study the effect of different medications used following PCI was not investigated. This could have had a confounding effect. In addition dyslipidaemia was not measured in this study, which could also have had a confounding effect. Patients in group B were more likely to be hypertensive; however, no further analysis was carried out regarding the relationship between hypertension and hs-cTnT.
This is a small observational cohort study carried out in a single center; therefore the wider application of these results may be limited.
Conclusion
High initial hs-cTnT on admission is associated with a greater risk of mortality and morbidity at 2-year follow up in patients from Erbil City in Iraq with STEMI undergoing PPCI.
Acknowledgments
None
Conflicts of Interests
The authors report no conflicts of interests
Funding
None
References
- 1. Murray, C.J., Lopez, A.D. Mortality by cause for eight regions of the world: Global Burden of Disease Study. (1997) Lancet 349(9061): 1269-1276.
- 2. Crea, F., Liuzzo, G. Pathogenesis of acute coronary syndromes. (2013) J Am Coll Cardiology 61(1): 1-11.
- 3. Reimer, K.A., Lowe, J.E., Rasmussen, M.M., et al. The wavefront phenomenon of ischemic cell death. 1. Myocardial infarct size vs duration of coronary occlusion in dogs. (1977) Circulation 56(5): 786-794.
- 4. Newby, L.K., Jesse, R.L., Babb, J.D., et al. ACCF 2012 expert consensus document on practical clinical considerations in the interpretation of troponin elevations: a report of the American College of Cardiology Foundation task force on Clinical Expert Consensus Documents. (2012) J Am Coll Cardiol 60(23): 2427-2463.
- 5. Apple, F.S., Collinson, P.O. Analytical characteristics of high-sensitivity cardiac troponin assays. (2012) Clin Chem 58(1): 54-61.
- 6. Apple, F.S., Sandoval, Y., Jaffe, A.S., et al. Cardiac troponin assays: guide to understanding analytical characteristics and their impact on clinical care. (2017) Clin Chem 63(1): 73-81.
- 7. Cullen, L.A., Mills, N.L., Mahler, S., et al. Early rule-out and rule-in strategies for myocardial infarction. (2017) Clin Chem 63(1): 129-139.
- 8. Adams, J. E., Abendschein, D. R., Jaffe, A. S. Biochemical markers of myocardial injury. Is MB creatine kinase the choice for the 1990s? (1993) Circulation 88(2): 750-763.
- 9. Giannitsis, E., Kurz, K., Hallermayer, K, et al. Analytical validation of a high-sensitivity cardiac troponin T assay. (2010) Clin Chem 56(2): 254 -261.
- 10. Ndrepepa, G., Kufner, S., Hoyos, M., et al. High-sensitivity cardiac troponin T and prognosis in patients with ST-segment elevation myocardial infarction. (2018) J Cardiol 72(3): 220-226.
- 11. Bergmann, O., Bhardwaj, R.D., Bernard, S., et al. Evidence for cardiomyocyte renewal in humans. (2009) Science 324(5923): 98-102.
- 12. Ndrepepa, G., Braun, G., Mehilli, J., et al. Prognostic value of sensitive troponin T in patients with stable and unstable angina and undetectable conventional troponin. (2011) Am Heart J 161(1): 68-75.
- 13. Hallén, J., Buser, P., Schwitter, J., et al. Relation of cardiac troponin I measurements at 24 and 48 hours to magnetic resonance–determined infarct size in patients with ST-elevation myocardial infarction. (2009) Am J Cardiol 104(11): 1472-1477.
- 14. Burns, R.J., Gibbons, R.J., Yi, Q., et al. The relationships of left ventricular ejection fraction, end-systolic volume index and infarct size to six-month mortality after hospital discharge following myocardial infarction treated by thrombolysis. (2002) J Am Coll Cardiol 39(1): 30-36.
- 15. Pride, Y.B., Mohanavelu, S., Zorkun, C., et al. Association between angiographic complications and clinical outcomes among patients with acute coronary syndrome undergoing percutaneous coronary intervention: an EARLY ACS (early glycoprotein IIb/IIIa Inhibition in non–ST-segment elevation acute coronary syndrome) angiographic substudy. (2012) JACC: Cardiovasc Interv 5(9): 927-935.
- 16. Thygesen, K., Albert, J.S., Jaffe, A.S., et al. Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol 72(18): 2231-2264.
- 17. Williams, B., Mancia, G., Spiering, W., et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. (2018) Eur Heart J 39(33): 3021-3104.
- 18. American Diabetes Association. Diagnosis and classification of diabetes mellitus. (2010) Diab Care 33(1): S62-S69.
- 19. McKee, P.A., Castelli, W.P., McNamara, P.M., et al. The natural histroy of congestive heart failure: The Framingham study. (1971) N Engl J Med 285(26): 1441-1446.
- 20. Kerensky, R.A., Wade, M., Deedwania, P., et al. Veterans Affairs Non-Q-Wave Infarction Stategies in-Hospital (VANQWISH) Trial Investigators. Revisiting the culprit lesion in non–Q-wave myocardial infarction: results from the VANQWISH trial angiographic core laboratory. (2002) J Am Coll Cardiol 39(9): 1456-1463.
- 21. Shaikh, A.H., Siddiqui, M.S., Hanif, B., et al. Outcomes of primary percutaneous coronary intervention (PCI) in a tertiary care cardiac centre. (2009) J Pak Med Assoc 59(7): 426-429.
Pubmed| Crossref| Others
- 22. Wijnbergen, I., Tijssen, J., van’t, V.M., et al. Gender differences in long‐term outcome after primary percutaneous intervention for ST‐segment elevation myocardial infarction. (2013) Catheter Cardiovasc Interv 82(3): 379-384.
- 23. De Luca, G., Suryapranata, H., Dambrink, J.H., et al. Sex-related differences in outcome after ST-segment elevation myocardial infarction treated by primary angioplasty: data from the Zwolle Myocardial Infarction study. (2004) Am Heart J 148(5): 852-856.
- 24. van der Meer, M.G., Nathoe, H.M., van der Graaf, Y., et al. Worse outcome in women with STEMI: a systematic review of prognostic studies. (2015) Eur J Clin Invest 45(2): 226-235.
- 25. Piccolo, R., Franzone, A., Koskinas, K.C., et al. Effect of diabetes mellitus on frequency of adverse events in patients with acute coronary syndromes undergoing percutaneous coronary intervention. (2016) Am J Cardiol 118(3): 345-352.
- 26. van der Schaaf, R.J., Henriques, J.P.S., Wiersma, J.J., et al. Primary percutaneous coronary intervention for patients with acute ST elevation myocardial infarction with and without diabetes mellitus. (2006) Heart 92(1): 117-118.
- 27. Giannitsis, E., Müller-Bardorff, M., Lehrke, S., et al. Admission troponin T level predicts clinical outcomes, TIMI flow, and myocardial tissue perfusion after primary percutaneous intervention for acute ST-segment elevation myocardial infarction. (2001) Circulation 104(6): 630-635.
- 28. Velders, M. A., Wallentin, L., Becker, R. C., et al. Biomarkers for risk stratification of patients with ST-elevation myocardial infarction treated with primary percutaneous coronary intervention: Insights from the Platelet Inhibition and Patient Outcomes trial. (2015) Am Heart J 169(6): 879-889.
- 29. Wang TKM, Snow TA, Chen Y, et al. High-sensitivity troponin level pre-catheterization predicts adverse cardiovascular outcomes after primary angioplasty for ST-elevation myocardial infarction. Eur Heart J Acute Cardiovasc Care 2014; 3:118-125.
Pubmed| Crossref| Others
- 30. Riddell, T. Heart failure hospitalisations and deaths in New Zealand: patterns by deprivation and ethnicity. (2004) N Z Med J 118(1208): U1254.
- 31. Joshy, G., Dunn, P., Fisher, M., et al. Ethnic differences in the natural progression of nephropathy among diabetes patients in New Zealand: hospital admission rate for renal complications, and incidence of end-stage renal disease and renal death. (2009) Diabetologia 52(8): 1474-1478.