Viable Live Birth in a Non Communicating Rudimentary Horn of Uterus: A Case Report
Manupriya Sharma1, Anjali Soni2, Suresh Verma2, Chanderdeep Sharma2*, Pawan Kumar Soni3
Affiliation
Chanderdeep Sharma, Department of Obstetrics and Gynecology, Dr. Rajendra Prasad Government Medical College, Kangra, Himachal Pradesh 176001, India, Tel: 91-9218925471; E-mail: cdsharma2006@gmail.com
Corresponding Author
Chanderdeep Sharma, Department of Obstetrics and Gynecology, Dr. Rajendra Prasad Government Medical College, Kangra, Himachal Pradesh 176001, India, Tel: 91-9218925471; E-mail: cdsharma2006@gmail.com
Citation
Sharma, C., et al. Pelvic Viable Live Birth in a non Communicating Rudimentary Horn of Uterus: a Case Report. (2016) J Gynecol Neonatal Biol 2(1): 17-19.
Copy rights
© 2016 Sharma, C. This is an Open access article distributed under the terms of Creative Commons Attribution 4.0 International License.
Keywords
Non communicating rudimentary horn of pregnancy; Viable live birth
Abstract
Background: Pregnancy in non communicating rudimentary horn of uterus is an extremely rare event at an estimated incidence of 1 per 100,000 to 140,000 pregnancies. Usually it is followed by rupture of uterus in first or second trimester of pregnancy.
Case: We are reporting a case of a multi parous women (with previous normal vaginal delivery), at 37 weeks gestation. She had a term pregnancy in non communicating rudimentary horn of uterus. She underwent cesarean section followed by excision of rudimentary horn and ipsilateral salpingectomy.
Summary and conclusion: Viable live birth resulting from pregnancy in a non communicating rudimentary horn of uterus is a very rare phenomenon. A high index of suspicion should be kept in mind especially in pregnant women with multiple failed attempts of Medical Termination of Pregnancy (MTP), fetal malpresentation, fetal growth restriction, abnormal placentation or failure of induction for termination of pregnancy.
Introduction
Pregnancy in non communicating rudimentary horn of uterus is an extremely rare event and is classified as an ectopic pregnancy[1]. Rupture of uterus is usually seen in first or second trimester of pregnancy[1]. We hereby report a case of such a pregnancy which not only continued to third trimester but also resulted in delivery of a live viable neonate.
Case Report
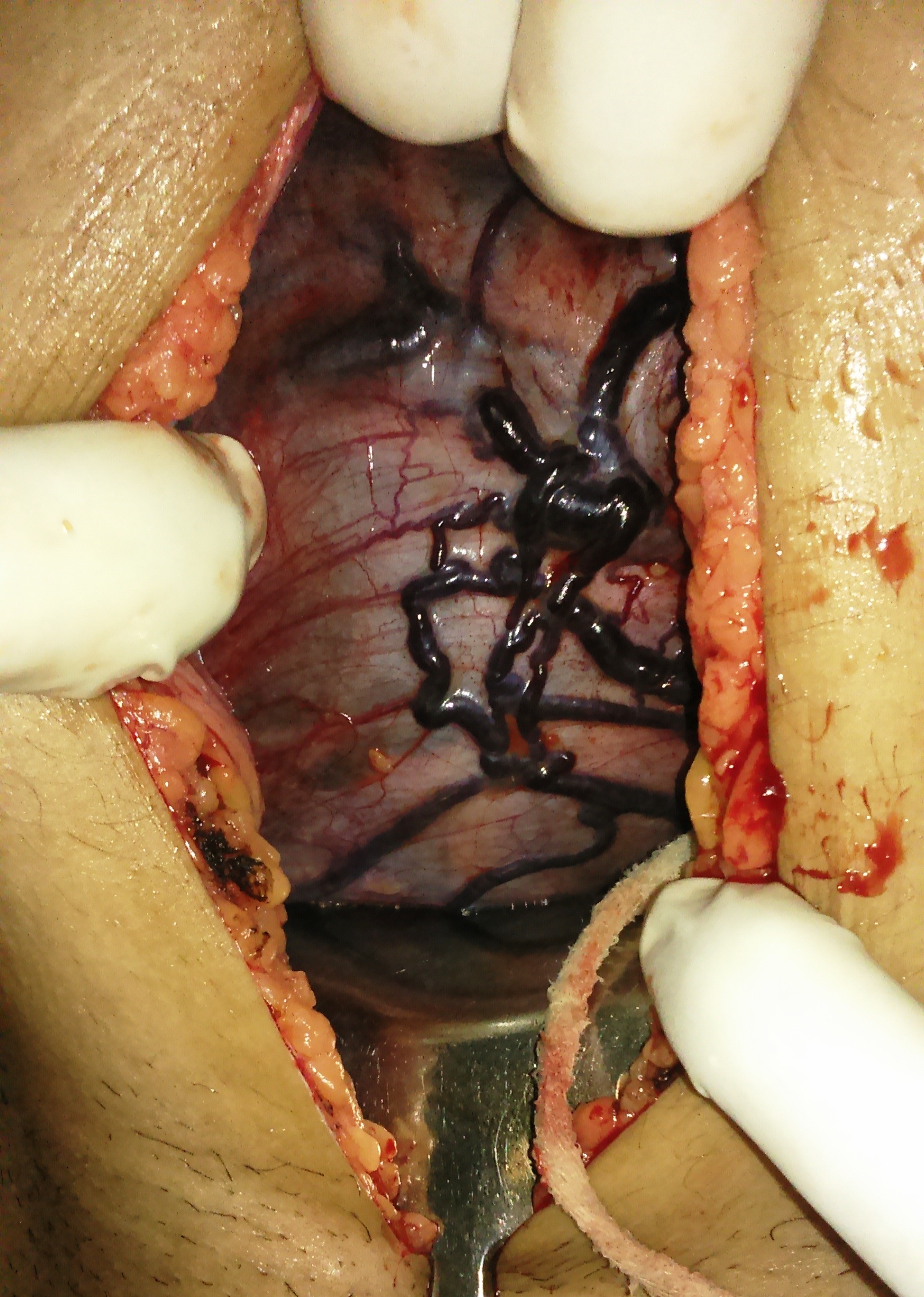
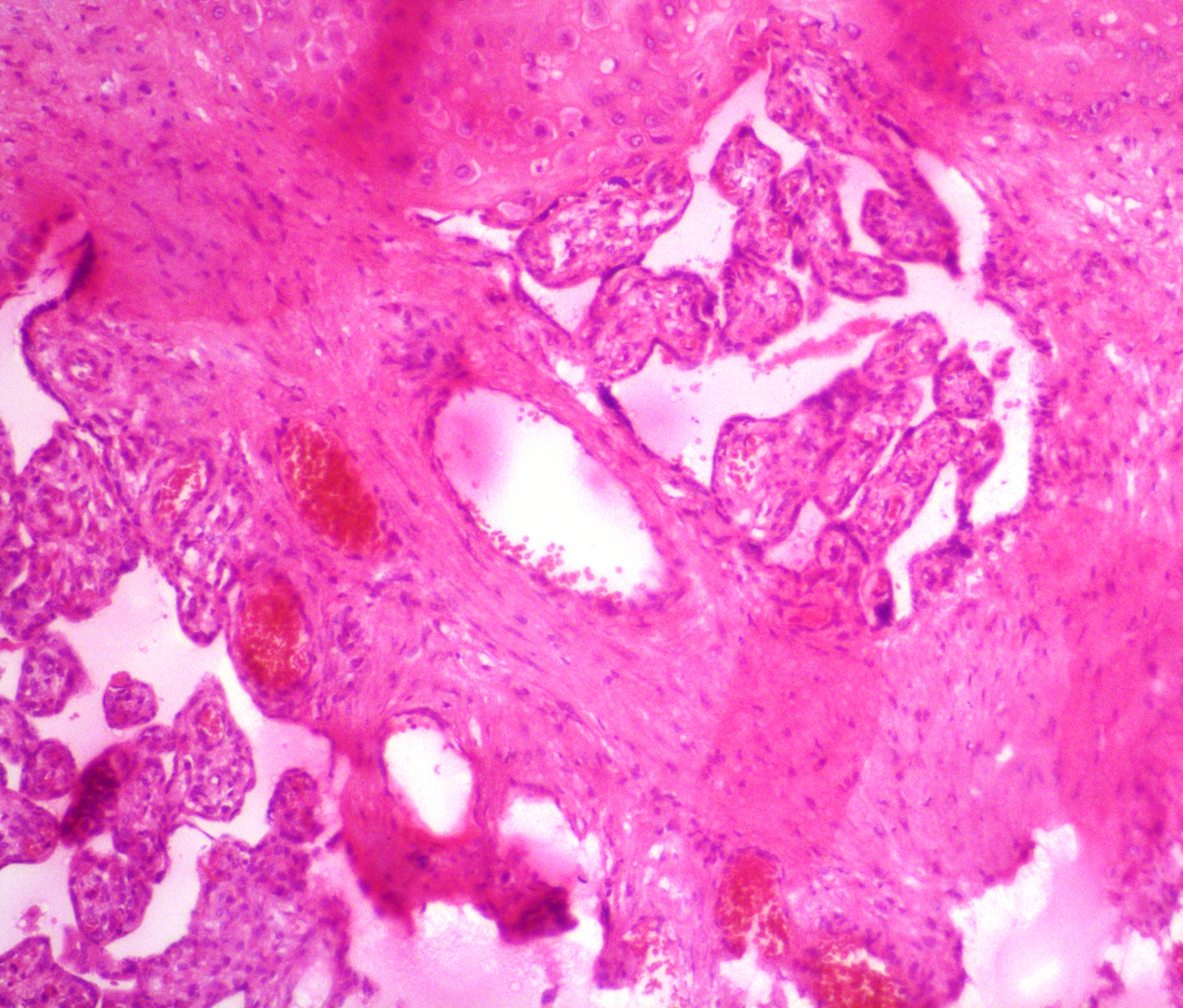
A 22-year-old gravida 2 para 1, with previous uneventful normal vaginal delivery, presented to the labor room at 37 weeks gestation. This was an unplanned pregnancy and she had taken oral abortifacients (mifepristone 200 mg followed by misoprostol 400 μg 48 hours later) twice for Medical Termination of Pregnancy (MTP) in first and second trimester of pregnancy. She was subsequently advised surgical evacuation of uterus which could not be done due to some domestic family dispute. She was lost to follow up due to domestic family dispute. Her antenatal period (otherwise) was uneventful. She reported in labor in third trimester (hence early diagnosis was not available). On examination the height of the uterus corresponded to 32 weeks gestation. She was in labor. The fetus was in breech presentation. On pelvic examination, cervix was deviated to left side. Cervical os was closed and minimally effaced. A firm, round mass around 8*8 cms was felt on right side. Ultrasound showed a fetus of 32 weeks gestation with an empty horn of uterus lying on right side. There was a single cervix. There was no history of severe dysmennorhoea or cryptomennorhoea. So a provisional diagnosis of mullerian anomaly of either bicornuate uterus (complete) or a unicornuate uterus (with a communicating horn) was suspected. After informed consent, emergency cesarean section was done in view of breech presentation with intra uterine growth restricted fetus. Infra umbilical midline vertical incision was given on anterior abdominal wall. Intra-operatively, the horrendous picture of abnormal vessels over the uterus was seen (Figure 1). There was a horn of uterus on right side and pregnancy was in left side horn of uterus. She delivered a healthy female neonate weighing 1900 grams. After delivery of the fetus it was found that there was no communication between the cervix and horn of uterus (which was having fetus). Hence a diagnosis of unicornuate uterus with non communicating horn with pregnancy in non communicating horn was confirmed. Additionally, there was abnormal morbid adherence of placenta. Rudimentary horn of uterus with placenta in situ was excised (Figure 2). Subsequently, she had an uneventful recovery. Ultrasound of kidneys revealed no congenital anomaly. Mother and neonate were discharged in healthy condition on day 7 post operatively. Histopathology examination of excised horn of uterus confirmed non communicating horn of uterus with morbid adherent placenta (placenta accreta) (Figure 3). Mother and baby were doing well at 6-week follow-up at the outpatient department.
Figure 1: Horrendous picture of rudimentary horn with extensive vessels after giving skin incision.
Figure 2: Excised rudimentary horn of uterus with placenta in situ.
Figure 3: Histopathological examination confirming morbid adherent placenta.
Discussion
Pregnancy in a non communicating rudimentary horn of uterus occurs at an estimated incidence of 1 per 100,000 to 140,000 pregnancies[1]. Out of these, the chances of reaching term gestation are only 10% and chances of neonate survival are only 2%. Pregnancy can only occur in a non communicating rudimentary horn of uterus by transperitoneal migration of spermatozoa or a fertilized ovum through contra lateral tube[2]. As the rudimentary horn of uterus is not directly connected to cervix or vagina, hence the only logical explanation of implantation in this site is by trans-peritoneal migration of sperm i.e. sperm ascends via vagina, cervix, normal hemi-uterus, contra-laterla fallopian tube, peritoneum, then ipsilateral fallopian tube (where fertilization occurs) and finally implantation of fertilized ovum in rudimentary horn of uterus[3]. Usually these pregnancies terminate by spontaneous rupture of non communicating rudimentary horn of uterus in first or second trimester of pregnancy[4]. Rarely do they reach third trimester of pregnancy.
Due to smaller volume and reduced distension of rudimentary horn of uterus[4], intra uterine growth restriction, oligo-hydramnios and mal presentation are common features (as seen in index case). Also in cases with non functional rudimentary horn of uterus as there is no functional endometrium so the placentation is almost invariably morbid adherent placenta (as seen in index case).
Mullerian anomalies are usually diagnosed during cesarean section. However, early diagnosis can be suspected in cases of deviated uterus with palpable adenexal mass (as seen in index case), or a mass extending outside the uterine angle (Baart de la faille’s sign) or rotation of uterus to opposite side with elevation of horn of uterus (Ruge Simnn Syndrome)[1]. Multiple failed attempts at termination of pregnancy have been proposed as a significant risk factor for obstructive mullerian anomalies. Ultrasonography and magnetic resonance imaging has made early diagnosis possible even in first trimester of pregnancy. In our case, the recognition of a rudimentary horn pregnancy was suspected on basis of history (failed MTP after repeated oral abortifacients), clinical examination (deviated uterus with an adenexal mass in contra lateral side and malpresentation of fetus) and ultrasonography.
The management of pregnancy in non communicating rudimentary horn of uterus is primarily excision of rudimentary horn along with ipsilateral salpingectomy (to prevent ectopic pregnancy subsequently). Rarely, hysterectomy may be required in cases with severe post partum hemorrhage. Recently, some reports of laparoscopic excision of rudimentary horn of uterus have also been reported[5,6].
Pregnancy in a non communicating uterine horn resulting in delivery of a live newborn is an extremely rare event. Due to variable myometrial thickness, reduced distension of uterine cavity and morbid adherence of placenta, rupture of rudimentary horn can occur at any period of gestation, more likely in first or second trimester of pregnancy[4]. Our patient was fortunate enough that this catastrophic event (rupture of uterus) did not occur even after spontaneous onset of labor.
Renal anomalies are also commonly associated with unicornuate uterus (20%)[1]. Investigations to rule out urinary anomalies are fundamental in these patients. Our patient incidentally had no such anomaly. Also patient should be advised regarding the increased risk of preterm labor and malpresentation in next pregnancies due to unicornuate uterus.
Pregnancy in rudimentary horn of uterus is classified as an ectopic pregnancy and carries grave fetal and maternal prognosis if early diagnosis is not made. Ante natal diagnosis is extremely difficult and usually made during surgery/laparotomy. Hence, there should be high index of suspicion among managing obstetricians especially in cases with multiple failed attempts of MTP, fetal malpresentation, fetal growth restriction, abnormal placentation or failure of induction for termination of pregnancy.
Conflict of Interest:
There is no conflict of interest with any individual or organization
References
- 1. Chopra, S., Keepanasseril, A., Rohilla, M., et al. Obstetric morbidity and the diagnostic dilemma in pregnancy in rudimentary horn: retrospective analysis. (2009) Arch Gynecol Obstet 280(6): 907–910.
- 2. Gonçalves, E., Prata, J.P., Ferreira, S., et al. An unexpected near term pregnancy in a rudimentary uterine horn. (2013) Case Rep Obstet Gynecol.
- 3. Nahum, G.G., Stanislaw, H., McMahon, C. Preventing ectopic pregnancies: how often does transperitoneal transmigration of sperm occur in effecting human pregnancy? (2004) BJOG 111(7): 706-714.
- 4. Kanagal, D.V., Hanumanalu, L.C. Ruptured rudimentary horn pregnancy at 25 weeks with previous vaginal delivery: a case report. (2013) Case Rep Obstet Gynecol.
- 5. Shahid, A., Olowu, O., Kandasamy, G., et al. Laparoscopic management of a 16-week ruptured rudimentary horn pregnancy: a case and literature review. (2010) Arch Gynecol Obstet 282(2): 121-125.
- 6. Contreras, K.R., Rothenberg, J.M., Kominiarek, M.A., et al. Hand-assisted laparoscopic management of a midtrimester rudimentary horn pregnancy with placenta increta: a case report and literature review. (2008) J Minim Invasive Gynecol 15(5): 644-648.